This article has been
cited by other articles in ScienceCentral.
Abstract
Increasing use of the nail gun has led to higher injury rates from the use of tools with sequential actuation. Nail gun injury can occur to various parts of the body. Very deep penetration in the brain can have fatal results. A 46-year-old male fired shots from a nail gun into his brain in a suicide attempt. This case demonstrated successful surgical management of the resultant open head injury.
Go to :

Keywords: Head injuries penetrating, Craniocerebral trauma, Brain stem
Introduction
The nail gun has useful industrial applications. Increasing use of the nail gun has led to higher injury rates from the use of tools with sequential actuation.
6) Nail gun injury can occur to various parts of the body.
1,
2,
5,
8) Often the injuries from the nail gun are not fully penetrating because of the bone.
4,
7,
9,
10) However, if penetration is very deep in the brain, the results may be fatal. We described a patient who fired shots from a nail gun deep into his brain, in a suicide attempt.
Go to :

Case Report
A 46-year-old male presented to our hospital with a Glasgow coma scale score of 3 and an open head injury. His son found him at home in possession of a nail gun. The patient was in a drunken state. Neurological examination revealed grade 0 motor reflexes; light pupillary reflex: 3 mm fix/5 mm fix and a comatose mental state. The scalp was ripped by the nail and the brain was exposed.
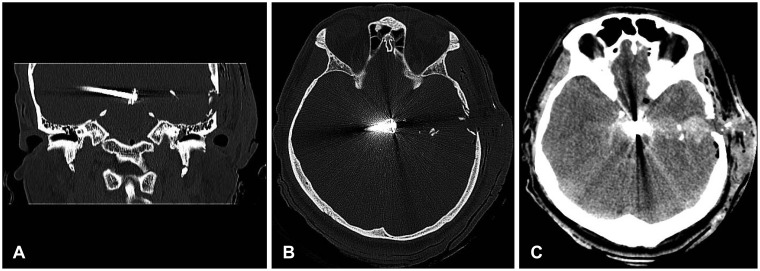
Brain computed tomography (CT) revealed comminuted fracture of the left temporal bone with inward displacement of bony fragments and foreign body in the suprasellar cistern to the right medial temporal lobe, with intracranial hemorrhage in the left temporal lobe along the moving pathway of the foreign body (
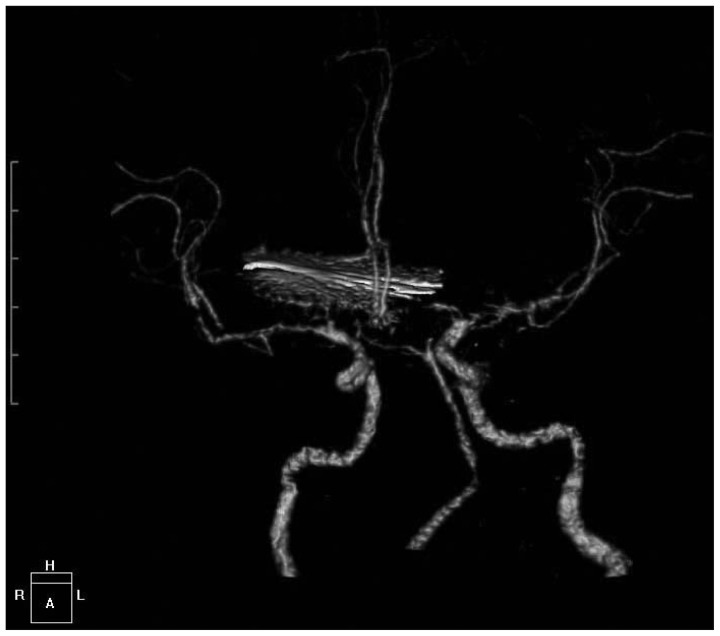
Figure 1). His vital signs were very unstable, and required orotracheal intubation with mechanical ventilator application. The patient was transferred to the intensive care unit, after initiation of antibiotic therapy. Surgery was planned for the removal of the penetrated nail, after the vital signs were stabilized. Preoperative CT angiography revealed no gross evidence of vascular injury (
Figure 2).
