Abstract
Objective
This retrospective study was undertaken to evaluate the efficacy of combined microscopic fragmentectomy and intraoperative nucleoplasty for sequestrated lumbar disc herniation.
Methods
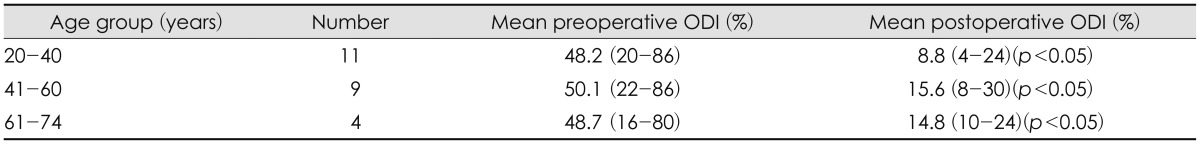
Twenty-four patients with magnetic resonance imaging proven sequestrated lumbar disc herniation with small annular leak treated by microscopic fragmentectomy and nucleoplasty were included. Patients were followed for at least one year. The Oswestry Disability Index (ODI; version 2.0) was used to assess preoperative and postoperative functional statuses in three age groups (20-40, 41-60, and >60 years). Visual analog scale and modified MacNab's criteria were used to assess the clinical outcomes for spinal surgery.
Results
Mean age at operation was 41.2 years (range 20-72 years). ODIs improved significantly regardless of age group. Significant pain relief was achieved at 1 year after surgery. Most patients (92%) had an excellent or good result according to modified MacNab's criteria, and all patients showed symptomatic improvement after surgery. There were two postoperative wound-related complications, and both responded to antibiotics. No patient underwent further additional surgery because of disc re-herniation during follow-up.
Go to : 
The terms "migrated" and "sequestrated" disc or fragment refer to displacement of disc material away from the opening in the annulus through which it has been extruded.5) When the distinction between the outer annulus and the posterior longitudinal ligament (PLL) is unclear and the torn annulus opening is small in sequestrated lumbar disc herniation, optimal surgical treatment is still debatable. Williams13) reported successful results for a microsurgical approach to a virgin herniated lumbar disc that involved removal of only the free fragment compressing the nerve root. By preserving healthy intervertebral disc material, this procedure supposedly offers excellent success rates, few complications, and a low recurrence rate. However, Rogers8) reported a high recurrence frequency after surgery involving removal of only the offending fragment as compared with more extensive discectomy. Of the therapeutic minimally invasive treatment options currently available, nucleoplasty is commonly performed to decompress nucleus pulposus and lower intradiscal pressure by inserting devices into the affected intervertebral disc.9) The purpose of this study was to determine the surgical outcome of microscopic fragmentectomy and intraoperative nucleoplasty in cases of sequestrated lumbar disc herniation.
Go to : 
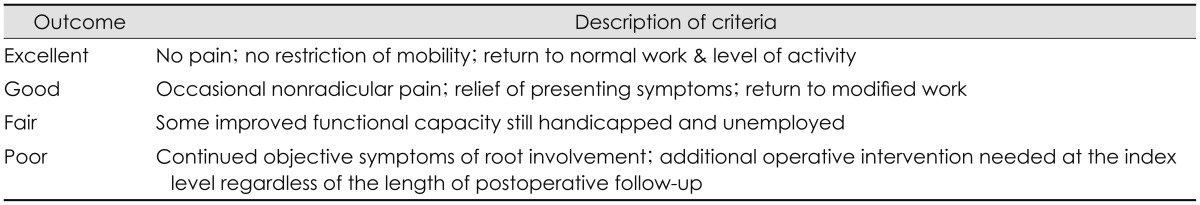
Twenty-four patients with magnetic resonance imaging confirmed sequestrated lumbar disc herniation that underwent combined microscopic fragmentectomy and intraoperative nucleoplasty between 2009 and 2012 were included in this study. After sufficient consenting to the surgical procedure, all underwent combined microscopic fragmentectomy and nucleoplasty by the same surgeon. The Oswestry Disability Index (ODI) questionnaire version 2.0 was used to assess degree of disability and functional status caused by sequestrated discs.4) All patients completed the ODI questionnaire preoperatively and at 1-year postoperatively. In all cases, microscopic fragmentectomy was followed by intraoperative nucleoplasty. To quantify pain and functional outcomes, we used modified MacNab's criteria (Table 1) and a 10-point visual analog scale (VAS). Statistical analysis was performed using the paired t-test and a confidence interval of 95%.
