Abstract
Objective
Chronic subdural hematoma (CSDH) is common in elderly patients. So, with an increasing number of elderly people in the general population, there is a need to investigate risk factors which increase recurrence rate. In this study, factors affecting the postoperative recurrence are investigated based on the reoperative CSDH cases.
Methods
Total of ninety-seven patients was enrolled in this study who had have operation for CSDH. In all patients, one burr hole trephination and drainage was the method of choice for the initial treatment of CSDH. We retrospectively evaluated several factors which affect to recurrence of CSDH.
Results
Retrospective analysis was performed in 97 patients. Sixteen patients experienced reoperation within 3 months (16/97, 16.5%) for recurrence of CSDH. And, when hematoma was divided by internal architecture, heterogeneous density group seems to be have close relationship with recurrence more significantly than homogeneous density group (p=0.002). Hypertension, diabetes mellitus, early removal of drainage tube, bilaterality of hematoma also have significant relationship with recurrence.
Conclusion
Recurrence rate of CSDH treated with one burr hole drainage is related with some various factors. There was statistically significant difference between recurred group and non-recurred group. Not only demographic factors but also internal architecture on preoperative brain computed tomography is a significant predicting factor of recurrence in CSDH patients who underwent a surgery. In this study, heterogeneous type hematoma have significantly related with recurrence of CSDH. We should give attention to these predicting factors for more effective care.
Go to : 
Chronic subdural hematoma (CSDH) is one of the most common diseases in neurosurgical practice. CSDH tends to occur in elderly male patient. Head trauma is the most common cause of subdural hematoma. But, identified history of trauma is obvious in about only half of patients. A trivial trauma can also attribute subdural hematoma formation in elderly group. Common treatment choice of CSDH is a surgical treatment, and several surgical methods included twist drill craniostomy, burr hole with drainage, and craniotomy with hematoma removal introduced up to date.2,6,13,15,18,22,28) During the past several decades, less invasive burr hole and drainage is the most common procedure. The surgical outcome of CSDH reported in the previous literatures varies widely with a percentage of recurrence rate from 3% to 30%.2,3,5,7,11,12,17,27,29) In spite of comparatively simple operative procedure, the recurrence rate is relatively high as compared with other traumatic brain injuries. A repeated operation has increased morbidity and mortality.14,16,18) Furthermore, the patients undergoing a repeated operation have suffered financially and psychically during that period. If we can reduce the recurrence rate by to study about risk factors that lead to recurrence, there will be an effective care for CSDH patients.
