Abstract
Objective
In June 28, 2012, a 'Hospitalization guideline for car accident patients' was announced to mediate the clash of opinions about the hospitalization of minor head trauma patients among doctors, patients and insurance companies. The guideline was issued to describe the patients' symptoms and emotions in detail after the injury. In this paper, evaluation for the guideline and suggestions for modifications was done.
Methods
Thirty-two doctors, 96 patients and 60 employees were each given surveys about the hospitalization guidelines, related personnels' attitude and evaluation of patients' emotional problems. The frequency, ratio and chi-square test were performed.
Results
Sixty-eight point eight percent of doctors, 79.8% patients and 91.6% insurance company employees agreed to the need for a guideline. Among the 68.8% doctors that supported the need for a guideline, 18.8% knew that the guideline actually existed. Sixty-nine point two percent of doctors said that they would apply the guideline once they were introduced to it. Among the announced guideline provisions, 'Glasgow coma score less than 15' and 'socially not suitable for discharge' required reevaluation since 40.6% all surveyors consented that these two criteria were not suitable. The consensus supporting the need for emotional evaluation came out to be 78.1%, 58.5%, 50.9% in doctors, patients and insurance employees respectively.
Conclusion
Although a guideline for hospitalization of minor head injury patients is necessary, some part of it seems to be reevaluated and improved, especially for clauses related to the patient's emotional problems. These changes and revisions to the guideline require further speculation and research.
Until recently, no official hospitalization guideline existed for minor head trauma patients after a car accident in the Republic of Korea. Doctors without formal neurosurgical training decided whether a patient should or should not be hospitalized based on their general medical knowledge or based on guidelines used by other countries. The lack of a specific guideline frequently causes clashes among doctors, patients, and insurance companies.14)
As a victim of a car accident, the patient wants to receive the optimal treatment possible as to avoid future side effects. Thus, they often request unnecessary hospitalization even in the absence of any symptoms in the fear of aftereffects, or sometimes to earn a bigger insurance compensation.5,7,10,14)
Car insurance companies insist that the hospitalization rate of minor head trauma is exceptionally high in Korea compared to other countries. They believe that the high hospitalization rate is due to malingerers hospitalized only in document to earn unwarranted compensation. According to these companies, this leads the increment of insurance premiums and the burden is eventually returned to the majority of citizens.14)
Medical professionals argue that it is difficult to ignore a patient's request to be hospitalized, which makes it difficult to make a reasonable decision based on the patient's medical state. They also believe that the insurance companies' claim on over-hospitalization is invalid and insist that the patient should be granted as much treatment as they request. No objections are raised when the injuries are physical and visible but the patient's subjective symptom and emotional or mental problems are often neglected. A simple guideline for mild head trauma patients can restrict unnecessary evaluation and hospitalization, which will maximize consumer benefit by minimizing medical cost and insurance premiums. In the cases of patients whose pain is not supported by radiologic evidence, a guideline will allow these patients to be hospitalized without the pressure having to be discharged.
On June 28th, 2012, the Ministry of land, transport, and maritime affairs issued a hospitalization guideline for traffic accident patients, which establishes the fundamental principle that patient with mild injuries should be treated on an outpatient basis to minimize the number of malingering patients. Medical professionals, public interest groups, and insurance companies participated in creating this guideline.
The purpose of this paper is to improve and supplement the current "Hospitalization guideline for car accident patients" by reevaluating the current hospitalization guideline and including factors such as the subjective symptoms that the patient undergoes and the post traumatic emotional problems felt by the patients.
Based on the "Hospitalization guideline for car accident patients" issued in June 28th, 2012, surveys were created and given to 32 doctors working in primary and secondary medical institution, 96 car accident patients that visited primary, secondary, tertiary hospitals, and 60 insurance company employees. Questionnaires were sent through mail.