All operations were performed under general anesthesia in the prone position. A microscope (Carl Zeiss, Oberkochen, Germany) was mounted to aid removal of sequestrated disc material. Exposure was obtained in each case according to the direction of the free fragment by making a 2-3 cm midline skin incision. In most cases, exposure of the ruptured disc fragment and involved nerve root was possible with minimal disturbance of the lamina or adjacent facet and limited bone removal. In all 24 patients, only the ruptured sequestrated fragment compressing the nerve root was removed. Epidural fat was disturbed as less as possible and only bleeding epidural vessels were coagulated. Intraoperative nucleoplasty was performed following successful microscopic fragmentectomy. Under fluoroscopic guidance, a 17 guage, 6 inch cannula was inserted into the targeted disc space lateral to the facet joint. After confirming correct cannula placement, an introducer needle was inserted into the disc. Once in proper position, of an introducer needle to the ruptured site a radiofrequency (RF) device (L-disq®, U&I company, Uijeongbu, Korea) was inserted, and as suggested by a manufacture company guideline, at least 7 RF passes were performed.
Go to : 
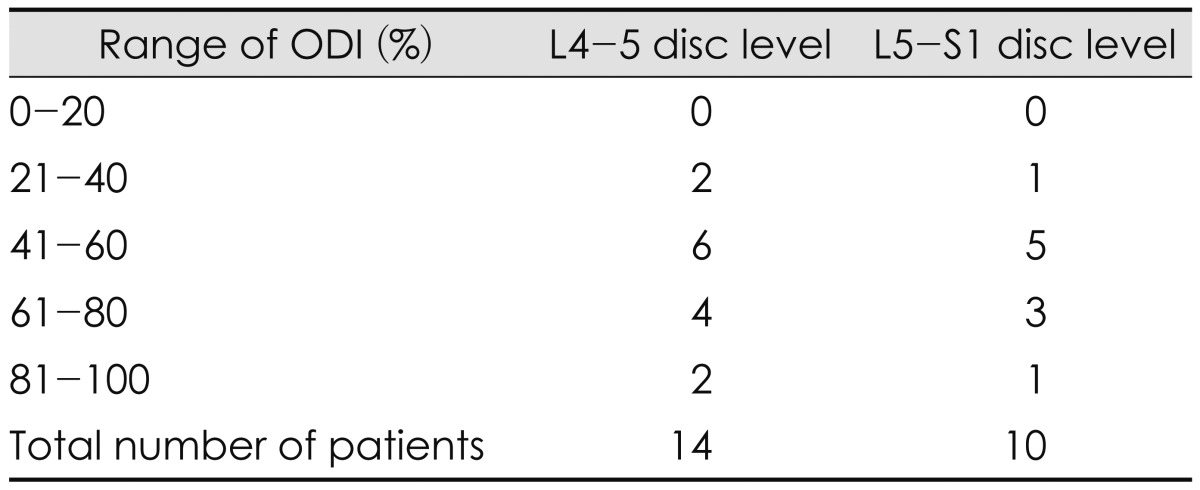
The 24 patients (mean age 41.2 years, range 20 to 74 years) were followed for a minimum of 1 year (mean follow-up 16.3 months). Involved levels were; L4-5 in 14 and L5-S1 in 10. Prior to the procedure, 11 patients had a disability score of 41-60%, 7 patients a score of 61-80%, 3 patients a score of 21-40%, and 3 patients a score of 81-100% (Table 2). ODIs improved significantly after combined microscopic fragmentectomy and intraoperative nucleoplasty regardless of age group (20-40, 41-60, and >60), (p<0.05)(Table 3). Furthermore, according to the 10 point VAS used (0=no pain and 10=intractable pain), mean pain levels dropped significantly from 8.3±1.5 to 2.6±1.6 (p<0.05). Most patients (92%) achieved an excellent or good result according to the modified MacNab's criteria at final follow-up (excellent: 14, good: 8). All patients obtained symptomatic improvement after surgery. However, one patient complained of occasional intermittent back and buttock pain, which subsequently required radiofrequency neurotomy, despite complete relief of radiating pain. Two postoperative wound-related complications responded to antibiotics, and no recurrent disc herniation was encountered during follow-up.
Go to : 
A free sequestrated fragment may migrate, which means that disc material moves away from the opening in the annulus.6,11) Some migrated fragments will be sequestrated, but the term migrated refers to position and not to continuity.5) When the opening in a torn annulus is tiny and the intervertebral disc involved is relatively healthy, the optimal surgical approach is debatable.
Williams13) developed the concept of microsurgical removal as applied exclusively to offending material decompressing neural structures and the dural sac without touching relatively healthy discal or bony components or articulations; this minimal approach has the advantage of leaving the normal anatomy relatively intact. Young patients that present with radiologically preserved intervertebral height, a disc with otherwise little degenerative change, and a near intact posterior ligament and annulus fibrosus at operation are expected to profit most from fragmentectomy, and the small opening is expected to seal spontaneously and permanently without further herniation. Wenger et al.11) also reported successful results for minimal bone removal and excision of only the completely extruded disc fragment without entering the disc space. However, this technique was not used in patients with a subligamentous herniation, a large tear in the annulus or in the PLL, or with a fragment not clearly separated from the disc space. Rogers8) reported a elevated recurrence rate when only the offending fragment was removed as compared with more extensive discectomies. Unfortunately, complete clearance of all disc material is not possible, because there is no distinct border between the rigid annulus fibrosus and the soft nucleus pulposus, and thus, visualization of the intervertebral disc space and instrument accessibility are limited. Furthermore, degenerative discopathy and extensive curettage of the interspace reduces intervertebral disc height and subsequently loosens ligaments and articular capsules. In addition, these loosenings, combined with reduced discal support in the anterior column, could result in segmental instability, facet arthrosis, and spondylosis, which in turn, could cause disc space narrowing and imbalanced weight bearing on spinal structures, and consequently, increase weight bearing at the facet joint.2,7,10)
