This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To analyze factors associated with fusion using allogeneic bone spacers for midline splitting cervical laminoplasty (MSCL).
Methods
During April 2012 and September 2013, seventeen patients with cervical spondylotic myelopathy (CSM) or ossification of posterior longitudinal ligament (OPLL) underwent MSCL with allogeneic bone spacers by a single surgeon. Mean follow up periods was 11.3 months (range, 6-19 months). Clinical outcomes were evaluated by the Japanese Orthopedic Association (JOA) scores at preoperative and postoperative 6 months. Simple cervical X-rays were taken preoperatively, immediate postoperatively, 3, and 6 months after operation. Computed tomography (CT) scans were performed preoperatively, immediate postoperatively and 6 months postoperatively. The differences between two diseases were analyzed on cervical lordosis, canal dimension, anteroposterior (AP) distance, fusion between lamina and allogeneic bone spacer and affecting factors of fusion.
Results
All surgeries were performed on 59 levels. There were no significant differences on the changes of lordosis (p=0.602), canal dimension (p=0.554), and AP distance (p=0.924) as well as JOA scores (p=0.257) between CSM and OPLL groups. Overall fusion rate was 51%. Multivariate analysis on the factor for the fusion rates between lamina and spacers showed that the immediate postoperative contact status between lamina and spacers in CT as significant factor of fusion (p=0.024).
Conclusion
The present study suggests that CSM and OPLL did not show difference of surgical outcome in MSCL using allogeneic bone spacer. In addition, we should consider the contact status between lamina and bone spacer for the better fusion rates for this surgery.
Go to :

Keywords: Allografts, Spondylosis, Spinal fusion, Spinal cord diseases, Ossification of posterior longitudinal ligament
Introduction
Midline splitting cervical laminoplasty (MSCL) has been considered an effective and safe method for decompressing multisegmental cervical lesions caused by cervical spondylotic myelopathy (CSM) or ossification of the posterior longitudinal ligament (OPLL) as well as for achieving immediate stability of these lesions.
4,
5)
In the beginning of this procedure, autologous grafts from the iliac crest were used to keep the opened lamina splitted.
2) However, pain and discomfort at the donor site of the iliac crest were not uncommon, probably due to injury to the superior gluteal nerve,
11) and sunken-down of grafted bone spacer occurred. And then hydroxyapatite (HA) was introduced as a spacer material, but the fusion rate between HA and cervical lamina is not good,
9) which may cause sunken-down or pull out. In addition, HA has the higher potency of infection than autologous grafts.
7)
In contrast, allogeneic bone grafts can avoid the complications associated with harvesting autologous bone. Allograft materials are obtained from deceased human donors, undergoes rigorous safety screening, and can be transplanted into the patient at the time of surgery. The shape of allografts is well developed and capability to keep splitted lamina also increased.
6) However, the fusion rate of MSCL using allogeneic bone spacers has not been studied well.
The purpose of this study was to examine the clinical and radiological outcomes in patients undergoing MSCL using allogeneic bone spacers, especially compared the results between CSM and OPLL.
Go to :

Materials and Methods
A total of 27 consecutive patients with compressive cervical myelopathy including CSM and OPLL underwent MSCL using allogeneic bone spacers, Allo-Spine® LAMINA SPACER (CG Bio, Seoul, Korea) between April 2012 and September 2013. Of these 27 patients, 10 patients were lost to follow-up. Patients with cervical kyphosis, evidence of cervical instability and serious medical problems were excluded for this surgery.
Therefore, we retrospectively analyzed the outcomes of 17 patients (4 men, 13 women). Mean follow-up duration was 11.3 months (range, 6-19 months). Of these patients, 6 were diagnosed as CSM and 11 as OPLL. Three patients of CSM had myelopathy due to dynamic factor such as fall-down and traffic accident, and the others due to static factor such as soft disc herniation and congenital canal stenosis. Fifty nine spacers were used in total. The numbers and locations of spacers were: 11 at C3 level, 17 at C4, 16 at C5, 12 at C6, and 3 at C7.
A single surgeon performed all laminoplasties. He made gutters at the bilateral laminofacet junctions with a 3 mm diameter diamond type burr, and split the midline spinous process with a 2 mm diameter diamond type burr. The allogeneic bone spacers were inserted between the splitted spinous processes and fixed with 1-0 black silk.
Cervical X-rays were taken preoperatively, immediate post-operatively, and after 3, 6 months. Computed tomography (CT) was performed preoperatively, immediate post-operatively, and after 6 months. Cervical lordosis was defined as the angle between C2 and C7 inferior endplates. Change in overall cervical lordosis was assessed on X-ray images (
Figure 1). Spinal canal dimension and anteroposterior (AP) distance between the posterior surface of the vertebral body and the anterior surface of allogeneic bone spacer were assessed on axial CT images, which were measured at the level of the vertebral pedicles.
 | FIGURE 1Cervical lordosis, defined as the angle between C2 and C7 inferior end plates. 
|
The primary clinical outcome was the rate of change in the Japanese Orthopedic Association (JOA) scores (0-17) between preoperative and postoperative 6 month period. Recovery from myelopathy at 6 months was calculated using the formula: (6 month JOA score-pre operative JOA score)/(17-pre operative JOA score).
