Abstract
Objective
The intracranial pathologies after head trauma should be usually progressed. It is clearly visualized in the non-invasive brain CT. The invasive monitor such as intracranial pressure (ICP) monitoring may be accompanied with the complications. This study aims whether the patients with severe head injury could be managed with serial CT scans.
Methods
The medical records of 113 patients with severe head injury in the prospectively enrolled trauma bank were retrospectively analyzed. After the emergency care, all the patients were admitted to the intensive care unit for the aggressive medical managements. Repeat brain CT scans were routinely taken at 6 hours and 48 hours after the trauma. ICP monitoring was restrictively applied for the uncertain intracranial pressure based on the CT. The surgical intervention and the mortality rate were analyzed.
Results
Immediate surgical intervention after the initial CT scan was done in 47 patients. Among the initially non-surgical patients, 59 patients were managed with the serial CT scans and 7 with the ICP monitoring. Surgical interventions underwent eventually for 10 patients in the initially non-surgical patients; 1 in the ICP monitoring and 9 in the serial CT. The mortality rate was 23.7% in the serial brain CT and 28.6% in the ICP monitoring. There was no statistical difference between two groups in the aspect of mortality (p=0.33).
Monitoring and targeted management of intracranial pressure (ICP) are widely advocated for the patients with severe head injuries. Brain Trauma Foundation (BTF) recently announced that ICP monitoring is considered to be the standard procedure in comatose patients who have sustained severe head injury.4) However, several studies have demonstrated inconsistent compliance with BTF guidelines for ICP monitoring22) and there were no evidence that such management resulted in improving functional outcome.5,15) Moreover, ICP monitoring has complications like ventriculitis and hemorrhage.1,2,6,9,12,17,23)
Because of short scan time, non-invasive technique, and good resolution, brain CT scan is the diagnostic standard for head trauma to evaluate intracranial pathologies. And it is also useful to predict the outcome and decide the management plan.14,18,21,22) Surgical interventions, such as decompressive craniectomy or craniotomy with hematoma evacuation, should be decided in the basis of the CT findings. Repeat CT scans have been published that it gives valuable information to know the progression of intracranial pathologies.14,21,22) As the intracranial lesions are usually progressing, timely identification of intracranial changes would be very important for managing the patients. The aim of the study is to investigate that serial CT scans without the invasive ICP monitoring could be applied for the management in severe head injuries.
Patients in severe head injury (Glasgow Coma Scale ≤8) were retrieved in a prospectively enrolled database of head trauma for a 3-year period. One-hundred thirteen patients were included for this study designed for the retrospective analysis of acute severe head injuries. All the patients were admitted at the intensive care unit and got the aggressive medical care including intubation, fluid therapy, hyperosmolar agents (mostly mannitol), and monitors for vital signs.