Therefore, we evaluated the predicting factors for recurrence of CSDH in 97 patients who underwent one burr hole and drainage for CSDH in our department.
Go to : 
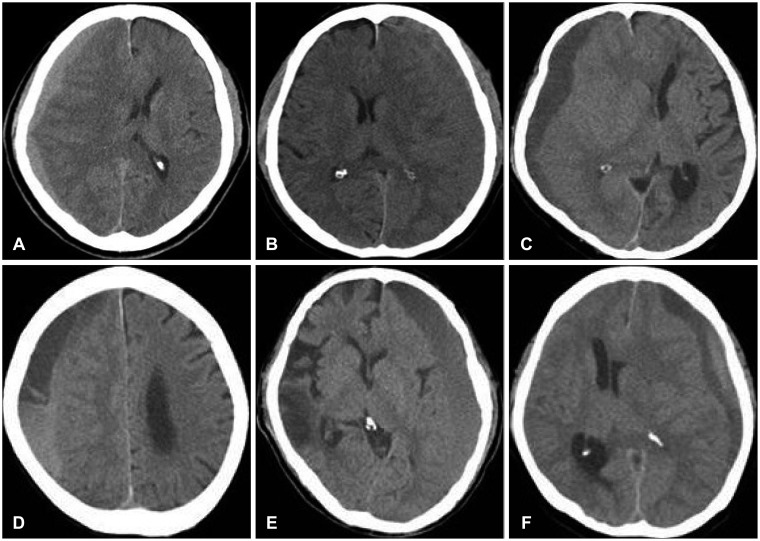
This study was based on retrospective analysis of 97 surgical cases of CSDH from January 2009 to October 2012. All patients enrolled in this study are treated with one burr hole and drainage, and have more than 3 months follow-up period. First, we diagnosed as subdural hematoma by computed tomography (CT) findings. And, we prove that by to confirm the dark reddish liquefied subdural hematoma, intraoperatively. To check-up brain CT was performed at the first visit to our institute, immediate postoperatively, and just before removal of drainage tube. Thereafter, we checked-up CT in the only patients having new symptom. We defined recurrent CSDH as the case of the reaccumulation of hematoma on the previously operated side in follow-up brain CT within 3 months after the previous operation. But, remained hematoma cases in brain CT due to capsulation by membrane were excluded. Among the 97 patients, 16 patients experienced reoperation due to recurrence of CSDH within 3 months. We retrospectively evaluated several factors that affect to recurrence of CSDH. Such as age, gender, hypertension (HTN), diabetes mellitus (DM), head trauma history, drainage tube removal time and preoperative CT findings were reviewed in this study. There are some factors in preoperative CT findings such as the thickness of hematoma, the degree of midline shift, the bilaterality of hematoma and internal architecture of hematoma. First, we classified the internal architecture of hematoma into two groups according to homogeneity in the CT images; homogeneous group and heterogeneous group. After then, each two groups were divided into three subtypes. Homogeneous group was divided as hyper-, iso-, and hypodensity type based on hematoma density. And, heterogeneous group was divided as separated, gradient and mixed type based on characteristics of hematoma (Figure 1). In here, the separated type means that hematoma shows a definite horizontal separated line, and the gradient type doesn't have the separated line, but have a gradation in the hematoma. The mixed type is not relevant to these two types. The thickness of hematoma and the degree of midline shift were decided by measuring the maximal numeric values in the CT images.
In our institute, a single burr hole trephination and drainage is a first line therapy. In general or local anesthesia, a small single burr hole site is usually on the frontal bone nearby Kocher's point or on the temporal line of parietal bone. And, if the reoperation was needed, we identified a new burr hole site in all recurrent patients. Cauterization of the dura was performed with a bipolar coagulator. After opening the dura, dark reddish colored liquefied blood gush out. Then, we diagnose CSDH exactly. A silastic drainage tube was inserted into the subdural space. And, intraoperative irrigation was done in every patient. The drainage tube was usually removed after two days postoperatively. And, early drainage removal time was defined as that removal time was shorter than 24 hours after surgery.16) In all patients, the time of drainage tube removal was when the drainage volume is less than 20 milliliters in last 8 hours. And, early drainage removal time was defined as that removal time was shorter than 24 hours after surgery.