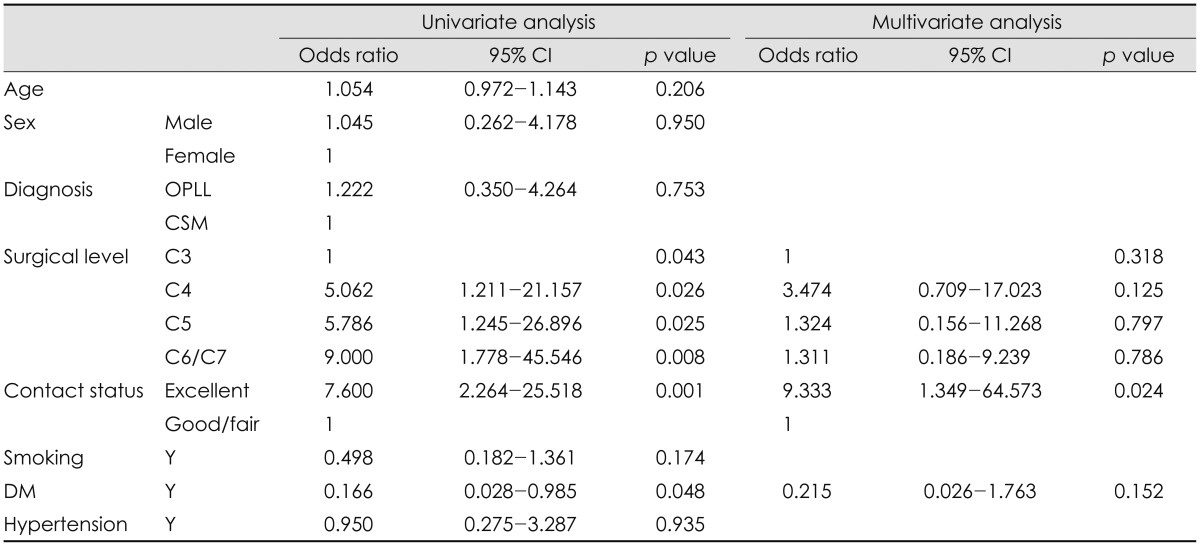
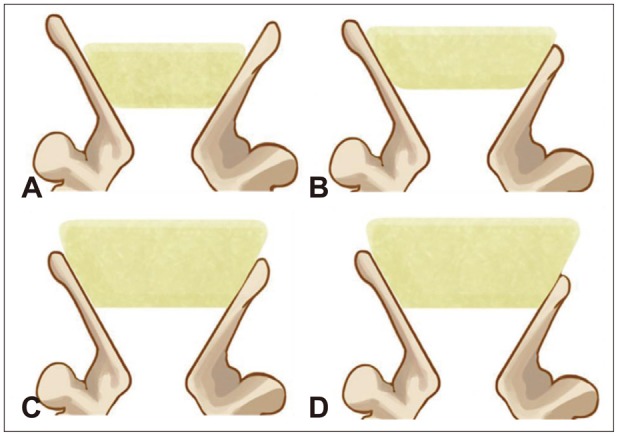
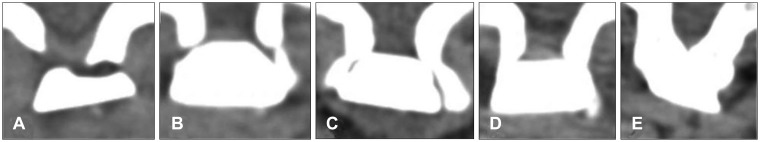
Contact status between lamina and allogeneic bone spacer immediately after surgery, and fusion between lamina and allogeneic bone spacer at 6 months were assayed as Hirabayashi method and Ichikawa classification (
Figures 2 and
3).
2,
3) D or E statuses were classified as fused status.
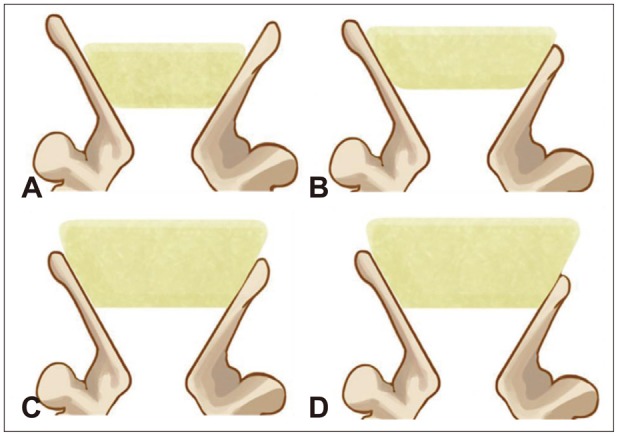 | FIGURE 2Four categories of immediate post-operative contact status between the spacer and the lamina. A: Excellent: complete touch on both sides of the spacer to the splitted spinous process. B: Good: complete touch on one side and more than half touch on the other side. C: Fair: more than half touch on both sides. D: Poor: half or less touch on at least one side. 