All the patients were taken for the initial brain CT at the emergency room. And then repeat brain CT scans were routinely followed in the 6-hour and 48-hour after the trauma. In our policy of serial brain CT scans, the 6-hour one was for detecting acute progression of intracranial hematomas and the 48-hour one for global evaluation of intracranial condition such as the brain swelling. Decompressive surgery was performed in anytime if indicated; 1) obliteration of basal cisterns in the CT scan, 2) midline shift ≥10 mm in the CT scan, and 3) any neurologic signs for transtentorial herniation. Severe head injuries of 113 patients was enrolled in this study. Among all the patients, 47 patients got an immediate surgical craniotomy or craniectomy after initial brain CT. The patients who were not immediately operated were monitored with ICP monitoring or serial brain CT. ICP monitoring was not a preferred procedure for the severe head injuries. Serial brain CT was preferred for knowing the intracranial status or detecting progressive pathologies. ICP monitoring was restrictively done only for the patients not confident of the intracranial pressure based on the brain CT. The parenchymal ICP monitoring catheter (Camino®, Intergra LifeScience Corp., Plainsboro, NJ, USA) was placed with a usual manner of manufacture's recommendations.
The patients were divided into two groups: the serial CT scanning group and the ICP monitoring group. We analyzed the surgical intervention such as decompressive craniectomy and/or hematoma evacuation and mortality at 3 months after trauma in both groups. Fisher exact test was used for the statistical analysis.
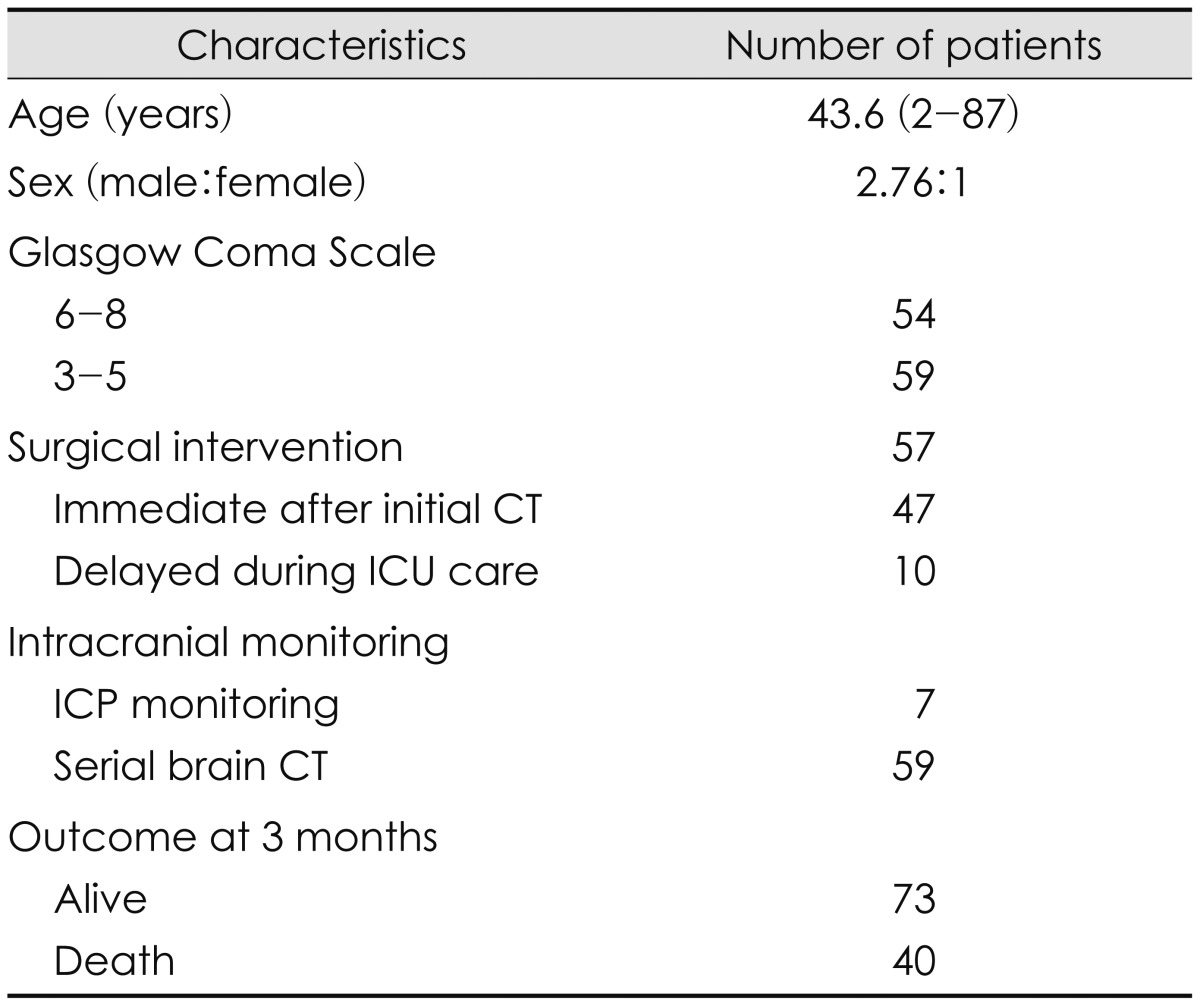
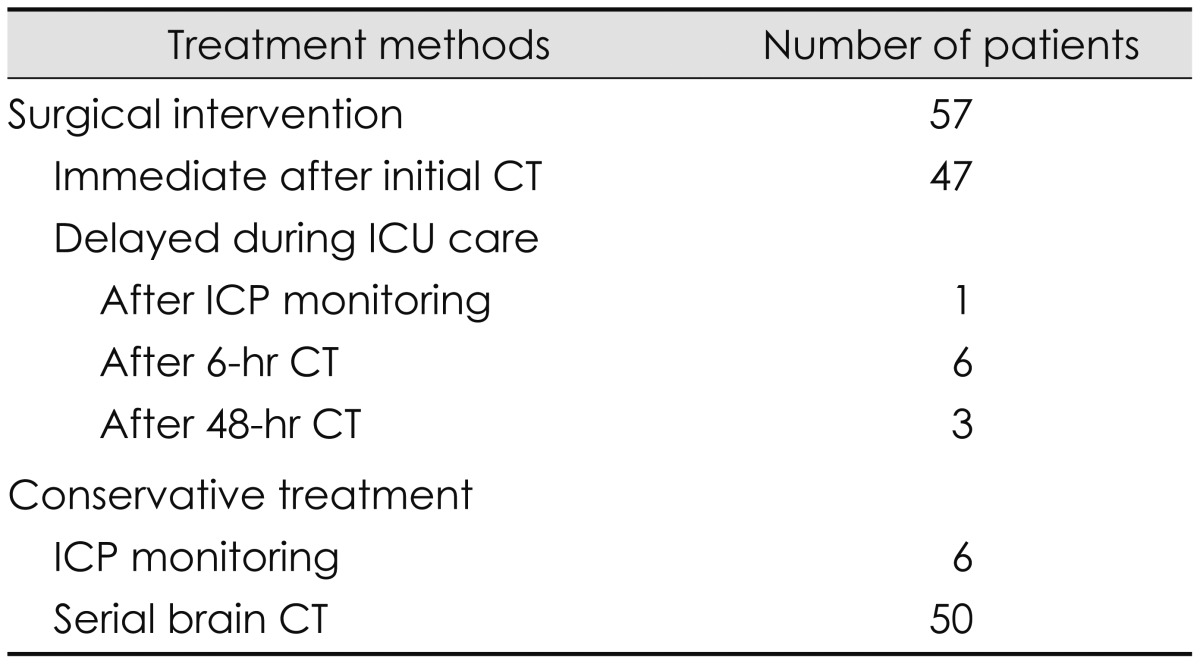
In 113 patients, there were 83 male and 30 females, ranging from 2 to 87 years (median; 43.6 years). Immediate surgical intervention after the initial CT scan was done in 47 patients (Table 1). Intracranial hematoma evacuation and only craniectomy was performed to control the intracranial pressure in these surgical patients. The immediate surgical cases were not assigned ether two groups. Among the non-surgical patients, aggressive medical managements were applied as the serial CT scanning group in 59 patients and the ICP monitoring group in 7 patients (Table 1). The serial brain CT was also taken in the patients for ICP monitoring.
Surgical interventions were done in 10 patients who were initially managed with medical treatment in the intensive care unit (ICU). Among the ICP monitoring group, only 1 patient got a decompressive craniectomy immediately after inserting the ICP monitor. Nine patients underwent decompressive surgery in the serial CT group (Table 2). Among them, 6 patients had operations after 6-hr CT scan and 3 patients after 48-hr CT scan. In the 6 operations after 6-hr CT, hematoma expansions were main cause of the surgery and 1 case was neurologically deteriorated just before 6-hr CT was taken.
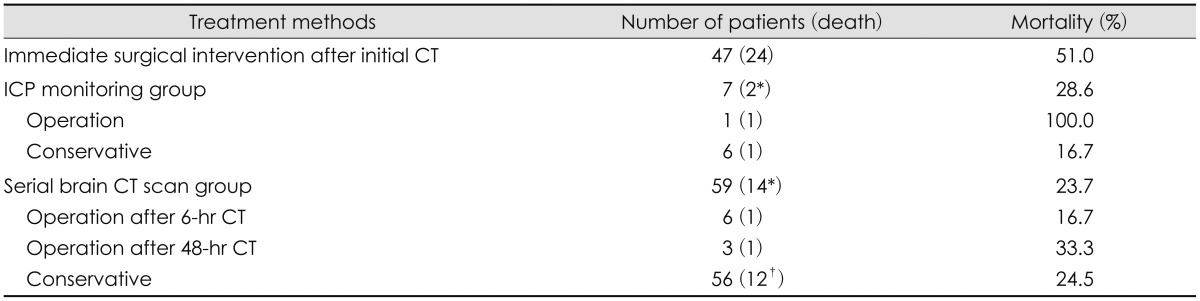
The mortality rate was 35.5% (40 in 113 of all the patients). Most of death happen in the patients for an immediate surgical intervention and fully comatose at the initial evaluation (Table 3). The mortality was 2 of 7 in the ICP monitoring group (28.6%) and 14 of 59 in the serial brain CT group (23.7%). There was no statistical difference of the mortality between two groups (p=0.33, Fisher exact test).
Elevation of ICP had been recognized as the most important factor affecting outcome in patients who have had the severe head injury and ICP monitoring has become standard procedure in the management of severe head injury patients.3,19) The BTF guidelines recommend the ICP monitoring in all salvageable patients with severe head injury. However, compliance with BTF guidelines was only 45.8% and patients with subarachnoid hemorrhage and those who underwent craniectomy/craniotomy were significantly more likely to undergo ICP monitoring.22) And the BTF ICP guidelines improved patient survival in this report. But, the treating physician's decision was the most common reason for not placing an ICP monitoring device. The compliance for implanting the ICP monitoring was relatively low and ICP monitoring devices tended to be placed in the surgical patients, not in initially medical-managed patients. They did not mentioned how to detect the ICP changes with non-invasive methods such as serial brain CT scans.