Statistical analyses were performed to find the significant predicting factors of recurrence by applying chi-square test and logistic regression analysis. In this study, a p-value of <0.05 means statistically significant for all analyses.
Go to : 
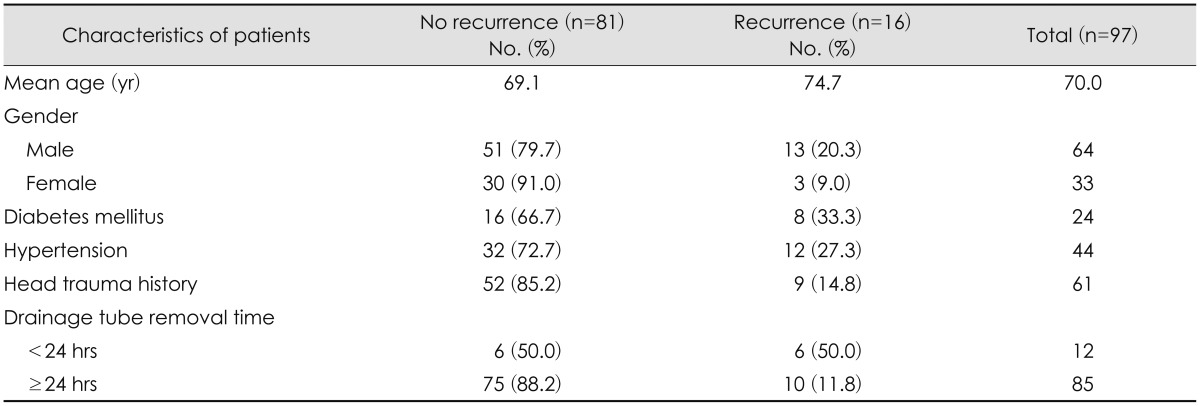
The characteristics of 97 patients are summarized in Table 1. Sixteen patients (16.5%) were recurred and all patients underwent a reoperation. Patient's data was similar to other previous articles. Sixty-four men and 33 women (ratio 1.9:1) enrolled in this study, and their mean age was 70.0 years (range, 15-93). Patients having DM are 24 (24.7%) and having HTN are 44 (45.4%). Sixty-one in all patients (62.9%) had remembered their head trauma history in the past few months. There are a few different features between recurrence group and no recurrence group. In recurrence group, mean age (±standard deviation) of patients (74.7±8.9) was older than no recurrence group (69.1±12.8). And recurrence group's male/female ratio (4.3:1) was higher than that of no recurrence group (1.7:1). The recurrence rates of patients having a history of HTN or DM (27.3%, 33.3%) were also higher than those of who do not have (7.6%, 11.0%). And the recurrence rate of patients having a history of head trauma (14.8%) was lower than that found in other group without a history (19.4%).
In our study, old age, male, HTN or DM and early drainage removal generally show us tendencies of recurrence.
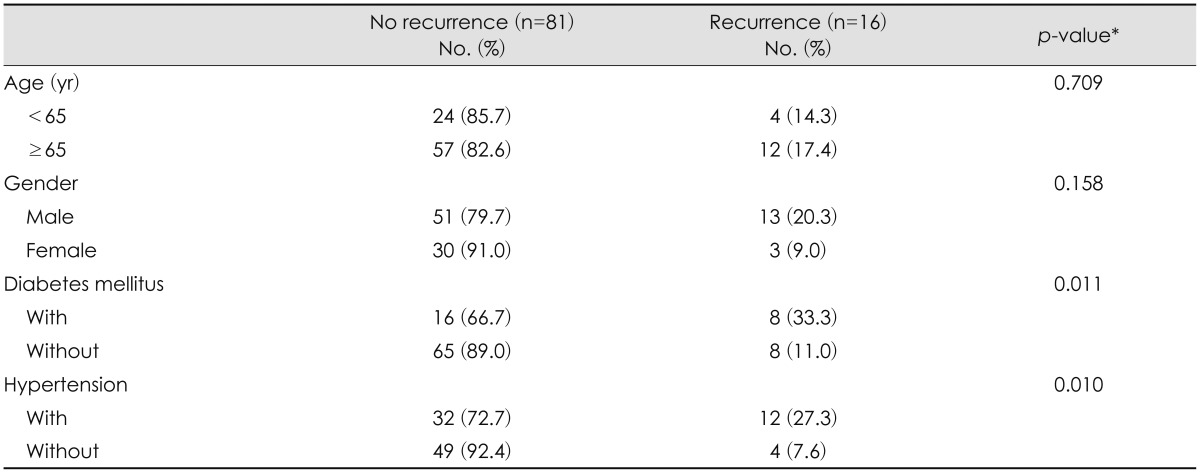
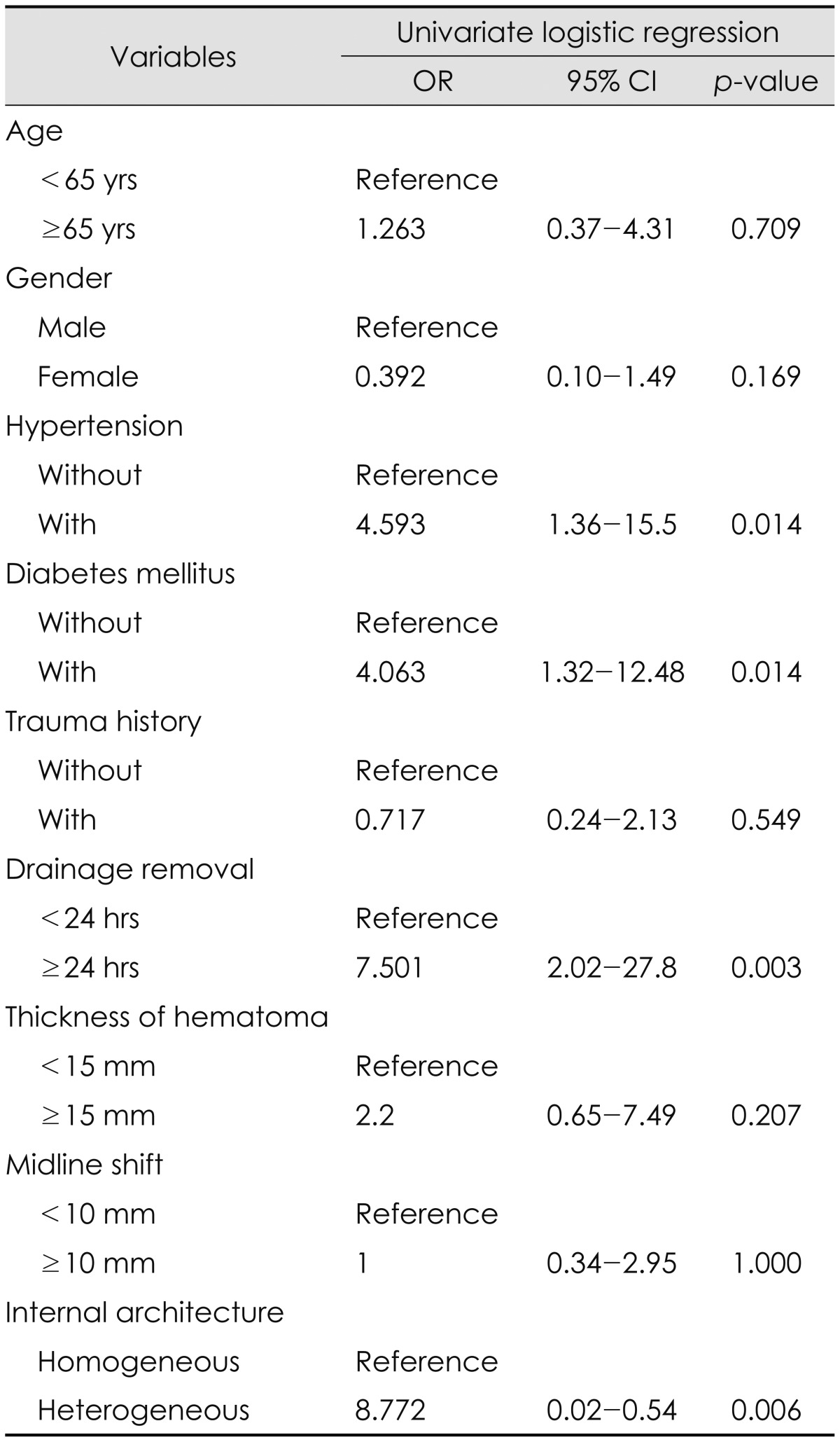
CSDHs occur frequently in male elderly group in generally. And there are 64 men and 33 women (mean age, 70.0 yrs) enrolled in this study. The recurrence rate of CSDHs tends to be higher in male patients (20.3%) and in the elderly (17.4%) than that of other groups. But, patient's age and gender were not statistically significant (p=0.709, p=0.158) (Table 2).
In sixteen recurred patients, 12 patients had a history of HTN and 8 patients had DM. There are controversial in relationship between recurrence and having HTN or DM. But, having underlying disease (HTN, DM) was statistically related to a recurrence of CSDH after surgery in this study (p<0.05)(Table 2).
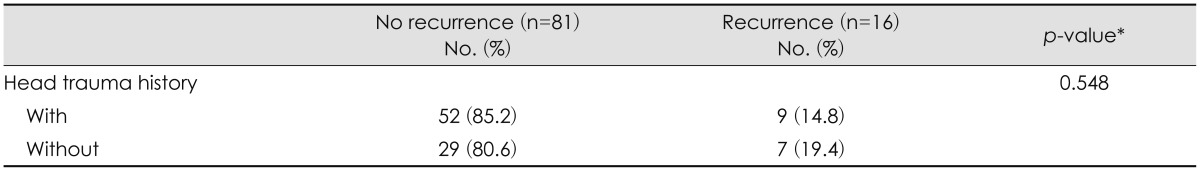
Many patients didn't have a cleared head trauma history. The experience of head injury remained in their memory in only 61 patients (62.9%). The analysis of correlation between the recurrence rate and head trauma history is shown at Table 3. There was no significant difference statistically (p=0.548). Nonrecurrent group's trauma history rate (64.2%) was rather slightly higher than recurred group's (56.3%).
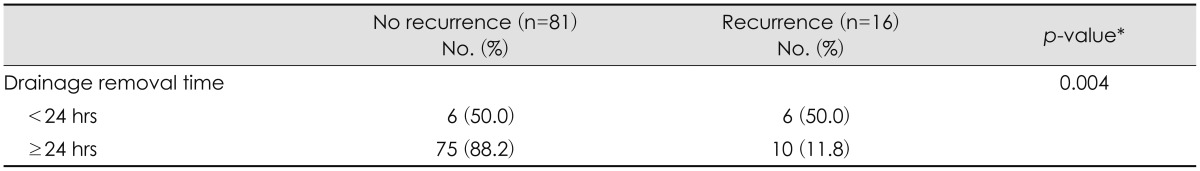