|
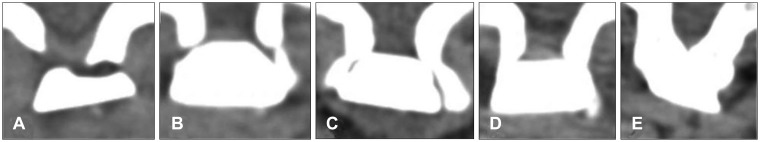 | FIGURE 3Fusion status between lamina and allogeneic bone spacer (Ichikawa classification). A: Bone resorption occurs around the implant. B: A clear space is present between the spacer and the bone without new bone formation. C: There is a space between the implant and the bone; however, new laminar bone formation is observed at the inner surface of the spinal canal. D: No space at the interface with new bone formation. E: Bridging of the new bone at the inner surface of the canal. When the different types were present at both interfaces, a lower degree of classification was applied. 
|
The factors that affected the rate of fusion between lamina and allogeneic bone spacer were analyzed by uni- and multivariate logistic regression. Age, sex, type of disease (CSM or OPLL), level of operation, contact status, smoking, diabetes mellitus (DM) and hypertension were included in these analyses. Groups were compared using the paired t-test, chi square test, Fisher's exact test, Mann-Whitney test, Linear mixed model, and uni- and multivariate logistic regression. We defined statistical significance as p value <0.05.
Go to :

Results
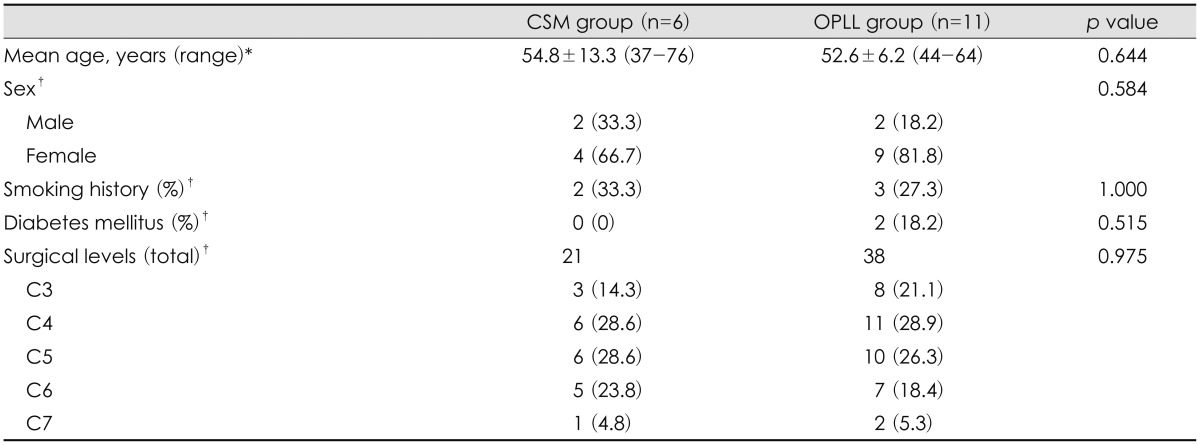
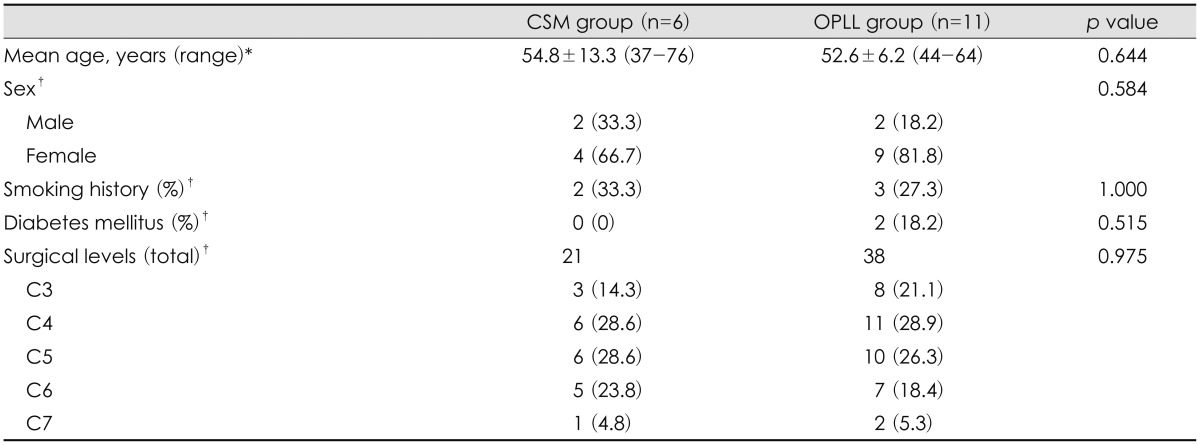
Patients were classified into two groups: CSM and OPLL. The baseline characteristics of the groups are shown in
Table 1. Of the 17 included patients, 6 were CSM and 11 were OPLL. Surgeries were performed on 59 levels, 21 for CSM and 38 for OPLL. There was no significant difference between those two groups in baseline characteristics.
