This article has been
cited by other articles in ScienceCentral.
Abstract
Acute subdural hematoma (ASDH) constitutes one of the most critical emergencies in neurosurgery and rapid spontaneous resolution of ASDH is an infrequent phenomenon. Several mechanisms have been attributed to explain this phenomenon including redistribution of subdural blood, dilution by cerebral spinal fluid and brain atrophy. Rapid resolution of ASDH related to coagulopathy is a rare phenomenon; to our knowledge, only one case has been reported. We report on a patient who showed rapid resolution of ASDH with coagulopathy and also discuss such a rare case with speculation of the coagulopathy as a factor to promote this phenomenon.
Go to :

Keywords: Hematoma subdural acute, Remission spontaneous, Blood coagulation disorder
Introduction
Acute subdural hemorrhage (ASDH) needs emergent neurosurgery or close observation because it associated with a 60-80% mortality rate. Sometimes, it is treated with emergent surgical decompression, patients may be managed conservatively when they are neurologically intact or the hematoma is small. Rapid spontaneous resolution of ASDH has rarely been reported because it takes several weeks or months for spontaneous resolution without neurosurgical interventions.
1,
3,
5) Moreover, the true incidence of rapid spontaneous resolution of ASDH is underestimated due to the routine use of emergency decompression. The underlying pathophysiology is not well understood, but probably more than one mechanism is responsible for this phenomenon. Two possible mechanisms for spontaneous resolution of ASDH have been put forward to explain this phenomenon including redistribution of subdural blood and dilution by cerebral spinal fluid (CSF).
10)
Herein, we present a patient with liver cirrhosis who show-ed an unexpected rapid resolution of ASDH spontaneously within 1 day after mild head injury and discuss the mechanism related to the coagulopathy contributed to the spontaneous resolution of the hematoma.
