Abstract
Encapsulated acute subdural hematoma (ASDH) has been uncommonly reported. To our knowledge, a few cases of lentiform ASDH have been reported. The mechanism of encapsulated ASDH has been studied but not completely clarified. Encapsulated lentiform ASDH on a computed tomography (CT) scan mimics acute epidural hematoma (AEDH). Misinterpretation of biconvex-shaped ASDH on CT scan as AEDH often occurs and is usually identified by neurosurgical intervention. We report a case of an 85-year-old man presenting with a 2-day history of mental deterioration and right-sided weakness. CT scan revealed a biconvex-shaped hyperdense mass mixed with various densities of blood along the left temporoparietal cerebral convexity, which was misinterpreted as AEDH preoperatively. Emergency craniectomy was performed, but no AEDH was found beneath the skull. In the subdural space, encapsulated ASDH was located. En block resection of encapsulated ASDH was done. Emergency craniectomy confirmed that the preoperatively diagnosed AEDH was an encapsulated ASDH postoperatively. Radiologic studies of AEDH-like SDH allow us to establish an easy differential diagnosis between AEDH and ASDH by distinct features. More histological studies will provide us information on the mechanism underlying encapsulated ASDH.
Acute subdural hematoma (ASDH) generally appears on computed tomography (CT) scan as a crescent-shaped high-density lesion, while acute epidural hematoma (AEDH) as a high-density lentiform lesion. The reported mechanism underlying subdural membrane formation is the result of proliferation and excessive thickening of the normal layer of dural border cells. Multilayered subdural membranes formed by dural border cells are cleaved by capillaries, collagen fibrils, and elastic fibers.1) Pathological mechanisms underlying lentiform ASDH have not yet been clarified. However, rupture of capillaries transfixing the subdural membrane make cracks between layers.4) Hematomas originating between the inner and outer layers are frequently biconvex-shaped. Encapsulated ASDH mimicking AEDH on a brain CT has rarely been reported.6) CT scan can lead to a misdiagnosis of encapsulated ASDH as AEDH. We herein report a case with AEDH-like appearance on a CT scan, which was confirmed as an encapsulated ASDH with unresolved chronic subdural hematoma (CSDH) during surgery.
An 85-year-old man presented with a 2-day history of mental deterioration and right-sided weakness. He had been admitted to a geriatric hospital for several years. In the geriatric hospital, the patient had often sustained minor head traumas due to weakness of both legs. There was neither external wound nor swelling on his scalp. His Glasgow coma scale score was 14 points. Right hemiparesis with a motor strength grade of 4 points was checked. He had undergone burr hole trephination and drainage for CSDH on the left cerebral convexity 4 years prior. At that time, incomplete resolution of CSDH was observed on a brain CT (Figure 1A). A newly developed AEDH was found near the burr hole site. Also, he had a medical history of Parkinson's disease and vascular dementia. However, he took neither antiplatelet nor anticoagulative agents. On a brain CT scan, a lentiform lesion in the left temporoparietal cerebral convexity showed high density partially mixed isodensity to low density (Figure 1B). AEDH was undoubtedly diagnosed by CT scan preoperatively. Emergency decompressive craniectomy and arcuately opened the dura and revealed a large lump of encapsulated ASDH along with unresolved CSDH instead of AEDH. No bleeding point was found. The encapsulated ASDH had the following structures: 1) an outer thick white-yellowish membrane covered with macroscopically not so plentiful vascular structures on the dural surface, 2) an inner thin membrane easily separated from the arachnoid membrane on the arachnoidal surface, and 3) a large amount of solid fresh blood clots with dark red and mud-like hematoma between them. The arachnoid mater and brain parenchyma were intact (Figure 2). Both layers of the capsule were easily dissected from the dura and arachnoid mater. Complete en bloc resection of the encapsulated ASDH was done. No feeding vessels of the encapsulated hematoma were found. After en bloc resection, no active bleeding was seen in the subdural space on a postoperative CT scan, the encapsulated ASDH was completely removed, and an intracranial hematoma was newly developed in the interhemispheric area (Figure 1C). His postoperative neurologic symptoms did not improve. His family (sons and daughters) did not consent to aggressive postoperative management, and then he was transferred to the geriatric hospital.