TABLE 1
Characteristics of the two patient groups

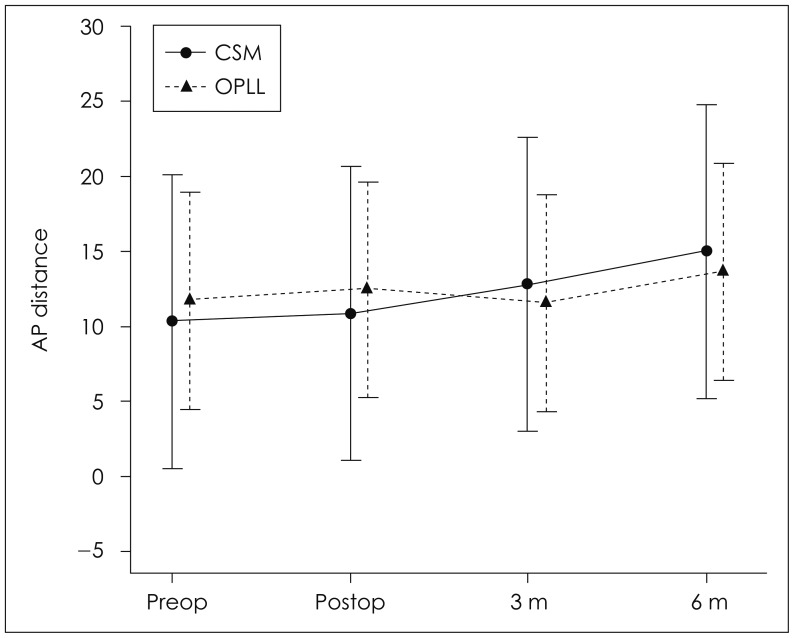
Mean cervical lordosis, which was defined as the angle between C2 and C7 inferior endplates, changed from 10.3±8.7 to 15.0±12.6 degrees in the CSM group and from 11.7±11.1 to 13.6±11.0 degrees in the OPLL group (
p=0.602)(
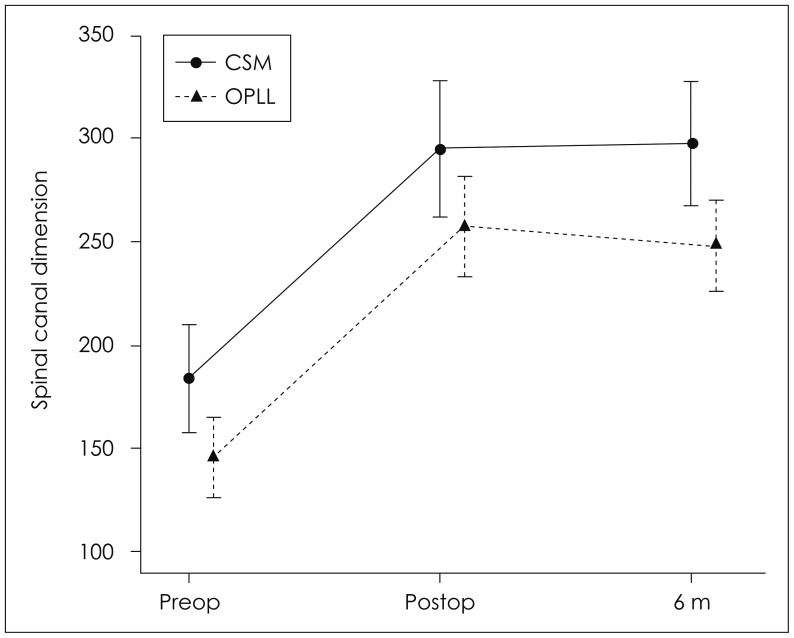
Figure 4). These data reveal the mean angle of cervical lordosis was not changed significantly and the occurrence of post-operative kyphosis was negligible. The spinal canal dimension was significantly increased after surgery from 183.1±41.1 mm
2 to 295.6±46.2 mm
2 in the CSM group (
p<0.001) and from 145.5±38.7 mm
2 to 255.8±56.6 mm
2 in the OPLL group (
p<0.001). In addition, the dimensions were evaluated as 299.0±34.2 mm
2 (
p=0.785) and 248.2±52.2 mm
2 (
p=0.216), respectively in post-operative 6 months. The spinal canal dimensions were increased with statistical significance after MSCL surgery in both CSM and OPLL, but there was no statistical difference between two groups (
p=0.554) (
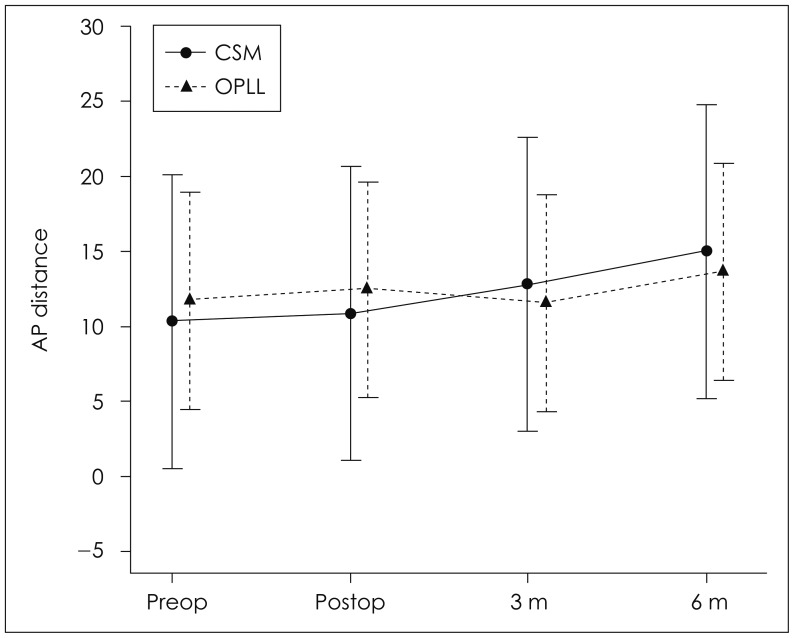
