This article has been
cited by other articles in ScienceCentral.
Abstract
Dural arteriovenous fistulas (AVFs) are uncommon, representing only 10% to 15% of all intracranial AVFs. Here we present the case of a patient with cerebral infarction who experienced a dural AVF after craniotomy for superficial temporal artery (STA) to middle cerebral artery (MCA) bypass surgery. A 48-year-old man presented with dysarthria and right side hemiparesis. A brain magnetic resonance imaging scan revealed multiple acute infarctions and severe stenosis of the left MCA. Therefore, STA-MCA bypass surgery was performed. A follow-up angiography performed 2 weeks after the surgery showed an abnormal vascular channel from the left middle meningeal artery (MMA) to the middle meningeal vein (MMV) just anterior to the border of the craniotomy margin. This fistula originated from a screw used for cranial fixation. The screw injured the MMA and MMV, and this resulted in the formation of a fistula. The fistula was successfully treated with transarterial embolization. Surgeons should be careful when fixing bones with screws and plates as fistulas can develop if vessels are injured.
Go to :

Keywords: Central nervous system vascular malformations, Cerebral revascularization, Meningeal arteries, Middle cerebral artery
Introduction
Dural arteriovenous fistulas (AVFs) are uncommon, representing only 10% to 15% of all intracranial AVFs.
5) AVFs are classified into the following two major groups: congenital and acquired. Acquired AVFs caused by sinus occlusion, trauma, or iatrogenic injury after craniotomy or ventriculostomy have been reported.
7) Injury to the dural vessels resulting from penetrating head trauma skull fractures, especially in the region crossing the meningeal grooves, has been reported to cause an AVF.
6) Here we present the case of a patient with cerebral infarction who experienced a dural AVF after craniotomy for superficial temporal artery (STA) to middle cerebral artery (MCA) bypass surgery.
Go to :

Case Report
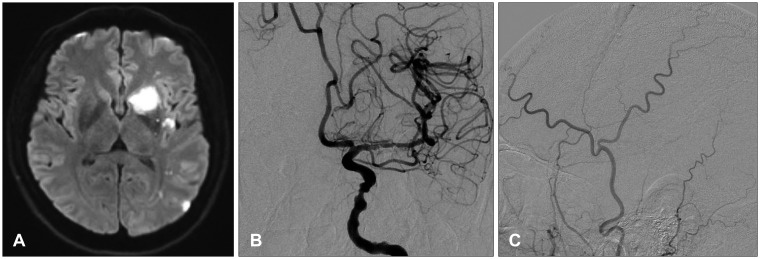
A 48-year-old man presented with dysarthria and right side hemiparesis. A brain magnetic resonance imaging scan revealed multiple acute infarctions in left basal ganglia and frontoparietal lobe, and severe stenosis of the left MCA. Angiography showed severe focal stenosis of the left M1 and perfusion delay of the MCA territory (
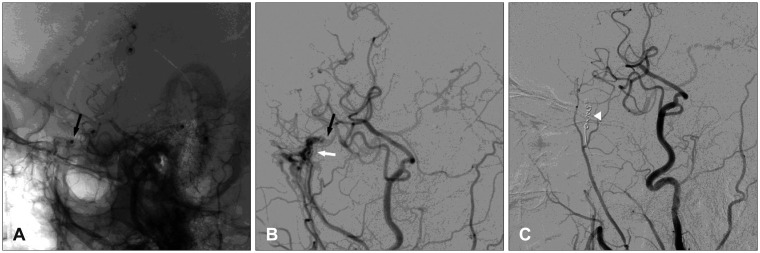
Figure 1). Therefore, STA-MCA bypass surgery was performed. His condition gradually improved, and follow-up angiography was performed 2 weeks after surgery. Selective angiography of the left extracranial artery (ECA) demonstrated an abnormal vascular channel from the left middle meningeal artery (MMA) to the middle meningeal vein (MMV) just anterior to the border of the craniotomy margin. This fistula originated from the site of a screw used for cranial fixation. The screw injured the MMA and MMV, and this resulted in the formation of a fistula. Although he had no fistula-related symptoms, the abnormal blood flow from the MMA influenced the STA-MCA bypass flow. Therefore, the lesion was occluded with coil embolization (
Figure 2). Using a guiding catheter in the ECA trunk, a microcatheter was navigated into the MMA, and then, detachable and pushable coils were inserted into the MMA. Angiography performed after the procedure showed complete occlusion of the fistula. He was discharged after coil embolization, and he is being followed up in the outpatient clinic.
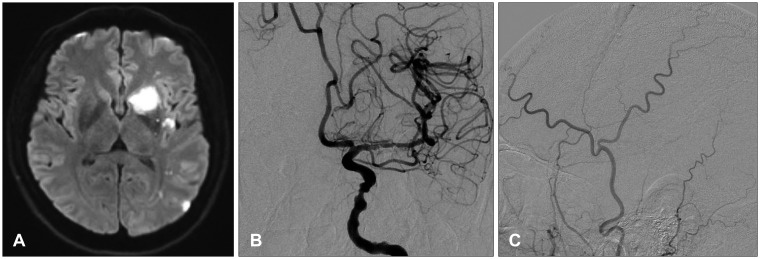 | FIGURE 1A: Diffusion-weighted magnetic resonance imaging revealed multiple acute infarctions in left basal ganglia and frontoparietal lobe. B: Preoperative anteroposterior angiogram of the left internal carotid artery demonstrating severe stenosis of the left middle cerebral artery. C: Preoperative lateral angiogram of the left external carotid artery demonstrating no evidence of a dural arteriovenous fistula.
|
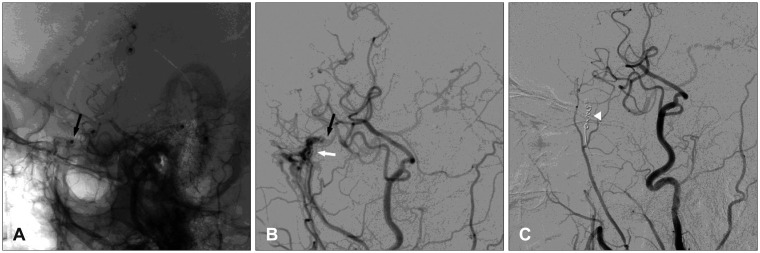 | FIGURE 2A: Lateral angiogram of the left external carotid artery obtained 2 weeks after superficial temporal artery to middle cerebral artery anastomosis demonstrating the craniotomy site and the screw (black arrow). B: The arteriovenous fistula from the middle meningeal artery (B, white arrow) caused by the screw (black arrow, same point as that in A). C: Transarterial coil embolization is performed (white arrowhead).
|
Go to :