Drainage removal in 24 hours postoperatively was usually a little fast time. Early drainage removal was enacted in 12 patients of 97 patients (12.4%) in our study. All the patients' drainage volume in last 8 hours was less than 20 mL, without exception. Half of them are in recurred group. The closed relationship between recurrence rate and drainage removal time is shown in the statistical analysis (p<0.05) (Table 4).
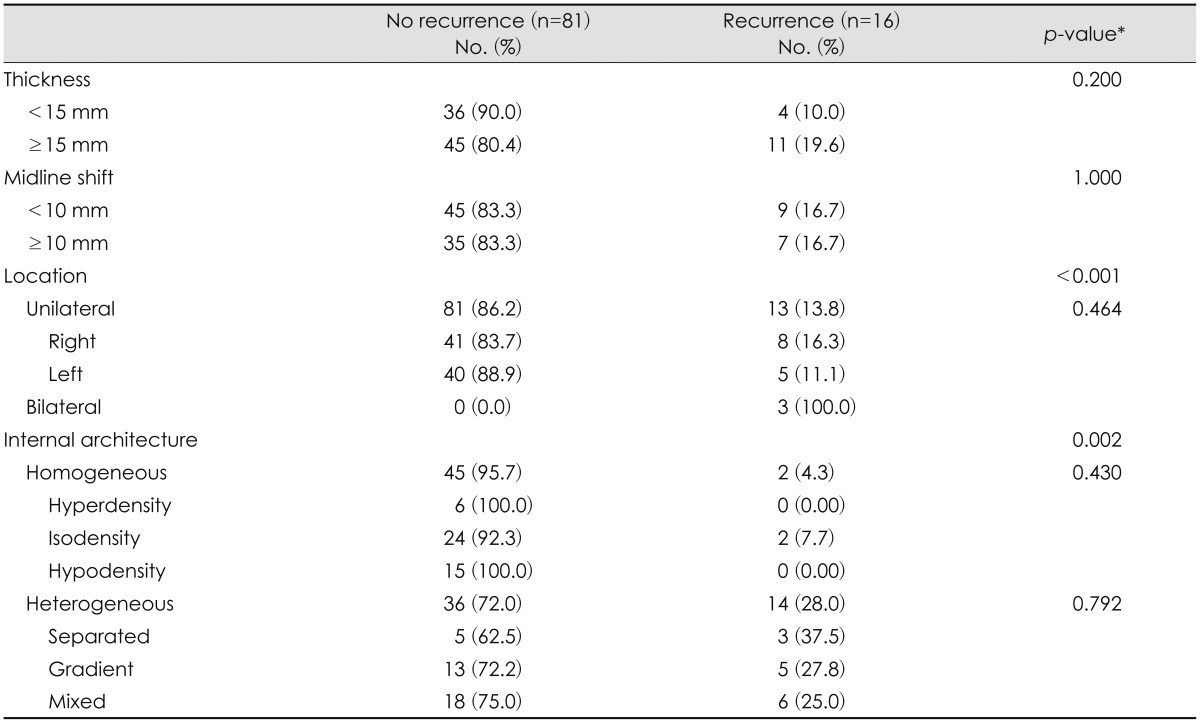
There was no standard criterion on the division of the degree of thickness in previous articles. We divided our patients into two groups on the thickness of hematoma by 15 mm. The recurrent patients who were 15 mm or more were 11 (19.6%), and the recurrent patients who were less than 15 mm were 4 (10.0%). But, there was statistically no significant difference (p=0.200)(Table 5).
The degree of midline shift also didn't have a statistical significance in recurrence (p=1.000). The recurrence rates of patients more than 10 mm and other patients (16.7%) were same (Table 5).
We divided our patients into unilateral group and bilateral group. Three patients of bilateral group all experienced a recurrence. In other words, only three patients in this study have the bilaterality of hematoma, and all of them are in recurred group. The bilaterality had a statistical significance in recurrence (p<0.001). But, there was no significant difference between right side group and left side group (p=0.464)(Table 5).
Internal architecture was discussed for the recurrence factor of CSDH in many previous articles.2,4,7,10,11,17,23) First, patients were categorized into two groups in accordance with homogeneity, homogeneous and heterogeneous group. Since then, homogeneous group is divided into hyperdense, isodense, and hypodense type based on hematoma's density. And, heterogeneous group is divided into separated, gradient and mixed type according to hematoma's character.
The statistical analysis about the relationship between internal architecture and recurrence shows that heterogeneous hematoma has a tendency of recurrence (p<0.05). But, each subtypes in a homogeneous group (p=0.430) and in a heterogeneous group (p=0.792) are not significantly different (Table 5).
Go to : 
The predicting factors for postoperative recurrence of CSDH were researched in several previous articles.1,2,4,7,8,9,10,11,16,21,23,25,29) But, each article's definition of recurrence is slightly different. And, the predicting factors of recurrence can be influenced by those differences.
In consideration of the definition of CSDH recurrence, the time interval between the initial surgery and recurrence varies in each articles from within 3 months1,2,4,7,10,11,17,29) to 6 months or more.20,21,26) And, the recurrent cases of only ipsilateral hematoma were enrolled in the study in most of articles,4,7,10,17,21,25,26) but both ipsilateral and contralateral hematoma recurrent cases came under the study in several articles.16,20) There are also some trivial differences, aside from these two differences. We defined recurrent CSDH as the case of the reaccumulation of hematoma on the only operated side within 3 months after the previous surgery. We exclude reoperative cases for remaining hematoma due to septation of wall and contralateral hematoma recurrence. Only complete resolution cases were comprised in this study. So, the results may be possibly different from the previous articles, notably in the internal architectures.
