Abstract
Objectives
We analyzed retrospectively incidence, management, and predictors of difficult intubation, which have been known through practical cases.
Methods
A total of 217 cases of difficult intubation (DI) between 2010 and 2014 were investigated. Risk factors such as age, body mass index, Mallampati score, thyromental distance, degree of mouth opening and range of neck motion, Cormack-Lehane grade, intubation and airway management techniques were investigated. The cases of each department were analyzed and the airway management techniques according to simplified risk scores (SRS) were also investigated.
Results
The average incidence of DI was 0.49%. Patients undergoing surgery in the departments of oro-maxillo-facial surgery (1.35%), ophthalmologic surgery (0.96%), urologic surgery (0.80%), and head and neck surgery of ear-nose-throat (0.62%) showed the higher incidence of DI. Difficult mask ventilation (10 of 217, 4.6%) was occurred with DI. Higher SRS were related to high rates of video laryngoscope use and fiberoptic guided intubation. There was a decrease in the use of McCoy blades after 2013, an increase in the use of video laryngoscope, and a consistent rate of fiberoptic intubation.
Conclusion
It is not easy to check all the predictors of DI in a preanesthetic evaluation and the predictors are not accurate. The role of clinical preparation and practical management is important, and the most important thing is to establish a planned induction strategy. Multiple factors system, such as simplified risk factors should be used to evaluate patients to prepare for appropriate airway management techniques in case of DI.
Airway management is fundamental technique and require the major responsibility for anesthesiologists. Failure to be prepared for difficult airway management is the major cause of severe morbidity and mortality related to anesthesia [1]. Following the appropriate airway management technique for individualized patient is crucial for a safe anesthesia care. Standard definition of the difficult intubation (DI) cannot be identified in the available literature. For previous practice guidelines, a difficult airway is defined as the clinical situation in which a conventionally trained anesthesiologist experience difficulty with facemask ventilation, endotracheal intubation, or both [2]. And a difficult endotracheal intubation is defined as the clinical situation in which cases of patients who are hard to intubate and require multiple intubation attempts, regardless of the tracheal pathology [2]. Alternatively, DI cases may be defined as those with Cormack-Lehane grade (C-L grade) III or IV on direct laryngoscopic view [3]. The DI represents a complex interaction between patients-related factors, the clinical setting, and the skills of the practitioner. Analysis of this interaction requires precise collection and communication of data. A previous meta-analysis has reported the incidence of DI to be 4.5%–7.5% [4]. Unpredictable DI brings numerous concerns regarding anesthesia. Many researchers have attempted to predict DI through simple airway physical examinations that can be conducted on bed-side [4]. But Wilson [5] advanced an opinion “test is not likely to be perfect, therefore, it remains essential that every anesthesiologist must be trained and equipped to deal with the now much less common, unexpected encountered difficult intubation.” Yentis [6] stated it is not easy to predict DI because of its low occurrence rate and questioned whether attempts are likely to be useful.
The aim of this study was retrospectively to analyze the incidence, predictors, management of encountered DI, and to review the preparation, strategy, follow-up care.
Retrospectively, 217 DI cases depending on the decision of the responsible anesthesiologists of anesthesia medical records from patients aged more than 18 years undergoing general anesthesia were included in a 5-year period of time (January 2010 to December 2014). This DI cases were diagnosed by anesthesiologists that performed tracheal intubation in each case. This study was conducted after obtaining the Institutional Review Board approval (No. 2016-06-035).
General anesthesia is provided by anesthesiologists of varied levels of training under at least one supervisor of our institutional anesthesia faculties or senior physicians. Preoperative evaluation for scheduled operation was performed and documented at least one day before operation in preanesthetic visiting clinic using standard screening tool including airway examination such as Mallampati score, dentition, range of neck motion, maximal mouth opening, and thyromental distance. If the abnormal results were observed, specialist consultation was performed.