To our knowledge, 9 cases of encapsulated ASDH mimicking AEDH have been reported in the literature. Multiple densities of CSDH may result from multiple episodes of trauma.8) In the CT scan of our patient, a biconvex-shaped hematoma showed high density partially mixed with low density. CT scan allows clinicians to make a diagnosis of AEDH before surgery.
Although hematomas appear biconvex-shaped on CT scan, ASDH usually has 4 characteristic features: a crescentic tail, an obtuse angle at the margin of the hematoma, a dural line above the hematoma, and a direct connection to the underlying intracerebral hematomas.10) In our case, however, we could not find the features on CT scan.
CSDH after burr hole trephination shows complete improvement in clinical symptoms or a low incidence of recurrence. Most cases of recurrent CSDH show liquefaction of hematoma.9) The resolution rate of CSDH within 3 months after burr hole drainage is reported to be 88% of all cases, and the late recurrence of CSDH can be defined as reappearance of a liquefied hematoma beyond 3 months after surgery.7) In our case, however, CSDH appeared as the dry and mud-like solid mass within the encapsulated ASDH. There have been a few cases of CSDH developing a solid structure due to the penetration of fibroblasts that replaced the fibrin meshwork of the hematoma by collagen fibrils.11)
Mechanisms underlying subdural neomembranes have been investigated and reported. In unresolved subdural hematoma or subdural hygroma, dural border cells proliferate and form subdural neomembranes.2) Proliferation of subdural neomembranes is inevitably combined with angiogenesis. Already matured subdural neomembranes and neocapillaries are not involved in subdural hematoma growth. However, interactions between the components of the outer subdural membrane and CSDH fluid contribute to the growth of the outer membrane and recurrent hemorrhage.4)
In our case, the patient had a 4-year history of burr hole trephination and drainage for CSDH in the left cerebral hemisphere. Although hematoma contents could have important factors for the growth of CSDH,12) the most important factor for the development of CSDH is vessels within capsules, which have a marked proliferation potential and a fragile nature.11) Unresolved subdural hygroma may become CSDH by repeated microhemorrhagic events from fragile new vessels which have grown into neomembranes.5)
In our case, the patient's neurologic symptoms were not aggravated until a new head trauma was sustained because a small amount of the encapsulated CSDH had no mass effect on the brain. Several head traumas could influence the maturation of subdural neomembranes and capillaries through the mechanism underlying most cases of ASDH. A newly developed hematoma within the encapsulated ASDH seemed to cause mental deterioration and right hemiparesis.
Although emergency decompressive craniectomy revealed encapsulated ASDH mixed with solid CSDH, en block resection of the lesion showed no bleeding vessels on the inner or outer surface of the subdural membrane. The encapsulated ASDH may have originated from ruptured capillaries between the multiple layers of the subdural membrane, as the majority cases of ASDH originate from ruptured bridging veins.
Histological findings are shown in Figure 3. The outer subdural membrane is composed of hyaline degeneration tissue with rich vascularity formed by the dura mater, and the inner subdural membrane is composed of thin fibrous tissue with hemosiderin pigments produced by old hemorrhage. A few dural border cells induce thin inner subdural membrane on underlying arachnoid membrane.3) Histological findings provided the following information: the origin of bleeding, characteristic composition of a new membrane, and mechanisms of encapsulated ASDH mimicking AEDH. Further clinical studies are warranted.
References
1. Friede RL. Incidence and distribution of neomembranes of dura mater. J Neurol Neurosurg Psychiatry. 1971; 34:439–446. PMID: 5096558.