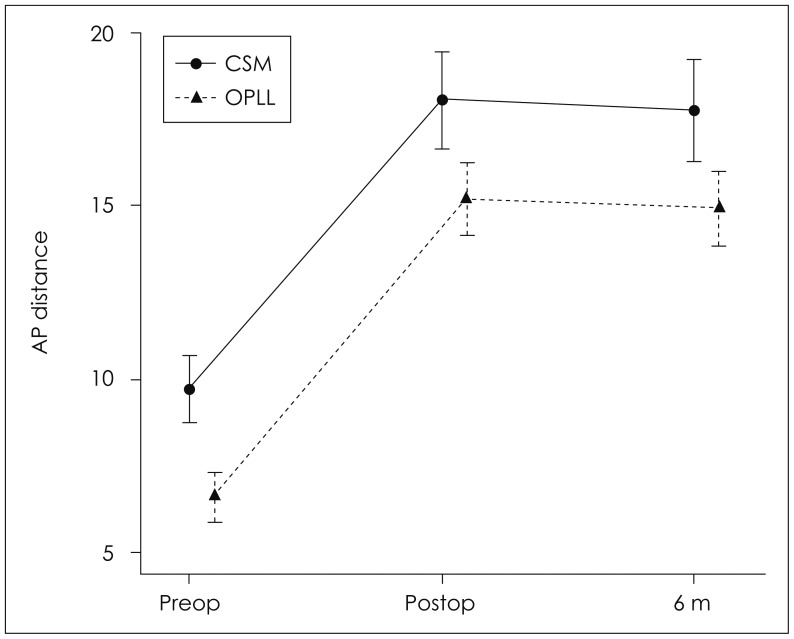
Figure 5). The AP distance of the spinal canal on axial CT images was increased immediately after surgery from 9.6± 1.6 mm to 17.9±2.0 mm in the CSM group (
p<0.001) and from 6.5±1.6 mm to 15.0±2.7 mm in the OPLL group (
p<0.001), but slightly decreased to 17.7±2.1 mm (
p=0.400) and 14.8±2.8 mm (
p=0.312), respectively at 6 months (
Figure 6). There was also no statistical difference in increase of AP distance between two groups (
p=0.924).
 | FIGURE 4Changes in cervical lordosis in the cervical spondylotic myelopathy and ossification of posterior longitudinal ligament groups. AP: anteroposterior, CSM: cervical spondylotic myelopathy, OPLL: ossification of posterior longitudinal ligament, Preop: preoperative, Postop: postoperative. 
|
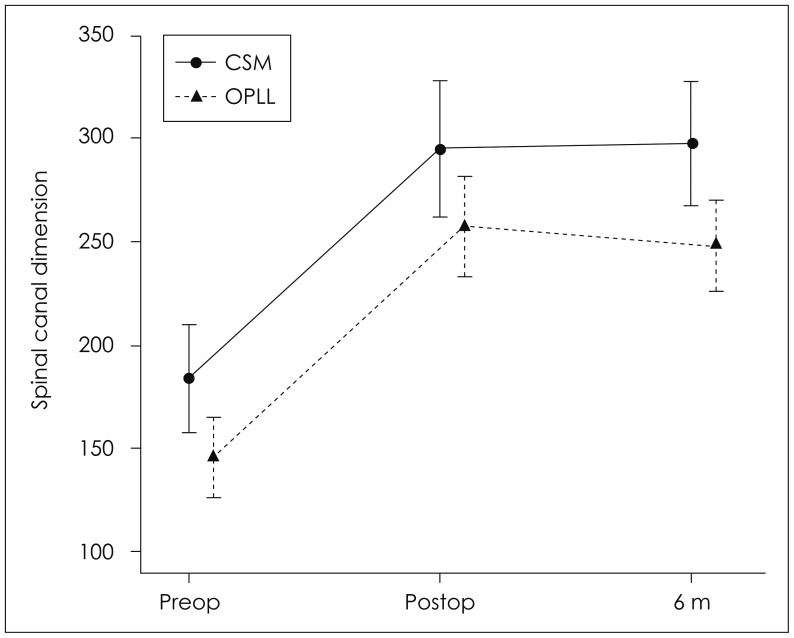 | FIGURE 5Changes of spinal canal dimension in the cervical spondylotic myelopathy and ossification of posterior longitudinal ligament groups. CSM: cervical spondylotic myelopathy, OPLL: ossification of posterior longitudinal ligament, Preop: preoperative, Postop: postoperative. 