Direct laryngoscopy was with a standard Macintosh blade sized appropriately. The direct laryngeal view was graded according to the C-L grade [7]. Grade III and IV were assumed to be DI and recorded as “difficult intubation” on anesthesia record.
Based on labeled DI anesthetic records, the patients' age, gender, height, weight, and body mass index (BMI, kg/m2), underlying disease such as rheumatoid arthritis and ankylosing spondylitis with abnormal neck motion, Classification of American Society of Anesthesiologist physical status (ASA class), previous history of DI, previous history of airway or neck surgery, analysis of each department, and whether the procedure was elective or emergency from the preanesthetic evaluation sheets were investigated. The nature of the airway difficulty including difficulty with face mask ventilation, and intubation technique, description of encountering airway difficulty and the used various airway management techniques were also collected.
The “complete documentation for DI” was considered as description of nature of DI and various airway management techniques served a beneficial or not as well as airway evaluation including history and standard physical examination. Age and BMI were divided into groups known as risk factors [8] for analysis of difficult mask ventilation cases. The risk factors for difficult mask ventilation reported by Kheterpal et al. [9] were analyzed.
The simplified risk score (SRS), which is a predictive factor for DI suggested by Eberhart et al. [10], was investigated for each patient. The evaluated risk factors included presence of front teeth, previous history of DI, Mallampati score>1, Mallampati score=4, and mouth opening<4 cm. The cases were given 1 point for each risk factor and the points were added up to determine the total score.
Data management and all statistical analyses were done using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Nominal variables such as Mallampati score, C-L grade, dentition, and mouth opening were analyzed using the chi-square test. Continuous variables such as BMI and age were assessed using the independent-sample t-test. Evaluation of the risk factors was done using logistic regression analysis.
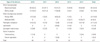
From 2010 to 2014, the total number of general anesthesia for patients over 18 years was 44,496 cases. The number of DI cases was 217, which translated to an incidence of 0.49%. The proportion of male to female patients was 59.9% to 40.1%. The average age and BMI were 55.3±14.2 years and 23.9±3.6 kg/m2, respectively (Table 1).
Twenty-three cases had a previous anesthesia history of DI. Among them, two cases belonged to department of general surgery (GS, 8.7%), 8 to department of orthopedic surgery (OS, 34.8%), 7 to department of urologic surgery (URO, 30.4%), 1 to department of head and neck surgery of ear-nose-throat (ENT, 4.3%), and 5 to department of oro-maxillo-facial surgery (OMS, 21.7%). There was two emergency surgery case. In 10 cases, intubation with direct laryngoscope was successfully performed even though previous of DI history, 1 case with video laryngoscope, and 12 cases with fiberoptic guidance. One case failed to endotracheal intubation and surgery was canceled. Twenty cases had a history of airway or neck surgery. Among them, 3 had a history of DI. Two cases had a history of gingival cancer surgery with abnormal distortion in the structural and function of the mandible due to mandible reconstruction and flap. Other case had a history of mandible fracture surgery, and showed restricted mouth opening <2 fingerbreadths (FB). The other 17 cases had no history of DI and were newly recorded as DI after the surgery.
One hundred and eighty-seven cases (86.2%) had documentations of their Mallampati scores. Mallampati score≥III accounted for 13 cases (7%). The number of cases that had documentation of dentition status was 156, and the anesthetic records showed that 22 cases had C-L grade IV. Only 111 cases (51.2%) had records of standard screening tool including airway examination such as Mallampati score, dentition, range of neck motion, maximal mouth opening, and thyromental distance, and C-L grade, intubation technique (Table 2).
Difficult mask ventilation (4.6%) was identified. A thyromental distance of less than 3 FB, which was significant with a P-value of 0.046 and the odds ratio of 5.12. Other known risk factors for difficult mask ventilation showed no discrepancies.