Even though the ICP monitoring may improve survival, it did not make better functional outcome in severe head injury.5,15) ICP/cerebral perfusion pressure (CPP) targeted intensive care resulted in prolonged mechanical ventilation and increased levels of therapy intensity, without evidence for improved outcome in patients who survive beyond 24 hrs following severe head injury.5) And it was impossible to predict need for ICP/CPP-guided therapy from clinical features at presentation.15) However, they concluded specialist critical care with ICP/CPP-guided therapy may benefit patients with severe head injury. In the management of severe head injury, ICP monitoring did not show improvement of the functional outcome but rather increase the costs and ICU stays. So, survival itself could be said a main reason to determine the initial management in the severe head injury. The ICP monitoring has been recommended in the severe head injury, but it has not proved whether it results in better functional outcome. Moreover, the outcome of the patients with severe head injury has been known as dismal. Functional recovery is usually poor. So, the primary goal of the management should get a rescue from dying. We just focused the mortality between two different monitoring methods in this study.
As the invasive procedure is accompanied with the complications, the ICP monitoring makes procedure-related side-effects.1,2,6,12,17) The most common complication is infection and intracranial bleeding.1,17) Intraventricular device has more hemorrhagic complication compared with intraparenchymal fiberoptic monitor.1) Infection rate was 2.2%.17) No complication was reported in the subdural ICP monitoring.10)
Brain CT scans are definitely standard diagnostic modality for assessing head injury patients. Repeated brain CT should be required clearly when patients show deteriorating neurologic signs. And physicians tend usually to decide the operations based on brain CT scan.16) Although the situation meets that ICP/CCP values are the cause of worsening the neurological deterioration in the severe head injury, physician would take the brain CT scan to decide a surgical plan before the surgery is performed. So, it could be said that usefulness of CT scanning is not disappearing on ICP monitored situation. But, transferral to CT room may miss the changes of neurologic deterioration and vital signs.
Progressive intracranial hemorrhage after head injury is often observed on serial CT scans.13,14,20,21) The expansion of traumatic intracerebral hematomas between the baseline and 24-hr CT scans occurred in approximately half of the subjects.13) The earlier after injury that the initial CT scan is obtained, the greater is the likelihood that the hematoma will expand on subsequent scans. So, the timing of the first CT scan is clearly important factor to predict the intracranial progression. In the spontaneous intracerebral hematomas, frequency of hematoma expansion is greatest among those who underwent the initial CT scan early and progressively declined as the time to initial scan is prolonged.11) Enlargement after 24 hours of onset seems extremely rare. Even though no deterioration of neurologic, clinical, and vital signs is detected, intracranial changes could be found in the routine CT scans.14) The findings in the routine CT scan may help predict the injury progression and determine the management plans.
