This article has been
cited by other articles in ScienceCentral.
Abstract
This case report describes a traumatic pseudoaneurysm arising from the right V4 segment of the vertebral artery, near the origin of the posterior inferior cerebellar artery. Post-traumatic vertebral artery pseudoaneurysm is rare, but associated with a high mortality rate. We report on an extremely rare case of post-traumatic pseudoaneurysm of the vertebral artery with delayed manifestation. A 9-year-old child was admitted to the emergency room after a pedestrian car accident. A computed tomography (CT) scan showed subarachnoid hemorrhage with intraventricular hemorrhage (IVH), multiple facial bones, and temporal bone fracture. External ventricular drainage and decompressive suboccipital craniectomy were performed for acute hydrocephalus and posterior fossa swelling. The patient's clinical condition became suddenly aggravated on the 15th hospital day, and brain CT confirmed appearance of a new 4th ventricle IVH. Digital subtraction angiography revealed a ruptured pseudoaneurysm arising from the right V4 segment of the vertebral artery. Parent artery occlusion using detachable coils was achieved. Despite intensive care, the patient's clinical condition showed continuous deterioration and the patient died of respiratory complications on the 52nd hospital day.
Go to :

Keywords: Craniocerebral trauma, Subarachnoid hemorrhage, Aneurysm, false, Vertebral artery
Introduction
Traumatic intracranial pseudoaneurysm is a rare condition, accounting for less than 1% of all aneurysms.
7) Of these, post-traumatic vertebral artery pseudoaneurysm is not well known, because the incidence of isolated trauma to the vertebral artery is extremely low. Majidi et al.
4) reported that incidence of vertebral artery dissection was 0.01% of patients with head and neck trauma. Traumatic pseudoaneurysm ruptures are associated with a high mortality rate, because of high risk of rebleeding or regrowth. We report on a rare case of post-traumatic pseudoaneurysm arising from the right V4 segment of the vertebral artery.