Patients undergoing surgery in the department of OMS (1.35%), ophthalmologic surgery (OPH, 0.96%), URO (0.80%), ENT (0.62%) showed the higher incidence of DI. The cases of OMS showed significant differences in terms of restricted mouth opening (P<0.001), history of DI (P=0.005), and history of airway or neck surgery (P=0.001). The cases of OPH was higher in incidence, but the number of cases was only four. The cases of URO showed significant differences from other departments in terms of age (P=0.006), BMI (P<0.001), gender (P<0.001), and history of DI (P=0.020). The cases of ENT had no difference from other departments.
Alternative approaches to manage encountered DI were identified cases that used McCoy blade (Penlon Ltd, Abingdon, UK) as well direct laryngoscopic blade of alternative design and size, lightwand, video laryngoscope-assisted techniques such as Pentax AWS (Pentax, Tokyo, Japan) and McGrath MAC (Aircraft Medical Ltd, Edinburgh, UK), awake fiberoptic intubation, and surgical airway (tracheostomy). Endotracheal intubation failed in a total of 3 cases; tracheostomy was performed in 2 of these cases and the surgery itself was canceled due to failed endotracheal intubation in 1 case.
Table 3 showed the frequency of airway management techniques in DI cases by year. Among the 27 cases that used fiberoptic intubation, 12 cases which had a history of previous fiberoptic intubation used fiberoptic guided technique from the beginning. Among the cases that used fiberoptic intubation from the beginning, 7 cases were recorded as DI. Five cases were expected to be DI, and fiberoptic intubation was used from the beginning. A total of 3 cases used lightwand, where 1 case was due to restricted mouth opening, 1 case was due to unsuccessful attempt of McGrath MAC and Pentax AWS, and 1 case was due to restricted neck extension.
Table 4 shows the frequency of the airway management techniques used in the C-L grade IV. The number of cases that had possible description of all the SRS-related specifications was 187. No case had an SRS of 0, 27 cases had an SRS of 1, 128 cases had an SRS of 2, 26 cases had an SRS of 3, and 6 cases had an SRS of either 4 or 5. Cases with an SRS of 1 and 2 had the largest number of direct laryngoscope use and the number of cases using direct laryngoscopes decreased with increasing SRS. Nine out of 26 cases with a score of 3 (34.6%) used video laryngoscope and 19 out of 128 cases with a score of 2 (14.8%) used video laryngoscope, which indicated that video laryngoscope was used in cases with scores ≥3. Fiberoptic intubation was predominantly used in cases with a score of ≥4 (Table 5).
Between 2010 and 2014, there were 0.49% incidence of DI. Male accounted for the larger proportion at 59.9%. Heinrich et al. [11] reported that male gender as a risk factor for C-L grade III/IV findings. In this study, male gender was higher incidence.
The average BMI was 23.9±3.6 kg/m2 and the average age was 55.3±14.2 years. Heinrich et al. [11] reported that 6.1% of the cases involved obese patients with a BMI over 35 kg/m2. In our study, only 2 cases had patients with a BMI of over 35 kg/m2 (0.9%). Ezri et al. [12] reported that BMI had not positive correlation to predict the increase in C-L grade. A large-scale cohort study by Lundstrom et al. [13] reported that the average BMI of patients with DI was 26.3 kg/m2 and that BMI was a weak predictor of DI. The average BMI in our study was low as value of 23.9 kg/m2.
Although Samsoon and Young [14] modified the Mallampati from 3-scale test to a 4-scale test. It is currently used as a screening tool to evaluate potential DI. In this study, 187 cases had documented Mallampati scores, and Mallampati ≥ III accounted for 13 cases (7%). Heinrich et al. [11] reported that 17.3% of DI cases had Mallampati scores of III or IV and that the Mallampati score was a factor that increased the predict rate for DI. But a meta-analysis by Lundstrom et al. [3] reported that the prognostic value decreased when only Mallampati scores were used for predictability of DI. The low proportion of cases with Mallampati scores III/IV in this study prove that solely using the Mallampati scores may not be reliable in predicting DI. In this study, difficult mask ventilation cases showed a significant difference in the short thyromental distance (<3 FB). However, Mallampati score, age, and BMI, the other predictors suggested by Kheterpal et al. [9] was not significant differences in this study.