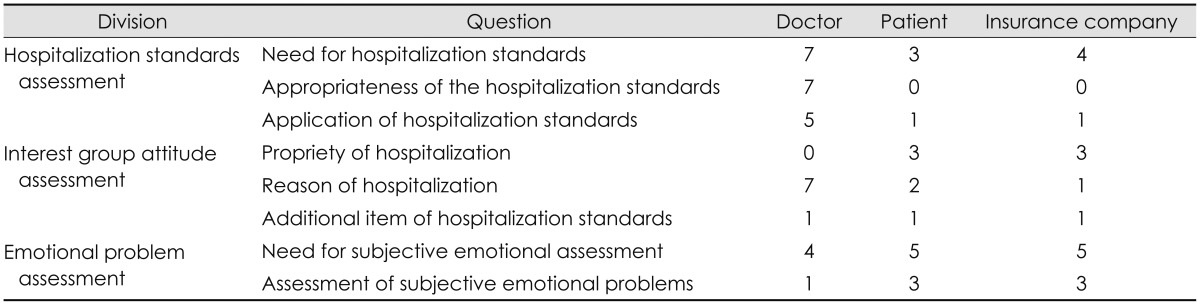
The survey is composed of 32 questions for doctors, 18 questions for patients, and 18 questions for insurance company employees. The survey is divided into three categories; hospitalization guideline assessment, interest group attitude assessment, and emotional problem assessment (Table 1). To minimize the confusion of the definition of mild head trauma, questionnaires for doctors defined mild head trauma as 'trauma resulting in acceleration or deceleration forces to the brain with transient alteration in consciousness, but without actual tissue injury', and the survey for patient stated 'light concussion, mild injury from head stubbing or hit by ball or other objects or light head injury accompanied by a short term of unconsciousness without brain hemorrhage and inflammation'.12)
1) The frequency and ratio of each response to an each question was analyzed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA) statistics program. Because the frequency of responses were different among the three groups (doctors, patients, and insurance companies), only the ratios were used for comparison. The assessment of suitability of hospitalization and the need to address emotional problems were analyzed using chi-squared test and Fisher test through cross tabulation.
2) The limitation of the survey analysis was that the number of answers one may choose in a multiple choice question was not restricted, and therefore the number of responses exceeded the number of people who participated in the survey. Thus, the results were analyzed using only the ratios. When the subjects answered questions that did not require answering they were discarded, and the multiple answers given to a single answer question were also discarded.
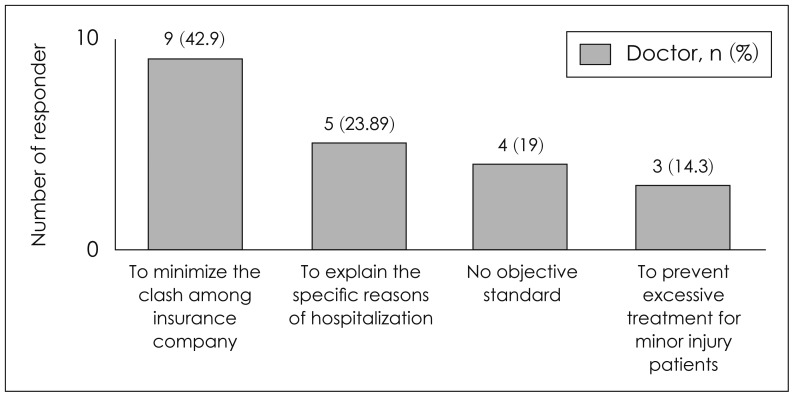
On the question that asks the need for mild head injury patients to be hospitalized, 68.8% of doctors gave affirmative responses and 31.2% gave negative responses. Among the ones that responded affirmatively, 42.9% argued that such standards are needed 'to minimize the clash among insurance company, doctors, and patients', 19.0% reasoned that it is needed because there is 'no objective standard', and 23.9% reasoned 'to objectively support reasons for hospitalization', and 14.3% reasoned 'to prevent excessive treatment for minor injury patients who can be fully recovered with simple treatment' (Figure 1). Among the ones who chose 'no', 40% reasoned that 'a minor head trauma guideline may be up for different interpretation depending on the affected group's self interest', 30% reasoned that there are 'no problems in current system', and some responded that 'every patient has their unique set of medical conditions'.
On the item which asks if respondents were introduced the 'Hospitalization guideline for car accident patients' issued by the Ministry of Land, Transport and Maritime Affairs, 18.8% of doctors said that they knew and 81.2% of doctors said that they didn't know. On the following question which asks whether the respondent is willing to use the guideline once they were introduced to it, 69.2% said that they are willing to follow the guideline (Table 2). Among the remaining 30.8% that responded 'not willing to follow', 75% of them said that 'the guideline seems proper but is doubtful about its application in reality' and 25% said that 'the guideline is improper'.
On the question 'what can be done to activate the use of the guideline?', 44.1% answered, 'campaign to inform minor head trauma standards to citizens' and 35.2% said 'induce the active participation of the doctor's union'. Some other answers were: 'broaden the guideline standards so that doctors can decide based on their conscience', 'increase patient burden of the hospital fee to reduce unnecessary hospitalization', and 'improve the current traffic accident insurance system' (Table 3).