Discussion
Dural AVFs represent only 10% to 15% of all intracranial AVFs.
1) Although the causes of dural AVFs remain uncertain, dural sinus thrombosis and venous thrombosis are important in the pathogenesis of dural AVFs.
2358) Another possible cause is iatrogenic injury. An iatrogenic dural AVF is most commonly found after intracranial surgery. Several dural AVF cases have been reported after burr-hole procedure, ventriculostomy, craniotomy, and craniectomy. Pappas et al.
6) reported recurrent subdural hematomas caused by a dural AVF after burr-hole drainage. Their patient had a chronic subdural hematoma. They performed burr-hole drainage; however, new acute subdural hematoma occurred at the burr-hole site. Angiography revealed a dural AVF adjoin the burr-hole made in the previous operative procedure. They performed craniotomy with extended bone flap and coagulation of a dural AVF.
Trauma to the MMA, especially in the part of the groove at the internal side of the cranium, can cause a dural AVF. Inagawa et al.
4) reported the case of a middle meningeal fistula caused by a head fixation device (Mayfield-Kees) that was used to stabilize the head during surgery for an aneurysm. Angiography after surgery revealed an AVF from the MMA to the pterygoid venous plexus.
Anatomical studies have shown that two meningeal veins usually accompany the MMA and its major branches.
6) Interestingly, the meningeal grooves are mainly occupied by the veins, in compared with the artery. This anatomic connection may elucidate the high frequency of traumatic fistulas, and result in the typical angiography finding of this location, named as "tram tracks".
6) A tear in the arterial wall from skull fracture can cause a MMA fistula.
2) Similarly, iatrogenic injury of the MMA can cause a dural AVF. In our case, a fixation screw injured the MMA. Angiography showed that the dural AVF originated from the screw tip, and on computed tomography, the screw tip was identified in the middle meningeal groove.
This dural AVF caused by screw fixation is unique, and it required surgery or endovascular treatment. A dural AVF can change the cerebral perfusion and flow dynamics, which can aggravate acute infarction associated with STA-MCA anastomosis.
7)
Go to :

Conclusion
We presented the rare case of a patient with cerebral infarction who experienced a dural AVF after craniotomy for STA-MCA bypass surgery. When performing craniotomy using screw fixation, it is important to avoid injuring the middle meningeal groove. Additionally, surgeons should be careful when fixing bones with screws and plates as fistulas can develop if vessels are injured. We suggest early intracranial embolization for a dural AVF after STA-MCA anastomosis to prevent further cerebral blood flow compromise.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download