Nucleoplasty, also known as percutaneous discectomy, is a minimally invasive procedure that uses RF energy to remove nuclear material.1) This technology involves the application of RF energy to a conductive medium and the creation of a highly focused plasma field (composed of ionized particles) around energized electrodes. The proposed mechanism of nucleoplasty's therapeutic effect is that it reduces intradiscal pressure. Thus, nucleoplasty combines coagulation and tissue ablation to form channels in nucleus and cause disc decompression. Shabat et al.9) reported successful outcomes without complications in 87 patients with mechanical back and radicular pain at a minimal follow-up of 1 year after nucleoplasty. The best candidates for nucleoplasty are patients with radicular pain secondary to a contained disc herniation or axial pain. The findings of a cadaver study conducted by Chen et al.1) showed that patients with incomplete annular tears and a minimally degenerated disc benefit most from nucleoplasty. Accordingly, it appears patients with a large fissure are unlikely to benefit from nucleoplasty, despite "contained" disc herniation. Instead, nucleoplasty could be alternative technique for small annular tear on behalf of the extensive microdiscectomy. Although, sequestrated disc herniation tends to have large annular fissure with PLL injury generally, we could obtain good surgical outcome by lowering intradiscal pressure without additional extensive discectomy. In the present study, significant improvements in VAS scores and ODIs were achieved after a minimum follow-up of 1 year. Furthermore, revision surgery due to re-herniation was not required during follow-up. However, there are always risks. Infection, bleeding and neural injury are uncommon but possible risks. Moreover, Cuellar et al.3) reported progressive disc degeneration in patients with persistent pain after nucleoplasty in less than 1 year after surgery.
It has been well established that patient selection is important for achieving satisfactory results after microscopic discectomy in cases of lumbar disc herniation. In their retrospective review of 259 lumbar discectomies. Wera et al.12) showed a significant increase in revision surgery because of the re-herniation of extruded disc fragments through a large or massive annular defect. This suggests that microscopic fragmentectomy is performed for a sequestrated lumbar disc herniation without additional opening in case of small annular leak, it would help to ameliorate symptom. And in such cases, intraoperative nucleoplasty can help to reduce intradiscal pressure. However, despite the successful outcomes achieved, this by no means indicates that patients with sequestrated lumbar disc herniation should be treated using this technique. There are two major limitations in this study. First, there is a lack of sufficiently powered studies and randomized control trials to support the widespread adoption of this procedure. Second, we did not study the relation between the disc degeneration grade such as Pfirrmann scores and clinical outcome. It should be performed cautiously due to its remarkable cost and the risk of neural injury, infection, bleeding and disc degeneration.3) In particular, despite our successful results, this does not mean most patients with lumbar disc herniation should be treated using this technique and patients with a large annular tear or PLL injury should be included carefully. We suggest that a long-term randomized control comparative study should be conducted to confirm our results in the near future.
Go to : 
Combined microscopic fragmentectomy and intraoperative nucleoplasty without conventional discectomy is a safe operative modality for sequestrated lumbar disc herniation. As demonstrated by the present series, the results obtained are favorable, and thus, we recommend this procedure can be viewed as a alternative treatment as compared with standard microsurgical lumbar discectomy with extensive nucleus pulposus removal.
Go to : 
References
1. Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine (Phila Pa 1976). 2003; 28:661–665. PMID: 12671352.