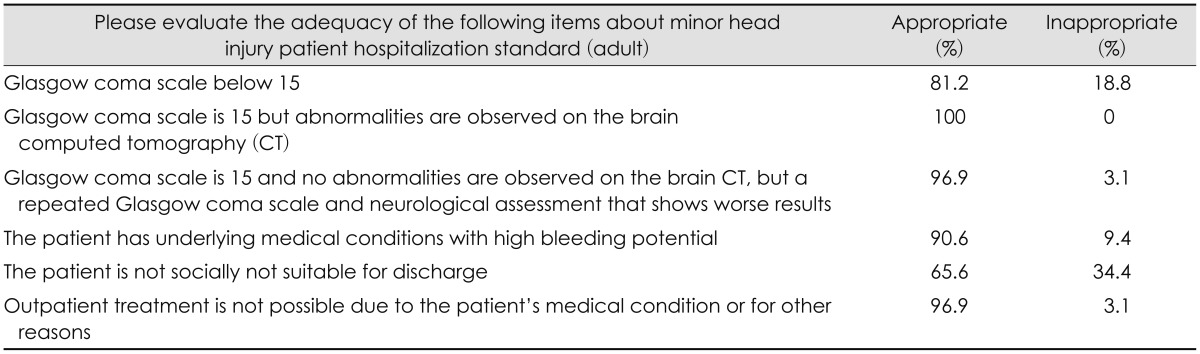
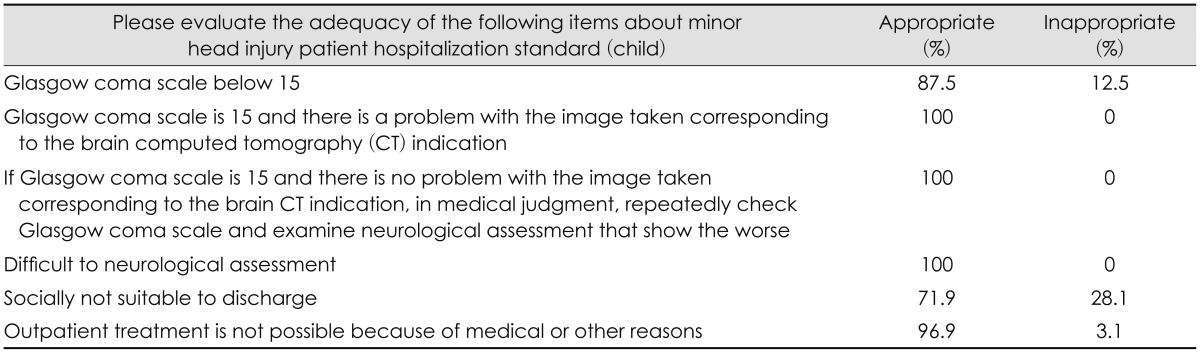
The following is the list standards included in the current hospitalization guideline for car accident patients issued by the Ministry of Land, Transport and Maritime Affairs.6) Thirty two doctors were given surveys about whether each criterion in the guideline is proper or improper as a standard. More than 90% believed that the standards were adequate except for the two standards, 'Glasgow coma scale below 15' and 'socially not suitable for discharge' (Table 4 and 5).
On the question whether respondent is satisfied with the evaluation questions, 59.4% responded positively and 40.6% responded negatively. Among the negative responses, 52.2% said that 'more questions are required for a full evaluation', 26.1% said 'not enough explanation provided', and 17.4% said that there are 'no evaluation questions for the patient's subjective emotion'.
On the question that asks the need for a hospitalization guideline, 79.8% of patients that participated in the survey said 'yes' and 91.6% of insurance company employee said 'yes'. This indicates that both patient and insurance company acknowledge the need for hospitalization standards (Figure 2).
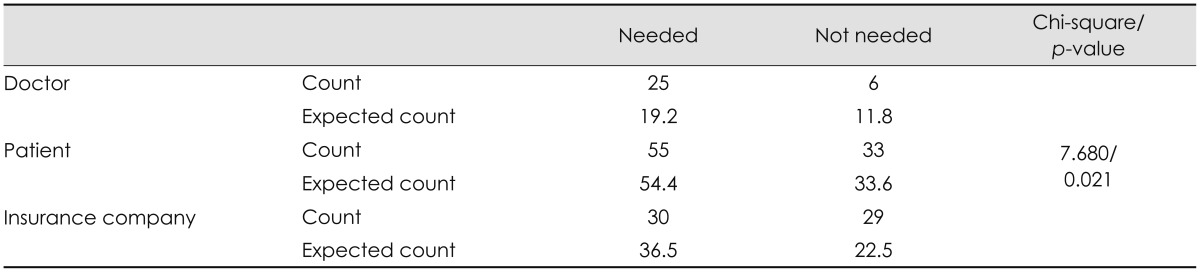
To evaluate the relationship among the three groups in terms of the need for a hospitalization guideline, we labeled those that answered 'completely true' or 'very true' as those that believed a hospitalization guideline was 'needed', and those that answered 'not true' or 'absolutely not true' as those that believed a hospitalization guideline was 'not needed'. Data revealed that there were significant differences in opinion among groups (Table 6).