Shiga et al. [4] conducted a meta-analysis on DI screening tests that could be performed at the bed-side. The results indicated that when only one of the predictors of DI, such as the Mallampati score, thyromental distance, or mouth opening was used for screening, the predictive value decreased. On the contrary, a combination of Mallampati score and thyromental distance was the most effective in predicting DI on the bedside. In this study, the previously mentioned risk factors did not show any significant differences. It is not easy to predict DI by relying on a single predictor; hence, multiple factors have to be considered. The results and values could differ based on the person conducting the tests. Predicting DI based on these factors could be difficult. Education on accurate screening test methods and documentation should be administered exactingly by high systemic standards. Besides preanesthetic evaluation, the factors should be double-checked at the operating room, and a secondary documentation should be performed. These procedures would allow for the preparation of an appropriate airway management technique by predicting the risk of DI.
Among the 217 cases of DI, only 111 cases had complete documentation comprising with screening test as well as the Mallampati score, C-L grade, intubation technique (51.2%). Although last successful airway management techniques were documented in all cases, we could not find the documented descriptions of the actual intubation as attempted and failed process for DI in 39 cases. Since the probability of DI is about 24% in patients with a previous history of DI [1], previous anesthesia records should be taken into account to decide on the appropriate airway management technique to be used. Since the anesthesia records help in deciding an appropriate technique, a more detailed documentation would be necessary.
Twenty-two cases had C-L grade IV; of these, 8 cases were intubated using direct laryngoscope. Of the 8 cases that used direct laryngoscopes, Macintosh blades were used in 3 cases. In cases with C-L grade IV, the epiglottis was not observable, and intubation using direct laryngoscope must have been difficult. There is a possibility that C-L grade III might have been incorrectly documented as grade IV. Neck manipulation or bougie introducer could have been used. However, these procedures were not documented and could not be confirmed. A study by Krage et al. [15], which evaluated 120 anesthesiologists regarding the definition of C-L grade using surveys, reported that only 25% of the participants could accurately define the criteria for each grade. In the simulator-based study, inter-observer reliability was fair with a kappa coefficient of 0.35 and intraobserver reliability was poor with a kappa of 0.15 [15]. That cases could have been inappropriately classified. It is important to train the anesthesiologist adequately to correctly classify each case. When a DI case is recorded, the patient's risk factors, such as Mallampati score, dentition, thyromental distance, degree of mouth opening, range of neck motion, surgical history, actual intubation process, C-L grade, and intubation technique should be accurately documented to be prepared for next anesthesia in the future. The patients should be allocated an environment that allows systematic documentation of airway management techniques.
During a period of 5 years, the incidence of DI was 0.49%, which is different from the 5.1% [1] reported by a previous study. This difference is inferred to be due to the racial differences between Asians and the Western population in terms of BMI [16], which may affect the risk factors. In our hospital, video laryngoscope was routinely used from the beginning for intubation when DI was suspected in case of BMI>30 kg/m2, poor dentition, and limited range of neck motion, and pathology of musculoskeletal system of neck. In such cases, the laryngeal view is improved, C-L grading is not possible due to direct laryngoscope is not used.
Although GS had the largest number of cases at 54, the incidence was 0.41%. Out of the 52 cases of OS, the incidence was 0.56%. OMS department had 16 cases, the incidence was 1.35%. It seems to be related to structural abnormalities around the airway or limitation of mouth opening. OPH cases was only 4. It was too small number. And patients of OPH cases had no specific risk factors. Of the 28 cases of URO, the incidence was 0.80%. The proportion of male patients was large and the average age was higher. The BMI in URO was relatively higher than others, and the number of patients with previous history of DI was also higher. These patient characteristics could have contributed to a higher incidence compared to other departments. A study by Moon et al. [17] reported that the incidence of DI increased with increasing age.