2. Cho BH, Kim SW, Lee SM, Shin H. The factors affecting the low back pain after microscopic discectomy. Korean J Spine. 2006; 3:158–161.
3. Cuellar VG, Cuellar JM, Vaccaro AR, Carragee EJ, Scuderi GJ. Accelerated degeneration after failed cervical and lumbar nucleoplasty. J Spinal Disord Tech. 2010; 23:521–524. PMID: 21131800.

4. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25:2940–2952. discussion 2952. PMID: 11074683.

5. Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society. American Society of Spine Radiology. American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 2001; 26:E93–E113. PMID: 11242399.
6. Ha JG, Park JH, Jeon SR. Clinical and radiological outcome analysis on anterior cervical discectomy and interbody fusion using hydroxyapatite block. J Korean Neurotraumatol Soc. 2011; 7:63–67.

7. Kim SW, Lee SM, Shin H. Radiofrequency facet denervation for low back pain after microscopic discectomy. J Korean Neurosurg Soc. 2005; 38:442–444.
8. Rogers LA. Experience with limited versus extensive disc removal in patients undergoing microsurgical operations for ruptured lumbar discs. Neurosurgery. 1988; 22(1 Pt 1):82–85. PMID: 3344091.

9. Shabat S, David R, Folman Y. Nucleoplasty is effective in reducing both mechanical and radicular low back pain: a prospective study in 87 patients. J Spinal Disord Tech. 2012; 25:329–332. PMID: 22124428.
10. Shao Z, Rompe G, Schiltenwolf M. Radiographic changes in the lumbar intervertebral discs and lumbar vertebrae with age. Spine (Phila Pa 1976). 2002; 27:263–268. PMID: 11805689.

11. Wenger M, Mariani L, Kalbarczyk A, Gröger U. Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery. 2001; 49:329–334. discussion 334-335. PMID: 11504108.

12. Wera GD, Dean CL, Ahn UM, Marcus RE, Cassinelli EH, Bohlman HH, et al. Reherniation and failure after lumbar discectomy: a comparison of fragment excision alone versus subtotal discectomy. J Spinal Disord Tech. 2008; 21:316–319. PMID: 18600139.

13. Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976). 1978; 3:175–182. PMID: 663769.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download