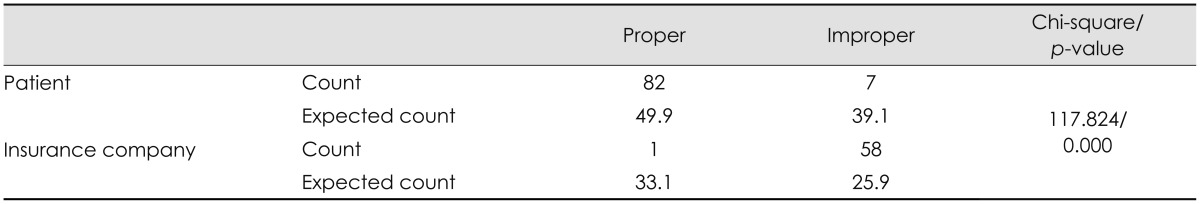
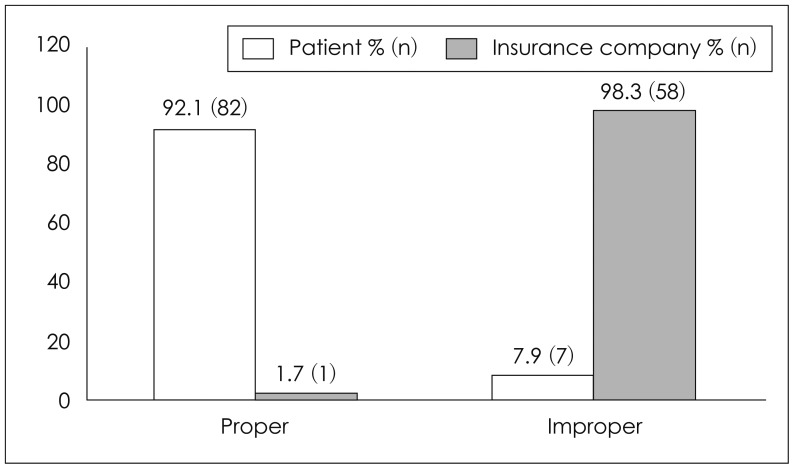
Contrasting responses were collected when the interest groups were asked, 'Are all the hospitalized patients actually in need of hospitalization?' 87.2% of patients said 'yes', but 96.7% of insurance company said 'no' (Figure 3). Further analysis reveals that validity of the difference of opinion between the patient group and insurance group (Table 7).
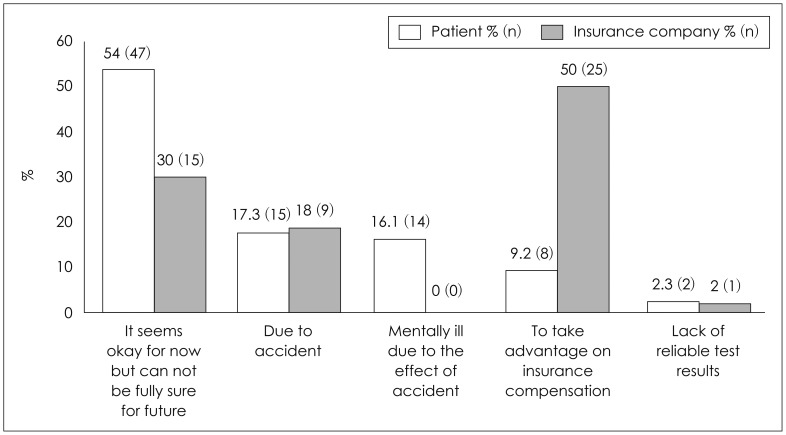
In terms of the reasons for hospitalization, 54.0% of the patients chose 'It seems okay for now but cannot be fully sure for future', 17.3% chose 'due to accident', 16.1% chose 'mentally ill due to the effect of accident', and 9.2% chose 'to take advantage of insurance compensation'. In contrast, 50.0% of insurance company chose 'to take advantage on insurance compensation', 30.0% chose 'mentally ill due to the effect of accident', and 18% chose 'due to accident' (Figure 4).
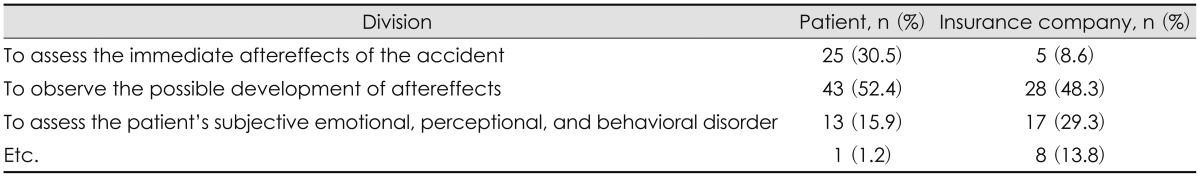
On the question that asks 'what items should be added to the guideline for the hospitalization of minor head trauma patients?', 52.4% of patients and 48.3% of insurance company chose 'to observe the possible development of aftereffects'. The next most frequent answer chosen by 30.5% of patients was 'to assess the immediate aftereffects of the accident', whereas 'to assess the patient's subjective emotional, perceptional, and behavioral disorder' placed second (29.3%) among the insurance company employees (Table 8).