2. Friede RL, Schachenmayr W. The origin ofsubdural neomembranes. II. Fine structural of neomembranes. Am J Pathol. 1978; 92:69–84. PMID: 686149.
3. Kawano N, Endo M, Saito M, Yada K. [Origin of the capsule of a chronic subdural hematoma--an electron microscopy study]. No Shinkei Geka. 1988; 16:747–752. PMID: 3412561.
4. Killeffer JA, Killeffer FA, Schochet SS. The outer neomembrane of chronic subdural hematoma. Neurosurg Clin N Am. 2000; 11:407–412. PMID: 10918009.

5. Lee KS. Natural history of chronic subdural haematoma. Brain Inj. 2004; 18:351–358. PMID: 14742149.
6. Miki S, Fujita K, Katayama W, Sato M, Kamezaki T, Matsumura A, et al. Encapsulated acute subdural hematoma mimicking acute epidural hematoma on computed tomography. Neurol Med Chir (Tokyo). 2012; 52:826–828. PMID: 23183078.

7. Oh HJ, Lee KS, Shim JJ, Yoon SM, Yun IG, Bae HG. Postoperative course and recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2010; 48:518–523. PMID: 21430978.

8. Park HR, Lee KS, Shim JJ, Yoon SM, Bae HG, Doh JW. Multiple Densities of the Chronic Subdural Hematoma in CT Scans. J Korean Neurosurg Soc. 2013; 54:38–41. PMID: 24044079.

9. Prieto R, Pascual JM, Subhi-Issa I, Yus M. Acute epidural-like appearance of an encapsulated solid non-organized chronic subdural hematoma. Neurol Med Chir (Tokyo). 2010; 50:990–994. PMID: 21123983.
10. Su IC, Wang KC, Huang SH, Li CH, Kuo LT, Lee JE, et al. Differential CT features of acute lentiform subdural hematoma and epidural hematoma. Clin Neurol Neurosurg. 2010; 112:552–556. PMID: 20483531.

11. Yamashima T, Yamamoto S. How do vessels proliferate in the capsule of a chronic subdural hematoma? Neurosurgery. 1984; 15:672–678. PMID: 6209593.

12. Yatsuzuka H. [Growing factors of chronic subdural hematoma--significance of CK activity in hematoma contents and neomembrane]. No To Shinkei. 1988; 40:963–969. PMID: 3196500.
FIGURE 1
A: Incompletely resolved chronic subdural hematoma after burr hole trephination 4 years prior to admission. A thick-walled isodense lesion is seen in the left temporoparietal cerebral convexity. B: Preoperative computed tomography scan shows a lentiform lesion (8×3.8 cm) with high density partially mixed with isodensity to low density, in the left temporoparietal cerebral convexity. Large amounts of subdural fluid collection along both cerebral convexities are seen. C: Postoperative CT scan shows a newly developed hematoma. An acute subdural hematoma along the interhemispheric fissure and left cerebral convexity is seen.
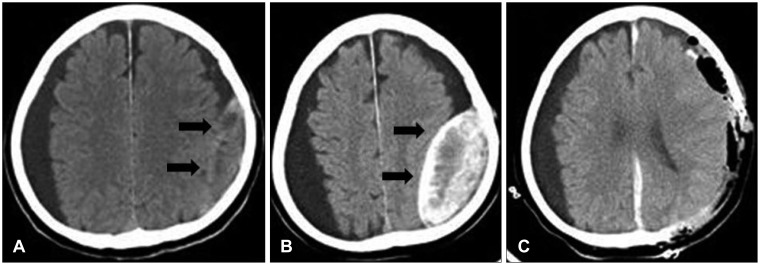
FIGURE 2
Photograph of the encapsulated hematoma in the subdural space shows the dura mater (thin black arrow), outer/inner neomembrane (thick black arrow), solid fresh blood clots with old mud-like blood clots (white arrow), and an intact brain parenchyma.
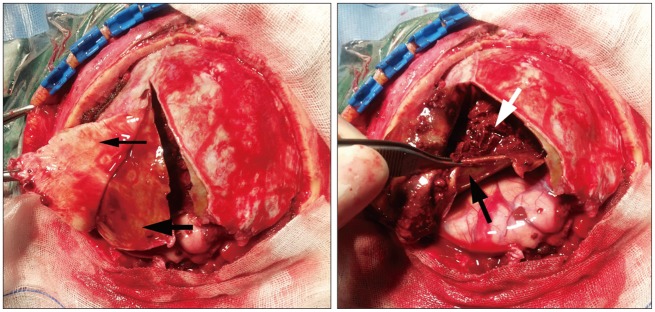
FIGURE 3
Photograph of resected hematoma. The thick outer neomembrane shows hyaline degeneration, and the thin inner membrane has meningothelial cells and hemosiderin pigments produced by old hemorrhage. A: The dura membrane has plentiful vascular structures (arrow). B: Hemosiderin pigments (arrow). C: Meningothelial cells (arrow). Hematoxylin and eosin staining. Original magnifications are marked by bars.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download