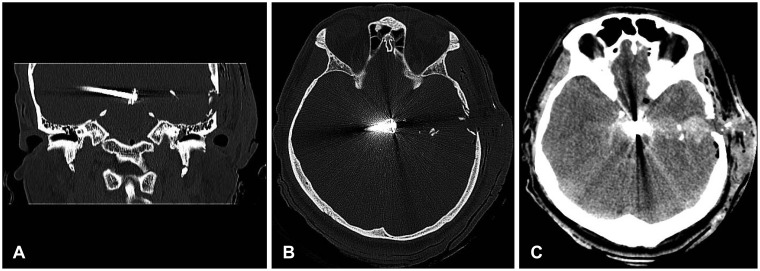 | FIGURE 1A: Initial brain computed tomography (CT) scan revealed comminuted fractures at the left temporal bone with inward displacement of bony fragments. B: Initial brain CT scan revealed foreign body at the suprasellar cistern to right medial temporal lobe. C: Initial brain CT scan revealed intraventricular hemorrhage at lateral and 3rd ventricle and subarachnoid hemorrhage at the basal cistern. Small amount of subcutaneous emphysema and diffuse scalp swelling were shown in the left temporal area. 
|
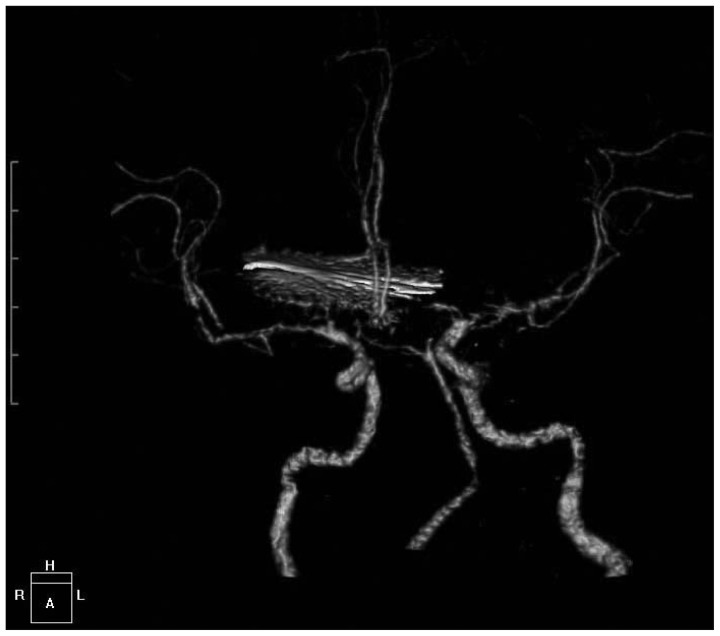 | FIGURE 2The preoperative brain computed tomography angiography revealed no gross evidence of vascular injury. 
|
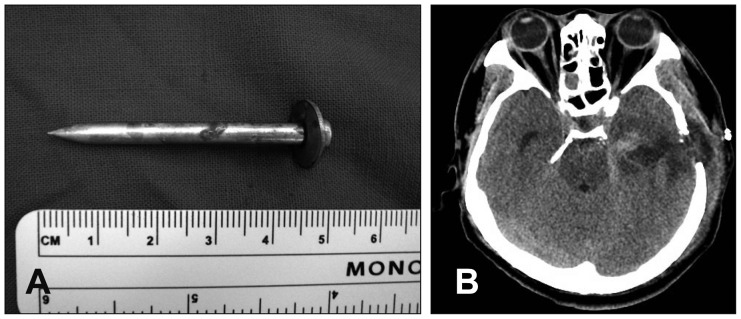
General anesthesia was employed. The patient was positioned supine with the head turned to the right on a horseshoe-shaped head holder. Intra-operatively, we found burned scalp (1st degree) and torn dura. We removed multiple fractured temporal bony fragments. We attempted cerebral endoscopy for removal of the nail, after bleeding control. However, continuous minimal bleeding blocked the operative sight. The nail was found by stylet with assisted neuronavigation (Medtronic StealthStation® S7™, Louisville, CO, USA) and removed with forceps (
Figure 3). A drainage catheter of intracerebral hematoma was placed and dural closure was accomplished with Durafoam™ (Codman, Wokingham, UK). Greenplast™ (Greencross, Seoul, Korea) were applied to prevent cerebrospinal fluid leakage.
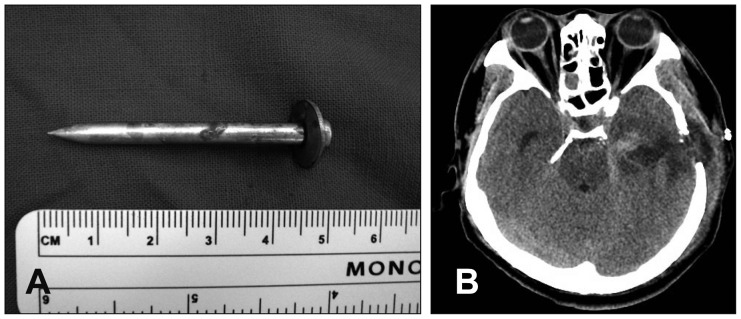 | FIGURE 3A: Photograph of a 5.0 cm long nail. B: Perihematoma edema seen in postoperative brain computed tomography. 