The airway management techniques currently used in our hospital are direct laryngoscope, McCoy blade, lightwand, Pentax AWS, McGrath MAC, and fiberoptic intubation. In 2013, McGrath MAC was introduced at our hospital and the use of McGrath MAC in DI gradually increased from 2013 to 2014. On the contrary, the use of Pentax AWS and McCoy blades gradually decreased. In cases where the distance from the mouth to the larynx was long or the mouth opening was restricted, Pentax AWS had an increased intubation failure rate [18]. As McGrath MAC blades have a curvature, they easily expose the vocal cord. The ease of use might have contributed to its increased use. The decrease in McCoy blade usage since 2014 was due to the increase in the video laryngoscope use. The use of fiberoptic intubation has been consistent throughout the years. It can be that the fiberoptic intubation was planned consistently in cases that had suspected DI, and that intubation often failed even with the use of a video laryngoscope.
The number of cases that had all the data necessary to calculate the SRS was 187. As cases with a score of 0, 1, or 2 had a high proportion of direct laryngoscope use, direct laryngoscope could be primarily used in cases with a score of 0, 1 or 2. Cases with a score of 3, 4 or 5 had a higher proportion of Mc-Grath MAC and fiberoptic intubation use. These devices should be prepared when SRS≥3.
As study was a retrospective study based on the medical records, this study has limitations. Thirty-nine cases did not have any documentation on the intubation process including C-L grade. It was not possible to determine the number of intubation attempts, external laryngeal manipulation, and use of bougie introducer. Since this study has only DI cases, the statistical results could underestimate factors previously known as predictors or risk factors of DI. And there was no documentation about complication related to intubation.
In conclusion, it is not easy to check all the predictors of DI in a preanesthetic evaluation and the predictors themselves may be not accurate. Therefore, the role of clinical preparation and practical management is important, and it is important to establish a planned induction strategy. Multivariate factor systems, such as simplified risk factors should be also used to evaluate patients to prepare for appropriate airway management techniques in case of DI.
Figures and Tables
References
1. Lundstrom LH, Moller AM, Rosenstock C, Astrup G, Gatke MR, Wetterslev J, et al. A documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia. 2009; 64:1081–1088.
2. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013; 118:251–270.
3. Lundstrom LH, Vester-Andersen M, Moller AM, Charuluxananan S, L'hermite J, Wetterslev J, et al. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177,088 patients. Br J Anaesth. 2011; 107:659–667.
4. Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005; 103:429–437.
6. Yentis SM. Predicting difficult intubation: worthwhile exercise or pointless ritual? Anaesthesia. 2002; 57:105–109.
7. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39:1105–1111.

8. Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R. Clinical anesthesia. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2013.
9. Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006; 105:885–891.

10. Eberhart LH, Arndt C, Aust HJ, Kranke P, Zoremba M, Morin A. A simplified risk score to predict difficult intubation: development and prospective evaluation in 3763 patients. Eur J Anaesthesiol. 2010; 27:935–940.

11. Heinrich S, Birkholz T, Irouschek A, Ackermann A, Schmidt J. Incidences and predictors of difficult laryngoscopy in adult patients undergoing general anesthesia: a single-center analysis of 102,305 cases. J Anesth. 2013; 27:815–821.
12. Ezri T, Warters RD, Szmuk P, Saad-Eddin H, Geva D, Katz J, et al. The incidence of class “zero” airway and the impact of Mallampati score, age, sex, and body mass index on prediction of laryngoscopy grade. Anesth Analg. 2001; 93:1073–1075.

13. Lundstrom LH, Moller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009; 110:266–274.
14. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987; 42:487–490.

15. Krage R, van Rijn C, van Groeningen D, Loer SA, Schwarte LA, Schober P. Cormack-Lehane classification revisited. Br J Anaesth. 2010; 105:220–227.

16. Saito T, Liu W, Chew ST, Ti LK. Incidence of and risk factors for difficult ventilation via a supraglottic airway device in a population of 14,480 patients from South-East Asia. Anaesthesia. 2015; 70:1079–1083.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download