It is very important to decide the optimal time to get the serial brain CT scans. Our protocol for the serial CT scans was that brain CT scans were taken at the emergency room and then followed in the 6-hour and 48-hour after the trauma. The 6-hour one was for detecting acute progression of intracranial hematomas and the 48-hour one for global evaluation of intracranial condition such as brain swelling or ischemic change. As mentioned earlier, the intracranial hemorrhages did not usually grow after 24 hours of onset. So, earlier follow-up CT would be very important. But, we suggest that 2 hr interval after the initial CT be too early to detect the intracranial progression. This may miss the progression or make one more scan to verify the more aggravation. In our results, 9 patients of the serial CT scan group underwent surgical interventions. Six of them got the operation after 6-hr CT and 3 after 48-hr CT. The result supported that CT scan after 24-hr of the trauma should be taken for detecting the intracranial progression such as brain swelling. In severe head-injured patients who are non-neurosurgical candidates on the basis of initial and 24-hr to 48-hr repeat CT scans, serial head CT scans had little clinical efficacy and did not lead to urgent operative intervention.8) So, routine CT scan may not be needed after 48-hr of the trauma. And the patients with routine-repeat CT scans fared better than did the non-routine-repeat CT group.7) This procedure of routine-repeat CT scans demonstrated a significant effect on patients with moderate and severe head injury. We could not say what time is optimal to get serial CT scans in the severe head injury. Our protocol may be suitable even though the patient does not show any neurologic deterioration. If the patient is worsening the neurologic condition, the urgent CT is mandatory.
In the present study, we have described the feasibility of the serial brain CT scans in the aspect of the patient management in the severe head injury. This study has several limitations. First, this is a retrospective analysis even though the cases were enrolled prospectively. Second, the number of patients was small to make a firm evidence of how to manage the patients. Although total number of the study was 113 of severe head injury, actual cases for analysis was only 66 to be assigned in the serial CT group and the ICP monitoring group. It is hard to be generalized for all the severe head injuries. Third, no definite indication for placing ICP monitoring was designed before the patient enrollment. So, it had an inevitable selection bias. As many factors affect the outcome and mortality of severe head injuries, it could not say that only the monitoring makes change the mortality like this study.
In summary, serial brain CT scans in time is useful way to be applied for the severe head injuries. And it could reduce the unnecessary implantation of an invasive ICP monitoring device. If brain CT give ambiguous findings for assuming elevated ICP, ICP monitoring is mandatory to determine the proper management. But, timely serial brain CT would be recommended in no obliteration of basal cisterns, no effacement of cortical sulci, and midline shifting less than 5 mm in the initial brain CT. And in the case that main pathology is the intracranial hematoma without brain edema, it is also a good candidate for the serial brain CT scans. But, it should be cautious that only serial CT scans without ICP monitoring is not applicable to all the severe head injuries.
Serial brain CT scans in time could be a good way to monitor the progression of the intracranial pathologies and reduce chances of implanting an invasive ICP probe. The time interval for serial scans may be optimal in 6 hours and 48 hours after the trauma even though the patients do not show any neurologic deterioration.
References
1. Anderson RC, Kan P, Klimo P, Brockmeyer DL, Walker ML, Kestle JR. Complications of intracranial pressure monitoring in children with head trauma. J Neurosurg. 2004; 101(1 Suppl):53–58. PMID: 16206972.