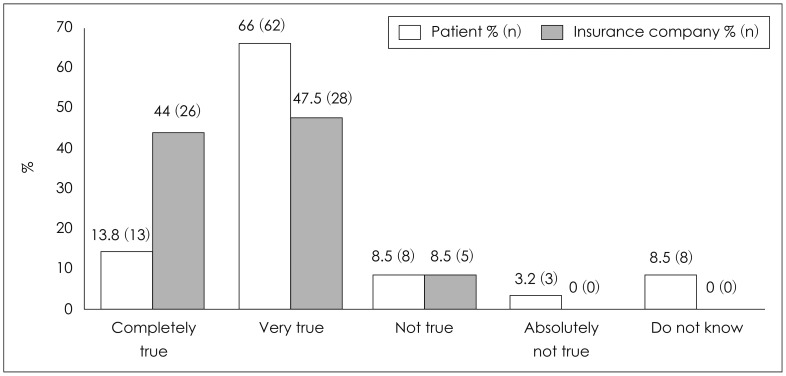
On the question of whether a subjective emotional evaluation is required, 78.1% of doctors, 58.5% of patients, and 50.9% of insurance company answered 'completely true' or 'very true' (Figure 5).
To evaluate the relationship among the groups, we labeled those that answered 'completely true' or 'very true' as those that believed emotional assessment was 'needed', and those that answered 'not true' or 'absolutely not true' as those that believed emotional assessment was 'not needed'. Data revealed that there were significant differences in opinion among groups (Table 9).
In terms of why an emotional evaluation is necessary, 56.2% of patients answered 'because patients feel uncomfortable in their daily lives', 19.3% of patients chose 'because doctors may miss the emotional problems felt by the patient', and 14.0% of patients answered 'because emotional problems are also injuries in need of treatment'. The insurance company answered different, 70% reasoned 'to distinguish malingerers who claim that they have an emotional problem' and 30% answered 'because emotional problems are also injuries in need of treatment'.
On the question which asks if the current evaluation method of emotional problems is reasonable, 87.5% of doctors, 63.8% of patient, 96.7% of insurance company gave negative responses (Figure 6).
On June 28th, 2012, the Ministry of Land, Transport and Maritime Affairs issued a 'Hospitalization guideline for car accident patients' which enforces outpatient based treatment of minor head trauma patients. The guideline was issued to minimize the number of malingerers as a way to improve the current car insurance system.6)
'Practice management guidelines for the management of mild traumatic brain injury' issued in the United States of America provides treatment directions by following standards set specifically for minor trauma patients and by evaluating the cognitive, behavioral, and emotional problems expressed by the patient.4) The 'Guidelines for mild traumatic brain injury following closed head injury' of Australia classifies minor trauma patients into high and low risk groups according to the degree of risk.8) In the case of head injuries, a patient is evaluated hourly over a period of four hours and the Abbreviated Westmead Post-traumatic Amnesia Scale (A-WPTAS) is used to evaluate cognitive function and current emotional state.8) The guideline provides an evaluation table which allows the doctors to record observations after discharge and evaluate post-traumatic disorders in detail. The 'National Institute for Health and Care Excellence guideline' of the United Kingdom suggests a treatment guideline and hospitalization standards by categorizing patients into infants, patients in need of an ambulance, patients in need of a computed tomography (CT) scan.1,9,11) It also describes specific discharge standards. In the 'European Federation of the Neurological Societies (EFNS) Guideline', the mild head injury patients are classified into four classes from 0 to 3, based on the Glasgow coma scale, patient consciousness, post-traumatic condition, age, drug addiction, and underlying risk factors.13) The World Health Organization also issued a guideline based on the diagnosis and treatment by age, symptoms, consciousness, Glasgow coma scale, drug addiction, fracture, and trauma mechinism.3) Lastly, the guideline issued by the Eastern Association for the Surgery of Trauma argues that a thorough neurological evaluation is necessary for patients with concussion syndrome during hospitalization even in the absence of neurologic abnormalities.2,4)
The Ministry of Land, Transport and Maritime Affairs enforces an outpatient based treatment for the management of mild car accident patients. The ministry also provides a hospitalization guideline for medical professionals based on the Glasgow coma scale, brain CT findings, neurological abnormalities, and underlying internal medical problem to allow certain minor trauma patients to be hospitalized. More than half of doctors, patients, insurance companies agreed to the opinion that hospitalization standards for mild head injury patients are necessary. This verified the need for a guideline which is expected to mediate the clash among doctors, patients, and insurance companies. It is difficult to say that the current guideline has been widely used clinically, judging from the result that suggests only 18.8% of doctors knew about the guideline. But as 69.2% of doctors who did not know about the guideline responded that they are willing to use it if they have chance to learn the guideline, the government should seek for a method that can introduce the new guideline to as many doctors as possible. And because many of the doctors who responded that they would not use the guideline had doubts about its proper application to reality, the government should investigate what problems exist in applying the guideline in reality and look for solutions.