The internal architecture of hematoma is a important predicting factor of postoperative recurrence in a few previous articles.2,4,7,10,11,17,18,23) Nomura et al.19) previously divided CSDHs into five types according to hematoma's appearance on preoperative brain CT (known as the internal architecture): hyperdensity, isodensity, hypodensity, mixed-density and layering types. And, Tsutsumi et al.26) analyzed the difference of recurrence rate among these types. There were no statistical differences in recurrence rate in the report.
Nakaguchi et al.17) classified the internal architecture of the hematoma in other way. They divided internal architecture of CSDHs into four types: homogeneous stage (hyperdensity, isodensity, and hypodensity subtype), laminar stage which be considered to be a subtype of the homogeneous stage, separated stage (including the gradient stage), and trabecular stage which features septation of wall. In this classification, the mixed-density type in the classification of Nomura et al.19) divided into the trabecular and laminar types, because the laminar type has a higher recurrence rate than the trabecular type, in spite of their similar mixed-density appearance. The laminar and separated type had a high recurrence rate, statistically.
In our study, patients were divided into two groups in accordance with homogeneity: homogeneous and heterogeneous group. After then, each group was divided into three subtypes. In the statistical analysis, the heterogeneous group had a high recurrence rate than homogeneous group (p=0.002). But, there were no statistical differences in recurrence among each subtype.
These differences of the results among the articles are due to various reasons. Though difference of classification is one of the reasons, the different definition of recurrence can be also the reason. The recurrence of laminar type is almost due to incomplete resolution of hematoma. But, the reoperative cases due to incomplete resolution were excluded in our study. Because, we defined recurrence as reaccumulation of hematoma on the operated side after previous complete resolution. An identical conception in a definition of recurrence is going to be needed for deduction of accurate risk factors.
Recurrence of CSDHs generally occurs more in the elderly and male patients group. That was explained by a capacity of brain re-expansion. Age and sex are not statistically significant in almost articles.2,4,7,8,9,10,11,16,17,18,20,23,25,29) In the present study, elderly male patients also had a higher recurrence rate, but there are not statistically significant.