2. Blaha M, Lazar D, Winn RH, Ghatan S. Hemorrhagic complications of intracranial pressure monitors in children. Pediatr Neurosurg. 2003; 39:27–31. PMID: 12784075.

3. Brain Trauma Foundation. American Association of Neurological Surgeons. Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007; 24(Suppl 1):S1–S106.
4. Brain Trauma Foundation. American Association of Neurological Surgeons. Congress of Neurological Surgeons. Joint Section on Neurotrauma and Critical Care, AANS/CNS. Bratton SL, et al. Guidelines for the management of severe traumatic brain injury VIII Intracranial pressure thresholds. J Neurotrauma. 2007; 24(Suppl 1):S55–S58. PMID: 17511546.
5. Cremer OL, van Dijk GW, van Wensen E, Brekelmans GJ, Moons KG, Leenen LP, et al. Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med. 2005; 33:2207–2213. PMID: 16215372.

6. Davis JW, Davis IC, Bennink LD, Hysell SE, Curtis BV, Kaups KL, et al. Placement of intracranial pressure monitors: are "normal" coagulation parameters necessary? J Trauma. 2004; 57:1173–1177. PMID: 15625446.

7. Ding J, Yuan F, Guo Y, Chen SW, Gao WW, Wang G, et al. A prospective clinical study of routine repeat computed tomography (CT) after traumatic brain injury (TBI). Brain Inj. 2012; 26:1211–1216. PMID: 22571813.