Go to :

Case Report
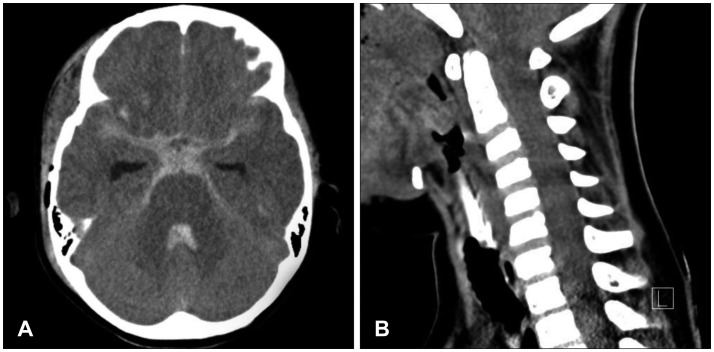
A 9-year-old child was admitted to the emergency room after a pedestrian car accident. On admission, his mentality was stupor and Glasgow Coma Scale score was 9. Motor power of all extremities showed a good grade but movement showed abnormal flexion in response to painful stimuli. Brain computed tomography (CT) showed subarachnoid hemorrhage (SAH) with intraventricular hemorrhage (IVH), multiple facial bones, and temporal bone fracture (
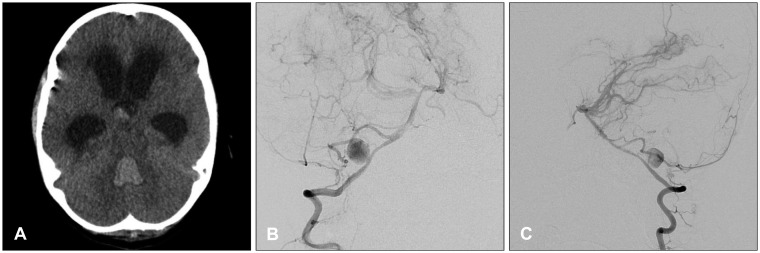
Figure 1). A cervical spine CT showed no abnormal findings. External ventricular drainage and suboccipital craniectomy were performed for acute hydrocephalus and decompression of posterior fossa swelling. Follow-up CT demonstrated resolution of the hemorrhage and his clinical condition recovered to stupor mentality. On the 15th hospital day, the patient showed decreased mentality into semicoma and CT scan revealed the onset of a new 3rd, 4th ventricle hemorrhage and aggravation of hydrocephalus. CT angiography and digital subtraction angiography confirmed a pseudoaneurysm measuring approximately 15 mm in size arising from the right V4 segment of the vertebral artery, near the origin of the posterior inferior cerebellar artery (PICA) (
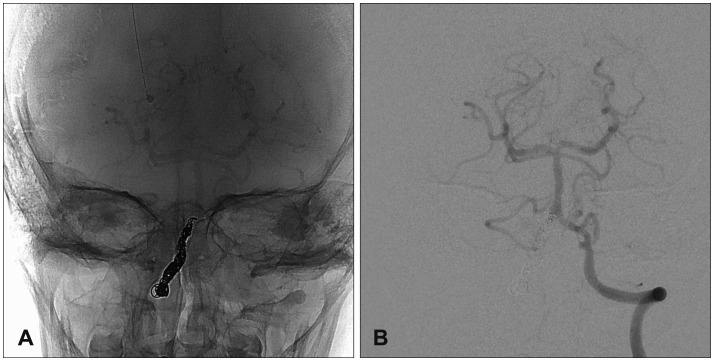
Figure 2). The dominancy of the vertebral artery was even in size and blood flow to the right PICA territory was supplied from the right anterior inferior cerebellar artery (AICA), meaning the AICA-PICA complex (
Figure 3). Therefore, we decided to occlude the parent artery for complete obliteration of the pseudoaneurysm. Final angiography confirmed complete obliteration of the pseudoaneurysm with preservation of the right AICA-PICA complex (
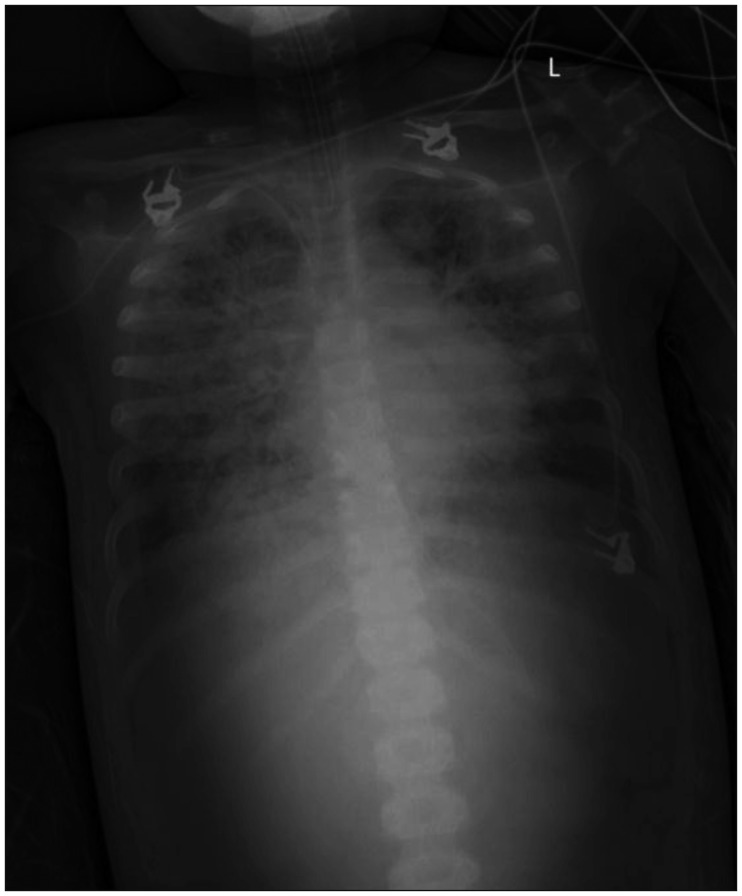
Figure 4). After endovascular treatment, the patient did not show worsening of neurological condition. Despite receiving intensive neurosurgical care, he died of acute respiratory distress syndrome on the 52nd hospital day (
Figure 5).