HTN and DM have been considered to be risk factors of recurrence in previous study. They related to recurrence of CSDHs in this study (p=0.010, p=0.011). In most previous literatures, HTN was not significant for a recurrence factor.4,8,9,11,16,25,29) But, DM was a significant risk factor of recurrence of CSDHs in several articles. Yamamoto et al.,29) recurrence rate of patients without DM had a higher recurrence rate than those with DM. They asserted that DM decreases rebleeding in CSDH patients, because the blood of patients with DM has a hyperviscosity, high osmotic pressure and increased platelet aggregation. In contrast to this result, DM may play a role in recurrence of CSDHs in several articles. Exudate of macrocapillaries in the outer membrane had an influence on recurrence of CSDH.4,24,25) The significance of HTN and DM as an independent risk factor for recurrence are still controversial.
Drainage tube removal time can be taken into consideration as a predicting factor of recurrence of CSDHs. Drainage tube removal within 24 hours is an independent risk factor of recurrence of CSDHs in this study (p=0.004). In the results of Oh et al.,20) patients who underwent removal of drainage within 24 hours had a higher recurrence rate than the other patients, but there are not statistically significant (p=0.192). Early drainage tube removal is necessary for to reduce an incidence of infection. But, too early removal of drainage tube can cause reaccumulation of subdural hematoma. The drainage tube removal time should be decided with due regard to amount of drainage and color of drainage fluid. An ideal time of drainage removal is controversial.
There are a few limitations of this study. The present study was a small size retrospective study, and follow-up period was a bit short. There are some sources of bias and limitation. But, the results of this study are enough significant by look at that almost results are similar to previous articles. We also conducted a univariate logistic regression study for accurate results. The results are same in the analysis (Table 6).
Go to : 
There are some differences among the previous articles and our study. These differences are due to several different limitations in these studies. So, a cooperative study of various hospitals and a large well-defined prospective study should be needed in the future. In accordance with our results, the heterogeneous type hematoma and the bilaterality are the significant recurrent factors in preoperative CT findings. If predicting factors related to recurrence will been displayed on preoperative brain CT, the more deliberate surgical consideration will have to be needed. And, the postoperative care such as drainage tube removal is also important to reduce the recurrence rate of CSDHs.
Go to : 
Notes
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST)(No. 2011-0030075).
Go to : 
References
1. Abouzari M, Rashidi A, Rezaii J, Esfandiari K, Asadollahi M, Aleali H, et al. The role of postoperative patient posture in the recurrence of traumatic chronic subdural hematoma after burr-hole surgery. Neurosurgery. 2007; 61:794–797. discussion 797. PMID: 17986941.