Go to :

Case Report
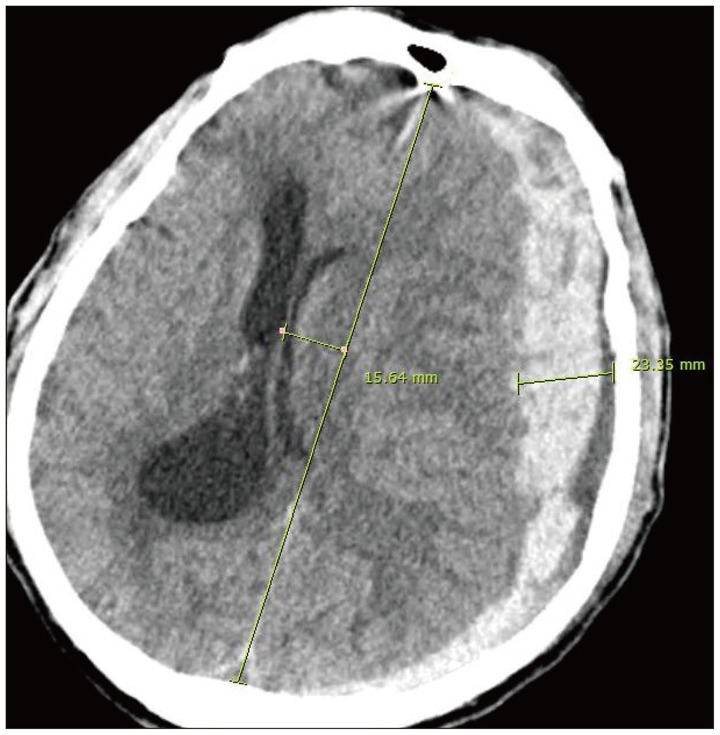
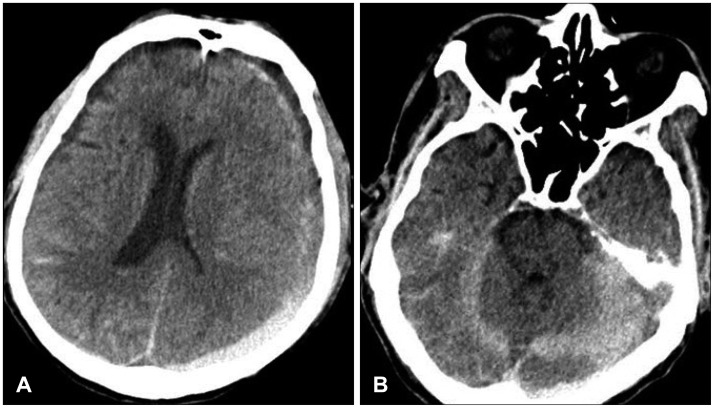
A 67-year-old male patient presented with deterioration of mental status following fall down less than 1 meter. He has the underlying disease, such as alcoholic liver cirrhosis, diabetes mellitus and hypertension. Initially, the patient was comatose with a score of five on the Glasgow coma scale and had a right hemiparesis with a dilated left pupil. Brain computed tomography (CT) revealed an ASDH with a thickness of 25 mm in the left frontotemporoparietal region. Midline shift caused by mass effects was 15 mm. A hypodense band was also observed between the inner table of the skull and the hyperdense collection (
Figure 1). We decided to perform craniotomy for hematoma removal but significant findings on blood work were revealed platelet count of 51000 and an international normalized ratio (INR) of 2.17. Under the consideration of post-operation complication and familial opinion, we decided to perform conservative care in intensive unit care. He received vitamin K and platelet transfusion. A repeated brain CT scan was performed 24 after the initial scan, and showed redistribution of hematoma to the tentorium and posterior inter hemispheric fissure (
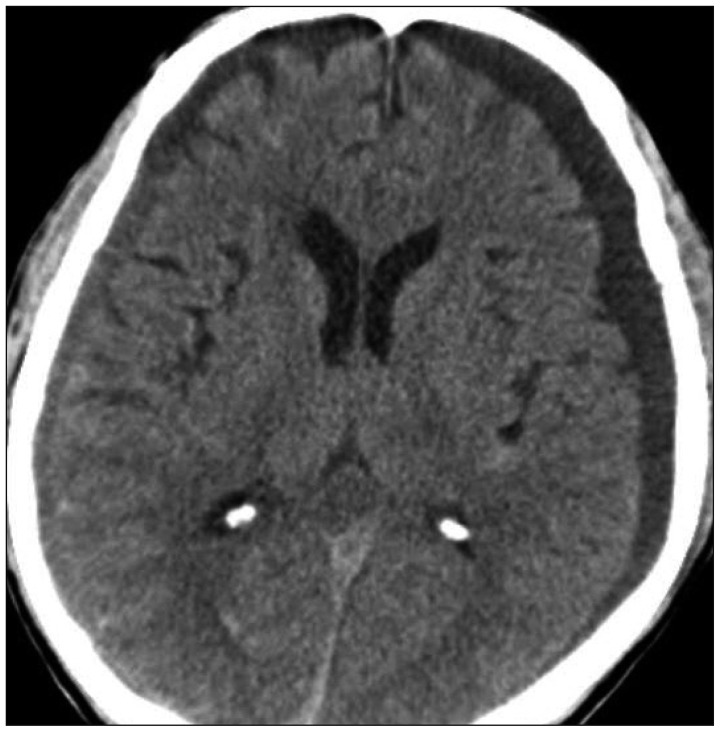
Figure 2). The ASDH over the left cerebral hemisphere had almost resolved. The mass effect to the ipsilateral lateral ventricle had resolved and the adjacent sulci reappeared. Another brain CT scan was performed on the next 3 days, CT scan showed complete resolution of the subdural hematoma (SDH) over the left cerebral hemisphere (
Figure 3). His clinical condition improved gradually after the CT scan. Within several days, he was obeying simple commands and verbalizing. He continued to improve radiologically and clinically from the neurological standpoint. He was subsequently referred to gastrointestinal doctor for the management of liver cirrhosis. After one month, he was discharged with alert mental status.