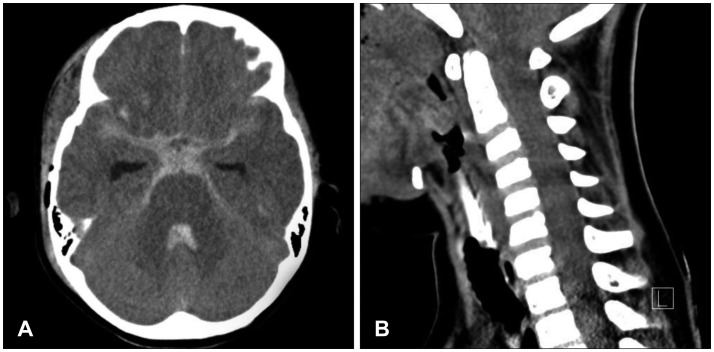 | FIGURE 1Initial non-contrast computed tomography (CT) showing subarachonoid hemorrhage around pons, both Sylvian fissures, and basal cistern (A). No abnormality was observed on cervical spine CT (B).
|
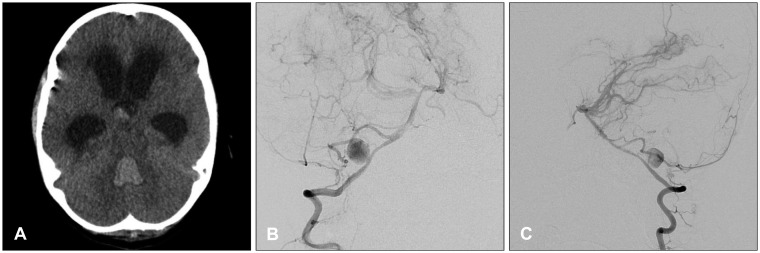 | FIGURE 2Follow-up computed tomography (CT) and digital subtraction angiography (DSA). A: Follow-up brain CT confirming increased 4th ventricle hemorrhage and hydrocephalus. B, C: DSA demonstrating a pseudoaneurysm arising from the right V4 segment of the vertebral artery, near the origin of the posterior inferior cerebellar artery.
|
 | FIGURE 3Computed tomography angiography showing a saccular lesion at the right distal vertebral artery and similar size of both vertebral arteries.
|
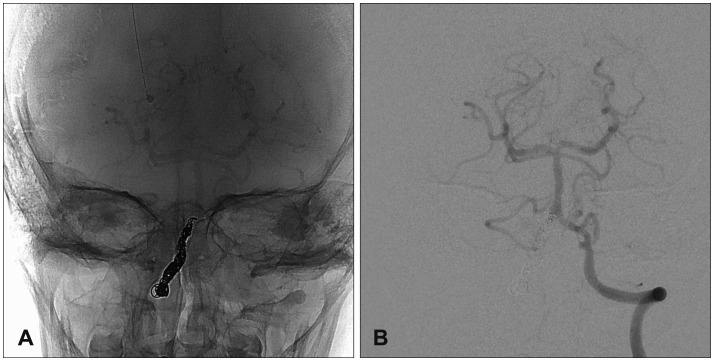 | FIGURE 4A: Post-procedural unsubtracted image reveals complete obliteration of the right distal vertebral artery including pseudoaneurysm. B: Left vertebral artery angiography confirms sufficient collateral flow of the right cerebellar hemisphere.
|
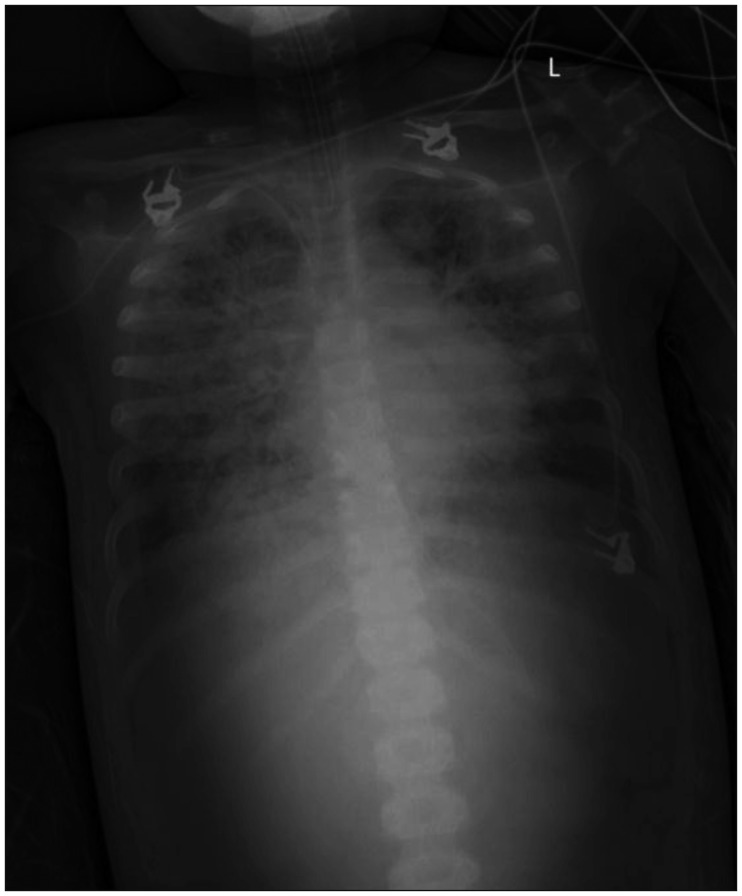 | FIGURE 5Chest X-ray showing haziness of both lung fields.