|
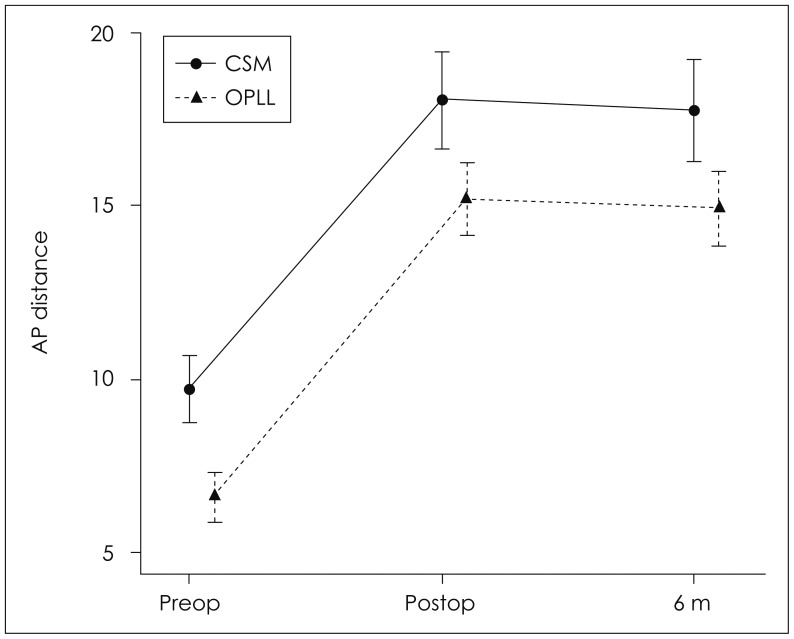 | FIGURE 6Changes of AP distance of the spinal canal in the cervical spondylotic myelopathy and ossification of posterior longitudinal ligament groups. AP: anteroposterior, CSM: cervical spondylotic myelopathy, OPLL: ossification of posterior longitudinal ligament, Preop: preoperative, Postop: postoperative. 
|
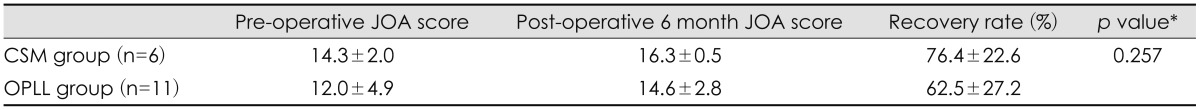
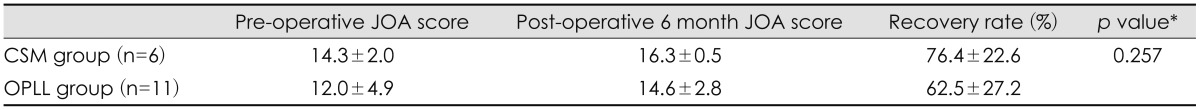
Mean JOA scores changed from 14.3±2.0 to 16.3±0.5 in the CSM group and from 12.0±4.9 to 14.6±2.8 in the OPLL group, with mean calculated recovery rates of 76.4±22.6% and 62.5±27.2%, respectively (
p=0.257)(
Table 2). There was no post-operative infection.