In response to the question about whether the current guideline is proper or not, 18.8% and 33.4% of respondents, respectively, suggested that the standards 'Glasgow coma scale below 15' and 'socially not suitable to discharge' were not appropriate. Also, 40.6% of respondents gave negative responses about being 'satisfied with the evaluation items'. These results indicate that the current hospitalization standards are far from being complete. Therefore, the two items that received many negative responses need to be re-evaluated.
Our surveys also revealed that more factors should be taken into consideration for a full evaluation, as many believed that the current guideline does not evaluate enough items. Other countries such as Australia classify patients into several groups and give different observation periods to each group, which makes it easier to observe mild head injury patients in detail. In Australia, A-WPTAS score is used for disease evaluation. We also believe that adding objective criteria can improve the thoroughness of the evaluation. Countries like England and Australia also have a system known as 'patient notification and management' which informs patients of the possible aftereffects and condition that may worsen.
Our survey also revealed a difference of opinions between patients and insurance companies about the reasons for hospitalization. The patients argued that hospitalization was necessary to evaluate possible aftereffects, while the insurance companies insisted that patients wanted to be admitted for insurance payouts.
On the subject of emotional problems, doctors and patients showed similar opinion while insurance companies had different opinion. Most doctors and patients agreed that specific, detailed evaluation about subjective emotions is required, but only half of insurance companies agreed to this idea. When we asked about the reason additional evaluation is required, more than half of the patients answered that they were worried about their emotional health while more than half of insurance companies answered that it was necessary to help distinguish between fake patients. Such results support the fact the insurance companies have a tendency to ignore patients' emotional problems. All three groups, however, agreed to the fact that the current method of emotional evaluation is not adequate. Based on these results, the ministry should start research on a more suitable evaluation method and observe how other countries evaluate emotional problems. In the United States, an evaluation of emotional problems includes observation of abnormalities in attentiveness, concentration, memory, fluency of words, judgment, overall thinking skill, and standards of behavior. Emotional disorder is defined as showing signs of depression, anxiety, agitation, hypersensitivity, impulsiveness, and aggression. Such detailed standards should be considered in the evaluation method and applied to the patients.
An analysis of the survey results of the current patient hospitalization guideline reveals that its existence is not well known and that we are indeed in need of a more applicable guideline. The surveys also revealed that a more active government involvement and promotion is necessary. Among the many shortcomings of the current guideline, hospitalization standards, specifically 'Glasgow coma scale below 15' and 'socially not suitable to discharge', need to be re-evaluated. Secondly, new research is required and the standards of other countries should be thoroughly investigated in order to formulate a more detailed and representative hospitalization guideline. Both patients and insurance companies agreed that 'to observe possible development or change in symptoms' should be included in the standards, and that more research on the subject is necessary. Last but most importantly, additional research is required to better evaluate patients' subjective emotional problems.
This paper has several limitations. It was carried in one city which possibly limits the diversity of the samples. It was also carried out by a single organization and the specimen known as the doctor group was relatively small limiting representability. The survey also does not take the difference in the level knowledge and information of the survey population into consideration.
References
1. Baines P. NICE head injury guidelines review of the legal mandate. Emerg Med J. 2005; 22:706–709. PMID: 16189032.

2. Barbosa RR, Jawa R, Watters JM, Knight JC, Kerwin AJ, Winston ES, et al. Evaluation and management of mild traumatic brain injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012; 73(5 Suppl 4):S307–S314. PMID: 23114486.
3. Borg J, Holm L, Cassidy JD, Peloso PM, Carroll LJ, von Holst H, et al. Diagnostic procedures in mild traumatic brain injury results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004; (43 Suppl):61–75. PMID: 15083871.

4. Cushman JG, Agarwal N, Fabian TC, Garcia V, Nagy KK, Pasquale MD, et al. Practice management guidelines for the management of mild traumatic brain injury the EAST practice management guidelines work group. J Trauma. 2001; 51:1016–1026. PMID: 11706358.

5. Lee JH, Kim JE. Comparisons and implications of leading countries' regulation system related to high admission rate of car accident patients. Seoul: Korea Insurance Research Institute;2010.
6. Ministry of Land, Transport and Maritime Affairs. Hospitalization guideline for car accident patients. Sejong: Ministry of Land, Transport, and Maritime Affairs;2012.