|
Go to :

Discussion
Development of traumatic intracranial pseudoaneurysms occurs after blunt or penetrating head and neck trauma. The mechanism is direct vessel injury from the foreign body or bony fragments due to skull fracture, or vascular torsion, stretching, and pressure against adjacent structures. The location of these pseudoaneurysms is varied, and they are commonly found in the anterior circulation. However, pseudoaneurysms of the vertebral artery are uncommon. Biffl et al.
2) reported that vertebral artery injuries are presented in 0.5% of blunt cervical traumas. Detection of traumatic pseudoaneurysms is still a clinical challenge due to its diverse presentation and lack of widely accepted diagnosis and management guidelines.
5) Clinical manifestation of vertebral pseudoaneurysm rupture could be a local neck mass, or neurologic symptoms related to posterior circulation due to microembolization. These pseudoaneurysms carry significant risk of embolic stroke and mortality, with cited figures of 13%, respectively.
13) However, some pseudoaneurysms of the vertebral artery, like V3 or V4 segment, which proceeds from C1 to a junction with the contralateral vertebral artery, could present with intracranial hemorrhage.
In general, deterioration of traumatic pseudoaneurysms may occur within several weeks after initial trauma. After the formation of a pseudoaneurysm, sudden onset of rebleeding could be associated with increased intracranial pressure or clot lysis. Traumatic pseudoaneurysm could only be definitively diagnosed by angiography. The pseudoaneurysms might be safely observed because spontaneous thrombosis could occur, but rebleeding could sometimes occur.
6) Therefore, early diagnosis and proper treatment of a pseudoaneurysm is also mandatory and highly important. Treatment should also be determined individually. Recently, endovascular treatment has been widely used in the treatment of traumatic aneurysms. Intervention could also be an effective method for management of pseudoaneurysm, particularly posterior circulation with poor clinical grade.
In the current case, the patient presented with post-traumatic SAH and IVH, which was mistaken for simple traumatic SAH, and there was no initial evaluation for vascular injury. However, we should have suspected pseudoaneurysm formation in this situation. Formation of a pseudoaneurysm should be suspected in patients with trauma, if there is thick SAH accompanying a basal skull fracture. The mechanism of traumatic brain injury is also an important consideration for development of pseudoaneurysm. Severe head trauma causing SAH could be causes of traumatic pseudoaneurysm formation.
On the 15th hospital day with deterioration of level of consciousness, angiography confirmed a rupture of a pseudoaneurysm arising from the right V4 segment of the vertebral artery. At the time of admission, there was no cervical spine injury that could affect dynamic injury to the vertebral artery. The trauma mechanism was complex. The child was pushed by a reversing school minivan with very low velocity immediately after leaving his car. Then, he fell down and was run over by the right rear wheel. Therefore, the exact mechanism of vascular injury is ambiguous; however, considering angiographic findings, we thought that pseudoaneurysm formation was due to the rupture of a perforating artery by traction injury or dissection. The definite treatment of traumatic pseudoaneurysm is a destructive method, meaning parent artery occlusion. We could occlude the right vertebral artery just proximal to the AICA origin, because there was no visualization on initial angiography and non-dominant vertebral artery compared with the contralateral side.
Go to :

Conclusion
We report an extremely rare case of traumatic pseudoaneurysm rebleeding arising from the intracranial vertebral artery. Post-traumatic intracranial pseudoaneurysm should be considered in any patient who exhibits neurological deterioration after head trauma. Therefore, brain CT angiography is mandatory for evaluation of vascular injuries in patients with traumatic SAH and for achievement of a better outcome, especially in cases showing thick SAH around the brain stem or SAH with accompanying basal skull fractures.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download