TABLE 2
JOA score changes in the two groups

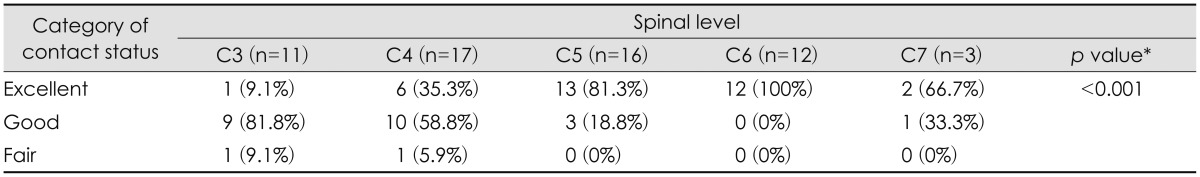
Excellent contact was achieved with 9.1% of spacers at C3, 35.3% at C4, 81.3% at C5, 100% at C6, and 66.7% at C7 (
p<0.001). Contacts between the spacer and the lamina become better in lower cervical level except C7 (
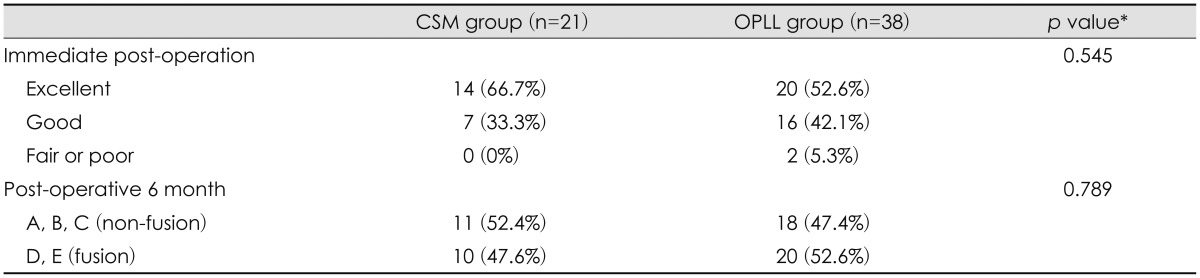
Table 3). In the respect of immediate post-operative contact status for CSM and OPLL, excellent in 14 levels (66.7%) and 20 levels (52.6%), good in 7 (33.3%) and 16 (42.1%), and fair at 0 (0%) and 2 (5.3%), respectively (
p=0.545). There was no poor status. The post-operative 6 month fusion status between lamina and allogeneic bone spacer, classified as D or E status were 30 (51%) in total, 10 (47.6%) in CSM, and 20 (52.6%) in OPLL (
p=0.789). There was no statistical difference in contact and fusion status between two groups. Excellent immediate post-operative contact status between lamina and allogeneic bone spacer had a significantly higher probability of fusion (
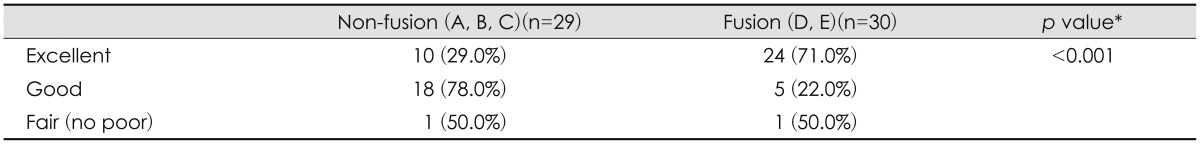
Table 4). In the respect of immediate post-operative bonding state affecting fusion rate, excellent group showed fusion in 24 (71.0%), good in 5 (22.0%), and fair in 1 (50.0%). Overall fusion rate was 51% (
Table 5).
TABLE 3
Number of spacers in each category of contact status between lamina and allogeneic bone spacer according to spinal levels
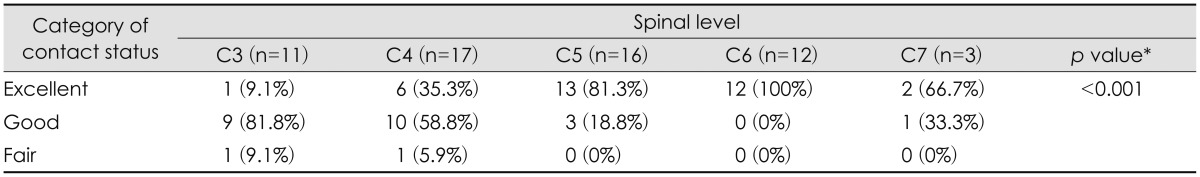

TABLE 4
Contact status and fusion status between lamina and allogeneic bone spacer in the two groups
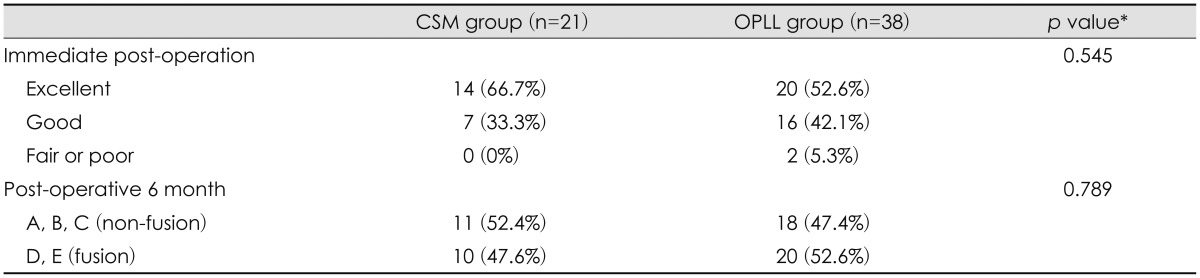

TABLE 5
Relationship between immediate post-operative contact status and fusion status after 6 months
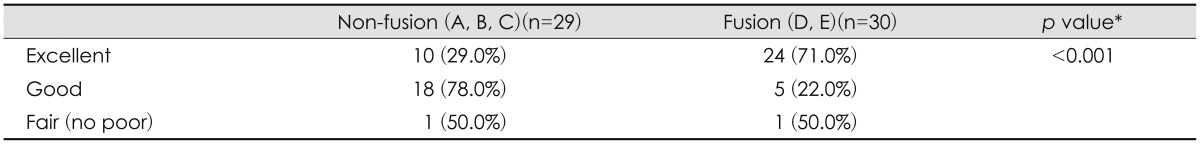

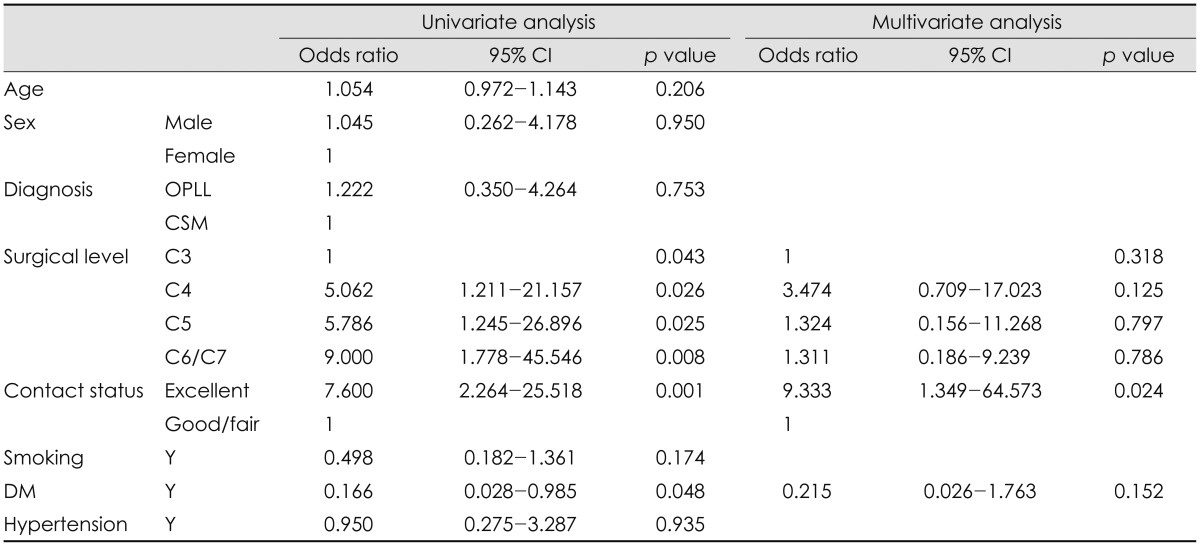
In univariate logistic regression analysis, surgical level of allogeneic bone spacer (
p=0.043), immediate post-operative contact status of spacer (
p=0.001), and absence of DM (
p=0.048) were significant factors. However, multivariate logistic regression analysis showed only contact status of lamina and bone spacer as significant factor of fusion (
p=0.024)(
Table 6).
TABLE 6
Logistic regression of factors affecting fusion between lamina and allogeneic bone spacer

Go to :

Discussion
There was no significant difference in clinical recovery rate between CSM and OPLL in previous studies.
1,