2. Ahn SY, Kim JH, Ha SK, Kim JH, Kwon TH, Park YK, et al. Clinical analysis of risk factors associated with the recurrence of chronic subdural hematoma. J Korean Neurotraumatol Soc. 2011; 7:68–73.

3. Arbit E, Patterson RH Jr, Fraser RA. An implantable subdural drain for treatment of chronic subdural hematoma. Surg Neurol. 1981; 15:175–177. PMID: 7221864.

4. Chon KH, Lee JM, Koh EJ, Choi HY. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir (Wien). 2012; 154:1541–1548. PMID: 22653496.

5. Ernestus RI, Beldzinski P, Lanfermann H, Klug N. Chronic subdural hematoma: surgical treatment and outcome in 104 patients. Surg Neurol. 1997; 48:220–225. PMID: 9290707.

6. Horn EM, Feiz-Erfan I, Bristol RE, Spetzler RF, Harrington TR. Bedside twist drill craniostomy for chronic subdural hematoma: a comparative study. Surg Neurol. 2006; 65:150–153. discussion 153-154. PMID: 16427409.

7. Kang MS, Koh HS, Kwon HJ, Choi SW, Kim SH, Youm JY. Factors influencing recurrent chronic subdural hematoma after surgery. J Korean Neurosurg Soc. 2007; 41:11–15.
8. Kim HS, Heo W, Cha JH, Song JS, Rhee DY. Factor affecting recurrence of chronic subdural hematoma after burr-hole drainage. Korean J Neurotrauma. 2012; 8:73–78.