7. Ministry of Land, Transport and Maritime Affairs. The Catholic University of Korea Industry-Academic Cooperation Foundation. A study on the basic research of improving car insurance health care delivery system: centered on the patient hospitalization and outpatient guide. Gwacheon: Ministry of Land, Transport and Maritime Affairs;2011.
8. Motor Accidents Authority NSW. Guidelines for mild traumatic brain injury following closed head injury. Sydney, AU: Ambulance Service of New South Wales;2008.
9. National Collaborating Centre for Acute Care. Head injury: triage, assessment, investigation and early management of head injury in infants, children and adults. London, UK: National Collaborating Centre for Acute Care;2007. 9. NICE Clinical Guidelines, No. 56.
10. Song YA. Improvement point and explanation for admission rate of car accident patients. Seoul: Korea Insurance Research Institute;2010.
11. Stavrinides V. Head injury admissions at a district general hospital: adherence to NICE guidelines. Online J Clin Audits. 2010. 2:Stavrinides.
12. The Korean Neurosurgical Society. Neurosurgery. ed 3. Seoul: Korea Medical Book Publisher;2005.
13. Vos PE, Battistin L, Birbamer G, Gerstenbrand F, Potapov A, Prevec T, et al. EFNS guideline on mild traumatic brain injury report of an EFNS task force. Eur J Neurol. 2002; 9:207–219. PMID: 11985628.

14. Yang DS. Present conditions and problems of automobile insurance victims admission. General Insurance. 2007; 468:14–24.
FIGURE 5
The necessity of evaluating the subjective emotional problems in minor head trauma patients.
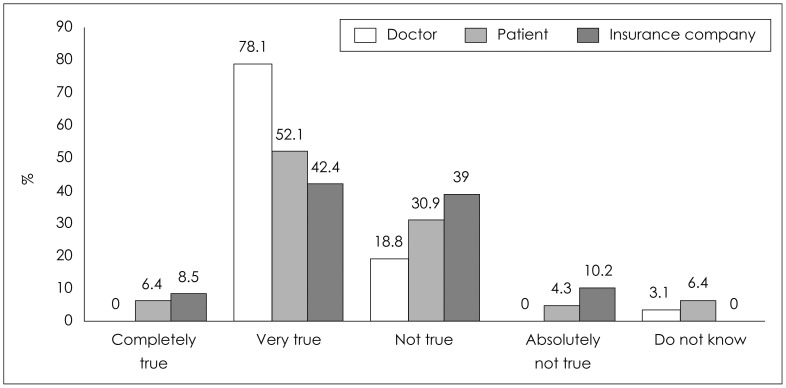
FIGURE 6
The appropriateness of the method in evaluating the subjective emotional problems regarding minor head trauma patients.
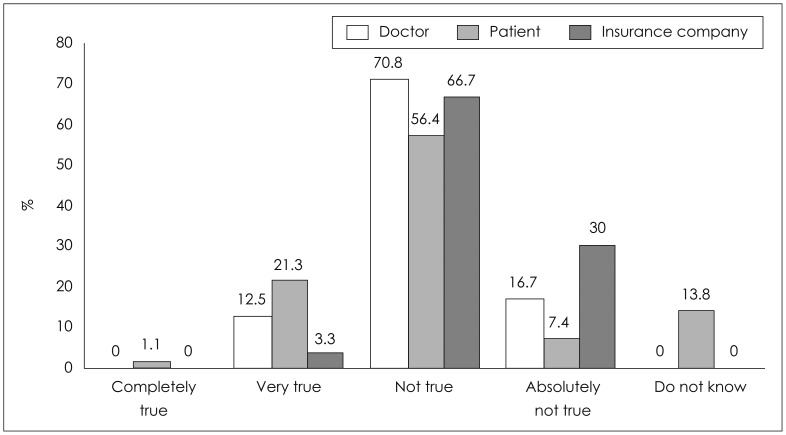
TABLE 2
Evaluation of 'Minor head trauma patients hospitalization guideline' from the Ministry of Land, Transport and Maritime Affairs applicability
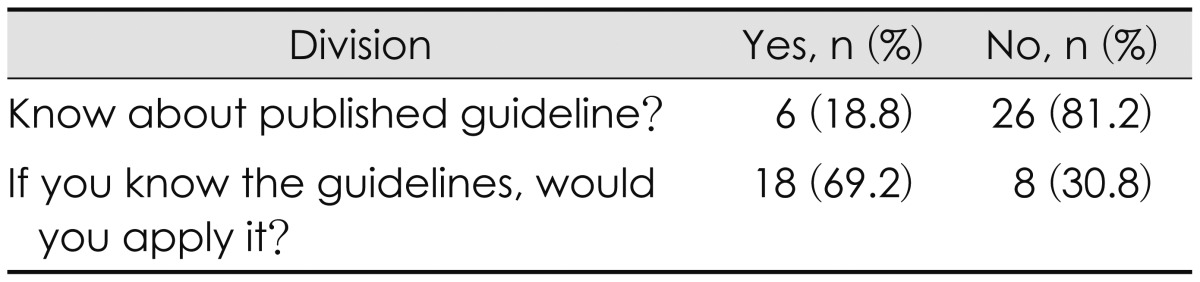
TABLE 3
The improvements to vitalize the 'Minor head trauma patients hospitalization guideline' from the Ministry of Land, Transport and Maritime Affairs
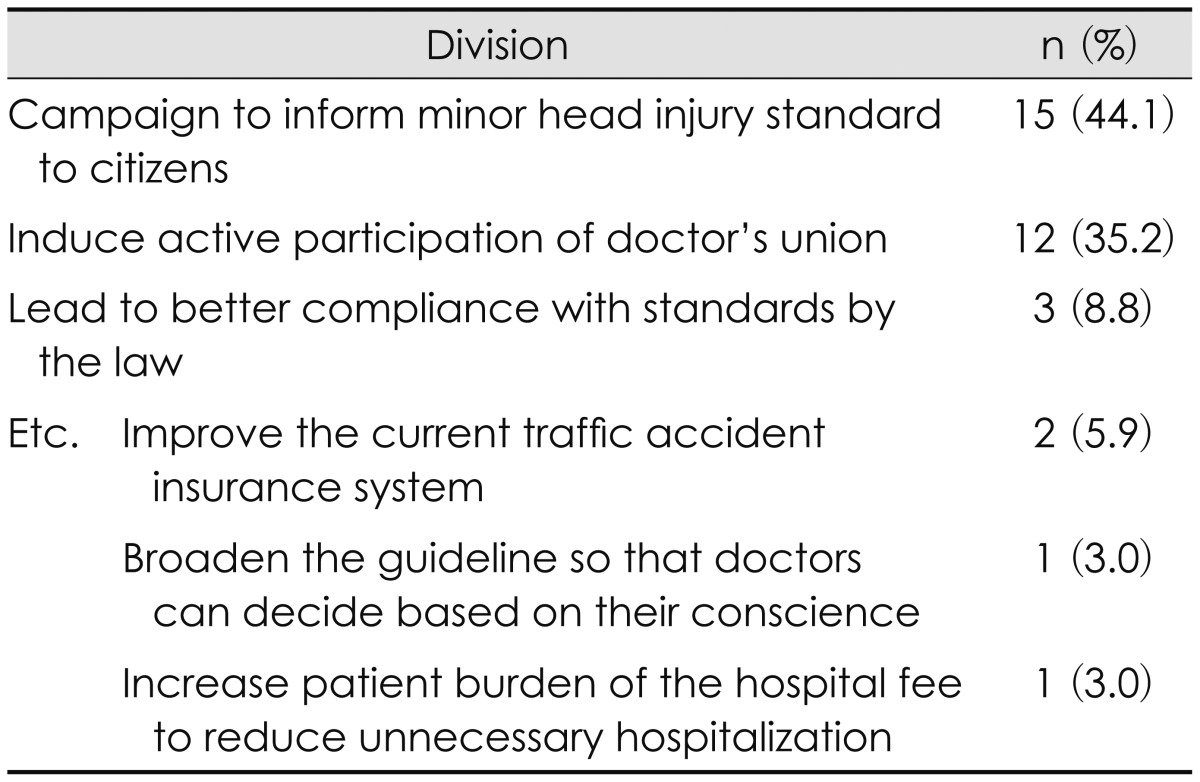
TABLE 6
Analyzing the correlation of the necessity of the minor head trauma patient's hospitalization guideline
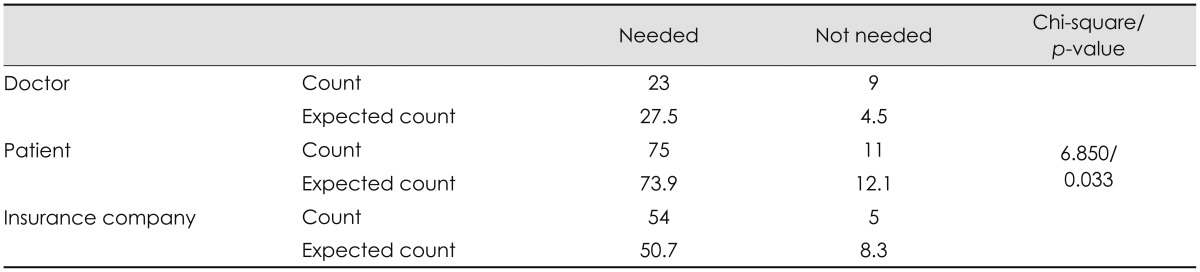
TABLE 7
Analyzing the correlation of the proper reason for hospitalizing the currently hospitalized patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download