12) Our results in this present study also support the data, in which post-operative clinical outcomes were significantly improved in CSM as well as OPLL, but no significant difference between two groups. The reason why there was no difference in clinical outcome between two groups could be primarily because this clinical outcome was affected by decompression of the spinal cord and post-operative expansion of spinal canal dimensions were similarly increased in two groups.
In the previous report on MSCL using HA spacer,
9) the overall fusion rate between lamina and HA was 27.46% and wingless type HA, which is similar shape as the allogeneic bone spacer used in this study showed 48.8%.
9) In our present study, the fusion rate was 51%, which is slightly higher than wingless type HA. Allogeneic bone material has physiologic matrix structure and porosity compared to HA material. Therefore, allogeneic bone spacer seems to have higher potential for bone fusion even though it was sterilized with antibiotics, chemicals, and gamma ray. But it had the potential of disease transmission such as viral hepatitis, tuberculosis, syphilis, septicemia and malignancy.
10)
In multivariate analysis, initial contact status between lamina and allogeneic bone spacer significantly affected fusion status. Nagashima et al.
8) demonstrated in animal experiments that a high degree of new bone formation occurred at the interface between the spacer and the spinous process. This finding is consistent with our study. We think that the splitted spinous process becomes higher in lower cervical levels and contacts between the spacer and the lamina become better in lower cervical level which explains the significance in univariate analysis.
The limitations of our present study are that this study is not prospective analysis and there were small cases in some classified groups such as C7 level and good/fair contact status. To study further results and outcome about MSCL using allogeneic bone spacer, additive analysis may be needed with prospective, larger cases and longer follow-up duration.
Go to :

Conclusion
This present study suggests that CSM and OPLL did not show difference of surgical outcome in MSCL using allogeneic bone spacer. In addition, we should consider the contact status between lamina and bone spacer for the better fusion rates for this surgery.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download