8. Figg RE, Burry TS, Vander Kolk WE. Clinical efficacy of serial computed tomographic scanning in severe closed head injury patients. J Trauma. 2003; 55:1061–1064. PMID: 14676651.
9. Guyot LL, Dowling C, Diaz FG, Michael DB. Cerebral monitoring devices: analysis of complications. Acta Neurochir Suppl. 1998; 71:47–49. PMID: 9779141.

10. Hong WC, Tu YK, Chen YS, Lien LM, Huang SJ. Subdural intracranial pressure monitoring in severe head injury: clinical experience with the Codman MicroSensor. Surg Neurol. 2006; 66(Suppl 2):S8–S13. PMID: 17071260.

11. Kazui S, Naritomi H, Yamamoto H, Sawada T, Yamaguchi T. Enlargement of spontaneous intracerebral hemorrhage. Incidence and time course. Stroke. 1996; 27:1783–1787. PMID: 8841330.
12. Khan SH, Kureshi IU, Mulgrew T, Ho SY, Onyiuke HC. Comparison of percutaneous ventriculostomies and intraparenchymal monitor: a retrospective evaluation of 156 patients. Acta Neurochir Suppl. 1998; 71:50–52. PMID: 9779142.

13. Narayan RK, Maas AI, Servadei F, Skolnick BE, Tillinger MN, Marshall LF, et al. Progression of traumatic intracerebral hemorrhage: a prospective observational study. J Neurotrauma. 2008; 25:629–639. PMID: 18491950.

14. Oertel M, Kelly DF, McArthur D, Boscardin WJ, Glenn TC, Lee JH, et al. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg. 2002; 96:109–116. PMID: 11794591.

15. Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med. 2002; 28:547–553. PMID: 12029400.

16. Patel NY, Hoyt DB, Nakaji P, Marshall L, Holbrook T, Coimbra R, et al. Traumatic brain injury: patterns of failure of nonoperative management. J Trauma. 2000; 48:367–374. discussion 374-375. PMID: 10744271.

17. Rossi S, Buzzi F, Paparella A, Mainini P, Stocchetti N. Complications and safety associated with ICP monitoring: a study of 542 patients. Acta Neurochir Suppl. 1998; 71:91–93. PMID: 9779154.

18. Servadei F, Nasi MT, Giuliani G, Cremonini AM, Cenni P, Zappi D, et al. CT prognostic factors in acute subdural haematomas: the value of the 'worst' CT scan. Br J Neurosurg. 2000; 14:110–116. PMID: 10889882.
19. Society of Critical Care Medicine. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Crit Care Med. 2003; 31(6 Suppl):S407–S491.
20. Stein SC, Spettell C, Young G, Ross SE. Delayed and progressive brain injury in closed-head trauma: radiological demonstration. Neurosurgery. 1993; 32:25–30. discussion 30-31. PMID: 8421553.
21. Tabori U, Kornecki A, Sofer S, Constantini S, Paret G, Beck R, et al. Repeat computed tomographic scan within 24-48 hours of admission in children with moderate and severe head trauma. Crit Care Med. 2000; 28:840–844. PMID: 10752839.

22. Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H, et al. Intracranial pressure monitoring in severe head injury: compliance with Brain Trauma Foundation guidelines and effect on outcomes: a prospective study. J Neurosurg. 2013; 119:1248–1254. PMID: 23971954.

23. Zingale A, Ippolito S, Pappalardo P, Chibbaro S, Amoroso R. Infections and re-infections in long-term external ventricular drainage. A variation upon a theme. J Neurosurg Sci. 1999; 43:125–132. discussion 133. PMID: 10735766.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download