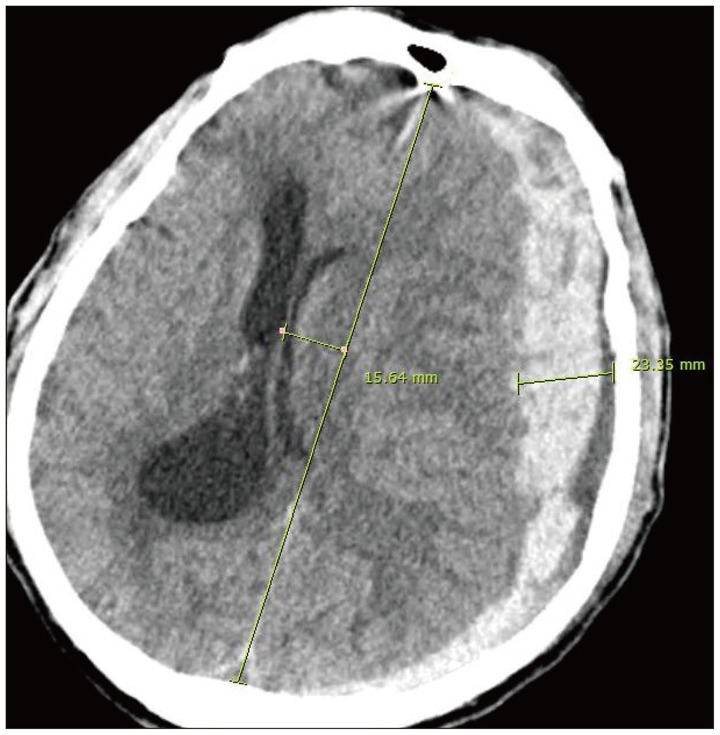 | FIGURE 1Initial computed tomography scan demonstrating a 23 mm thickness of acute subdural hematoma with midline shift of 15 mm in the left frontotemporoparietal region with herniation sign, compression of the brain stem. A band of low density between the subdural hematoma and inner table of the skull is seen. 
|
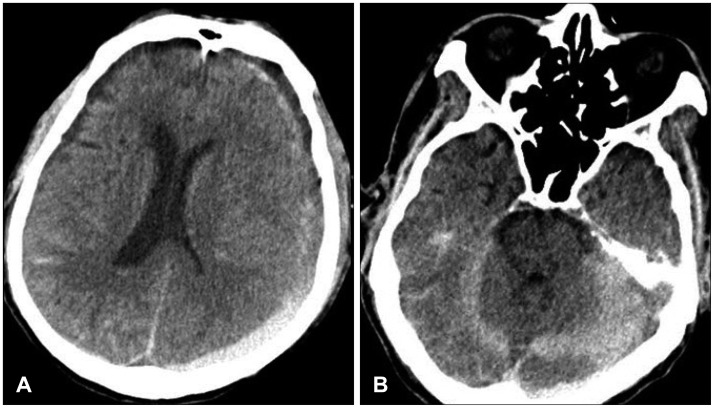 | FIGURE 2A: Computed tomo-graphy (CT) scans 1 day after the 1st brain CT scan shows a decrea-se of acute subdural hematoma and improvement of midline shift. B: The other image showing pro-minent redistribution of the hematoma into the tentorial spaces. 
|
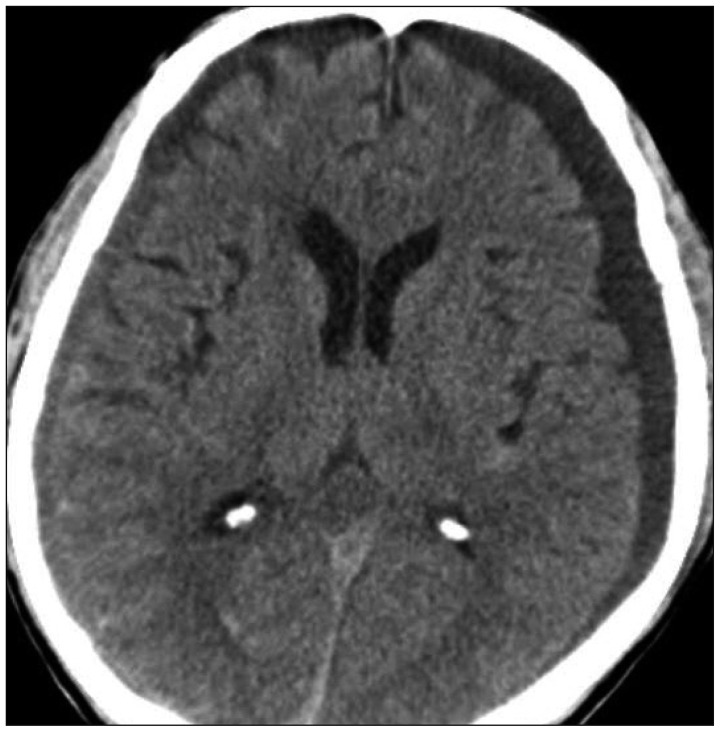 | FIGURE 3Computed tomography scan 3 day after accident shows resolution of acute subdural hematoma and a minimal amount of chronic subdural hematoma in both sided. 