|
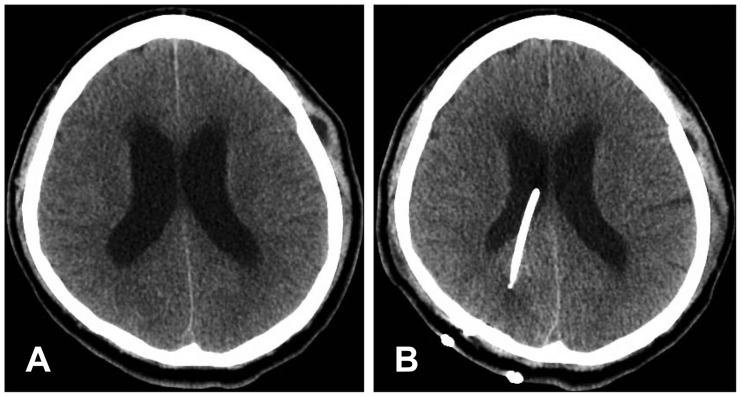
The patient's vital signs stabilized after removal of the nail. Neurological examination revealed Grade 3 motor reflexes; light pupillary reflex: 6 mm fix/6 mm fix; and a semicomatose mental state. Hydrocephalus had developed a month later. After ventriculoperitoneal shunt operation (
Figure 4), neurological examination revealed Grade 3 motor reflexes; light pupillary reflex: 5 mm fix/5 mm fix; and stuporous mental state with a Glasgow coma scale score of 6.
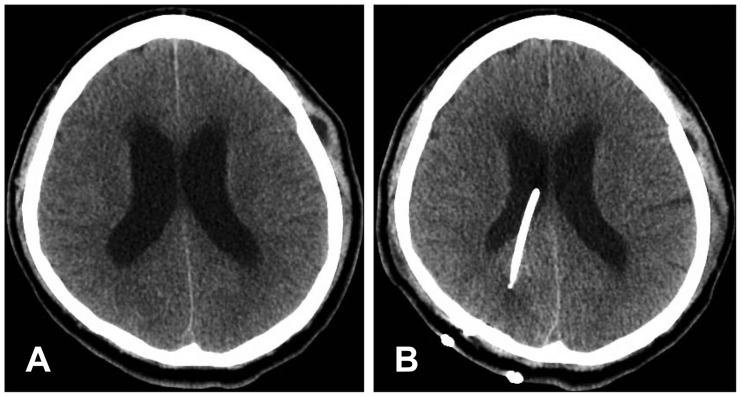 | FIGURE 4A: Preoperative brain computed tomography (CT) revealed Evan's ratio 0.32 with subcutaneous cerebrospinal fluid collection. B: Postoperative brain CT revealed Evan's ratio 0.30 with reduced subcutaneous cerebrospinal fluid collection. 
|
Go to :

Discussion
Injury rates have increased with the wide use of the nail-gun. The most common cause of nail-gun injury is work-related accidents,
6) although there are some instances of suicide. The efforts to reduce accidents is successful, however it is difficult to reduce nail gun use for suicidal purposes. Additionally, resultant brain injury can be fatal, and treatment is aimed at survival. We have three things considered for the treatment of patient. First, as in an emergency situation, airway, respiration and circulation are required to be evaluated. Our patient had acidosis and hypotension due to respiratory failure. Our patient's vital sign was stable after orotracheal intubation and mechanical ventilation. Second, the most commonly reported complications are the development of meningitis and cerebral abscesses.
10) So third generation cephalosporins (Triaxone, 2 gm/day) used immediately in this case. Third, the nail is required to be removed safely. So our patient's nail was found by stylet with assisted neuronavigation (Medtronic StealthStation® S7™) and removed with forceps. But if we can use electromagnetic tools, we enable more safe and easy removal.
Many patients with intracranial nail injuries survive with a relatively good neurological outcome, as long as the great cerebral vessels are intact and the brainstem is spared.
10) But prognosis was poor when primary traumatic brain stem damaged.
3) In this case, major blood vessels were intact, but due to early brain stem damage clinical outcome was poor.
Go to :

Conclusion
The nail gun is a powerful industrial tool used to drive nails into various hard surfaces with ease. However, there is an increased risk of injury to humans. If penetration is very deep in the brain, the results may be fatal. This case demonstrated successful surgical management of open head injury resulting from a nail gun. Brain stem injury in the subject led to a poor prognosis.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download