9. Kim SG, Yang JC, Kim TW, Park KH. Factors that influence to chronic subdural hematoma recurrence. Korean J Neurotrauma. 2013; 9:81–86.

10. Ko BS, Lee JK, Seo BR, Moon SJ, Kim JH, Kim SH. Clinical analysis of risk factors related to recurrent chronic subdural hematoma. J Korean Neurosurg Soc. 2008; 43:11–15. PMID: 19096538.

11. Kong WK, Kim BC, Cho KT, Hong SK. Factors affecting postoperative recurrence of chronic subdural hematoma. Korean J Neurotrauma. 2012; 8:122–127.

12. Kotwica Z, Brzeziński J. Chronic subdural haematoma treated by burr holes and closed system drainage: personal experience in 131 patients. Br J Neurosurg. 1991; 5:461–465. PMID: 1764227.

13. Lee JY, Ebel H, Ernestus RI, Klug N. Various surgical treatments of chronic subdural hematoma and outcome in 172 patients: is membranectomy necessary? Surg Neurol. 2004; 61:523–527. discussion 527-528. PMID: 15165784.

14. Mellergård P, Wisten O. Operations and re-operations for chronic subdural haematomas during a 25-year period in a well defined population. Acta Neurochir (Wien). 1996; 138:708–713. PMID: 8836286.
15. Mohamed EE. Chronic subdural haematoma treated by craniotomy, durectomy, outer membranectomy and subgaleal suction drainage. Personal experience in 39 patients. Br J Neurosurg. 2003; 17:244–247. PMID: 14565521.

16. Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001; 41:371–381. PMID: 11561347.

17. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001; 95:256–262. PMID: 11780895.

18. Nayil K, Ramzan A, Sajad A, Zahoor S, Wani A, Nizami F, et al. Subdural hematomas: an analysis of 1181 Kashmiri patients. World Neurosurg. 2012; 77:103–110. PMID: 22405391.

19. Nomura S, Kashiwagi S, Fujisawa H, Ito H, Nakamura K. Characterization of local hyperfibrinolysis in chronic subdural hematomas by SDS-PAGE and immunoblot. J Neurosurg. 1994; 81:910–913. PMID: 7965121.

20. Oh HJ, Lee KS, Shim JJ, Yoon SM, Yun IG, Bae HG. Postoperative course and recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2010; 48:518–523. PMID: 21430978.

21. Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, et al. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet. 2009; 374:1067–1073. PMID: 19782872.

22. Smely C, Madlinger A, Scheremet R. Chronic subdural haematoma--a comparison of two different treatment modalities. Acta Neurochir (Wien). 1997; 139:818–825. discussion 825-826. PMID: 9351986.
23. Stanisic M, Lund-Johansen M, Mahesparan R. Treatment of chronic subdural hematoma by burr-hole craniostomy in adults: influence of some factors on postoperative recurrence. Acta Neurochir (Wien). 2005; 147:1249–1256. PMID: 16133770.

24. Tokmak M, Iplikcioglu AC, Bek S, Gökduman CA, Erdal M. The role of exudation in chronic subdural hematomas. J Neurosurg. 2007; 107:290–295. PMID: 17695382.

25. Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S. Independent predictors for recurrence of chronic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery. 2008; 63:1125–1129. discussion 1129. PMID: 19008766.
26. Tsutsumi K, Maeda K, Iijima A, Usui M, Okada Y, Kirino T. The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg. 1997; 87:870–875. PMID: 9384397.

27. Wakai S, Hashimoto K, Watanabe N, Inoh S, Ochiai C, Nagai M. Efficacy of closed-system drainage in treating chronic subdural hematoma: a prospective comparative study. Neurosurgery. 1990; 26:771–773. PMID: 2352594.

28. Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 2003; 74:937–943. PMID: 12810784.

29. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003; 98:1217–1221. PMID: 12816267.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download