|
Go to :

Discussion
ASDH is a frequent brain insult resulting from head injury and ASDH is a neurosurgical emergency requiring immediate therapeutic intervention. Most of these patients undergo urgent hematoma evacuation via a craniotomy except for those with poor general condition or with irreversible brain damage. Interestingly, there are a number of case reports in the literature describing the event of spontaneous ASDH resolution.
6,
10) The mechanism of the spontaneous resolution of ASDH has been attributed to intracranial redistribution of the hematoma rather than disappearance in the subdural space.
8) Two possible mechanisms have been proposed for this infrequent phenomenon. First, the hematoma may be diluted by flow of cerebrospinal fluid through the arachnoid tear, followed by retrograde flow into the subarachnoid space. This process is explained by the presence of a low density band between the SDH and inner table of the skull and it may be a useful sign for cases with good prognosis.
8) Second, brain swelling, caused by cerebral contusion, compresses the hematoma and may contribute the redistribution of hematomas resulting in rapid resolution of SDHs.
8) Some authors have demonstrated the finding of redistribution and dispersal of blood in the cerebellar tentorium or inter hemispheric subdural space with follow-up magnetic resonance imaging.
7,
9) In addition, the accompanying fracture might have facilitated the redistribution of the ASDH and improvement of the brain shift. This process may be explained by the prolapse of dura mater into the fracture sites by the force of the SDH.
2)
In this case, two mechanisms have been put forward to explain the rapid resolution of ASDH. First, this patient had a brain atrophy and the presence of a low density band between the SDH and inner table of the skull. The specificity of our case was the presentation of low density component and cerebral atrophy with widening of subarachnoid space. The combination effect of cerebral atrophy and CSF leakage may favor both redistribution and dilution of ASDH. Second, in follow-up imaging, there is an increasing of layer of a hyperintense component consistent with acute blood along the tentorium (
Figure 2) suggesting blood redistribution.
Additionally, the unique aspect of the case presented above is that the patient had a coagulopathy. In the present case, we were concerned as to why spontaneous resolution of ASDH happened to this patient with liver cirrhosis. To date, only one case of similar phenomenon has been reported. Chaudhary et al.
4) described a similar case of resolution of large SDH in a 73-year-old male with myelodysplastic syndrome. Healthy individuals possess adequate amounts of clotting factors, regulatory proteins, and platelets to achieve optimal clot formation, clot limitation, and dissolution. Patients with liver disease, on the other hand, have a disturbed balance of pro-coagulant and anti-coagulant factors deviating from the normal coagulation cascade. In this case, our patient had a known chronic liver disease, liver cirrhosis. There are two important factors to achieve hemostasis. One is a formation of a "platelet plug" which requires sufficient quantity of functional platelets working in an intact blood vessel. The other is a production of a "fibrin clot" which needs adequate and functional clotting factors. In this patient, as noted above, multiple factors can result in a hypocoagulable state because of liver cirrhosis. Decreased levels of all liver synthesized pro-coagulant factors, including the vitamin K dependent clotting factors (II, VII, IX, and X), indicated by the prolonged INR. Additionally, platelet dysfunction is also a contributing aspect of decreased clot formation, including thrombocytopenia. These conditions acts like the face and back of a coin for causing an ASDH with minor trauma in this patient, they may have also concerned to redistribution of hematoma by the preventing the well-organized hematoma formation. Summing up, this coagulopathic status is more susceptible for hematoma to wash out or redistribute via the CSF dilution route.
Go to :

Conclusion
Spontaneous resolution of ASDH is a rare phenomenon with only a few reported cases. The pathophysiologic mechanisms that are responsible for this phenomenon are dilution by CSF and redistribution of the ASDH in patients with cerebral atrophy. In this case, coagulopathy, as a new factor, may contribute to the spontaneous resolution of the hematoma.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download