Introduction
Uremic pleuritis is a fibrinous pleuritis of unknown cause in patients with chronic kidney disease (CKD). The term "uremic pleuritis" was first introduced 4 decades ago, however, there is still a lack of information regarding the pathogenesis, clinical course and optimal management. Although a previous study reported that the incidence of uremic pleuritis is 20%–57% in patients who died of uremia, due to the recent wide adaptation of regular dialysis in CKD patients, the incidence is decreasing [1]. The diagnosis of uremic pleuritis is challenging as there is no pathognomic diagnostic test. Exclusion of other causes of pleural effusion is necessary before the confirmative diagnosis.
Conventionally, uremic pleuritis has been treated with regular hemodialysis, repeated thoracentesis or chest tube drainage. In case of persistent disease, pleurodesis or surgical decortication can be an option [2]. However, cases unresponsive to those therapies have been reported [234]. Treatment of refractory uremic pleuritis has not been established. Here, we report a case of refractory uremic pleuritis which showed marked improvement following corticosteroid therapy.
Case
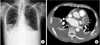
A 53-year-old male was admitted to our hospital because of increasing bilateral pleural effusion and dyspnea (modified Medical Research Council grade II) for 2 weeks. He had undergone hemodialysis for 4 hours 3 times a week for 5 years for CKD due to type I diabetes and hypertension. He never smoked and was a social drinker. His height and weight were 163.5 cm and 58.8 kg, respectively. His blood pressure was 130/88 mmHg, heart rate was 88 beats per minute, respiration rate was 20 breaths per minute, and body temperature was 36.7℃. Chest auscultation revealed decreased lung sound on both lung fields. His lower extremeties showed no pitting edema. Chest X-ray showed blunting of both costophrenic angles suggesting bilateral pleural effusion. Chest computed tomography (CT) scan showed a large amount of bilateral effusion (Fig. 1).
Laboratory findings showed anemia (hemoglobin, 10.4 g/dL), uremia (creatinine, 5.5 mg/dL), hypoalbuminemia (albumin, 2.9 g/dL), and elevation of C-reactive protein (CRP, 30 mg/L). The anti-nuclear and anti-neutrophilic antibodies were all negative. B-type natriuretic peptide level was normal. Multiplex reverse transcriptase real-time polymerase chain reaction (PCR) for respiratory virus was negative. In addition, test for human immunodeficiency virus and hepatitis virus were negative. Echocardiography revealed normal cardiac function without pulmonary hypertension. We performed thoracentesis and the pleural fluid was straw-colored and monocyte dominant exudate. Bacterial culture, acid-fast bacili smear/culture and tuberculosis PCR using pleural fluid revealed negative findings. Adenosine deaminase was within normal limit. Thus we performed thoracoscopic pleural biopsy for this exudative pleural effusion with unknown etiology. Biopsy sample revealed chronic inflammation with fibrosis without evidence of infectious disease or malignancy (Fig. 2). On the basis of these results, we could diagnose him as uremic pleuritis. As the Kt/V, a way of measuring hemodialysis adequacy, has been above 1.4, as recommended by current guideline, we continued hemodialysis and maintained the chest tube drainage. However, the amount of drainage was over 200 mL daily for 2 week. Even after the dialysis regimen was intensified from 4 hours to 5 hours per day weekly for several weeks, the draining amount was not decreased and the CRP level was elevated to 88 mg/L. To manage this refractory case that is not responsive to conventional treatment, we administered methylprednisolone at an initial dose of 40 mg/day, given the possibility of an ongoing inflammatory process in this pleuritis. The draining amount gradually decreased and the CRP level also dropped to normal after 2 weeks of administration. We removed the chest tube and tapered out the medication during 4 weeks (Fig. 3). Pleural effusion did not recur after suspension of the treatment and he has been followed up in our outpatient clinic for more than one year without complications.
Discussion
Even after dialysis became widely available, patients with CKD face a variety of complications including pleural effusion. Many etiologies including volume overload, heart failure, infection, malignancy and connective tissue diseases can cause pleural effusion in those patients [25]. Uremic pleuritis has become a clinicopathologic entity by Nidus et al. [4] in 1969 as fibrinous pleuritis of unknown cause in patients with CKD. Recent studies reported that it consists of 3.8%–23.7% of pleural effusions developed in hemodialysis patients [25].
Uremic pleuritis results from inflammation of the pleural membranes and its pathogenesis is poorly understood [6]. Although toxins like phosphates, uremic acid and retained immune complexes have been suggested as the etiology, there is no proven association between uremic toxins and the development of uremic pleuritis. The pleural fluid is typically serous or serosanguinous with a predominance of either lymphocytes or neutrophils. Of note, one must rule out other causes before concluding the pleural effusion as a uremic pleuritis. Pleural biopsy is critical for the diagnosis and shows nonspecific chronic fibrinous inflammation. In general, uremic pleuritis responds to treatment including regular hemodialysis or drainage of the pleural effusion. A previous study has reported that pleural effusion improved in 94% of patients with continuation of hemodialysis with or without chest tube drainage [2].
In the present case, even after chest tube drainage and intensification of hemodialysis, there was no improvement of pleural effusion. As the effusion was exudate and the CRP level was elevated during the clinical course, we assumed that an inflammatory process was involved. We started corticosteroid and the effusion was gradually cleared with reduction in the CRP level. To our knowledge, there are only three reported case of refractory uremic pleuritis which improved with corticosteroid treatment [278]. In the first case, they started 50mg of prednisolone and complete disappearance of effusion was observed 6 weeks after treatment [2]. In the other cases, they used the same regimen and the pleuritis or pleuropericarditis was resolved in a month [78]. Similarly, we used 40 mg of methylprednisolone initially and noted nearly complete response in 2 weeks of treatment.
In conclusion, the present case suggests that corticosteroids may have benefit and can be considered as a therapeutic option for uremic pleuritis which is resistant to conventional treatment. Further studies are necessary to determine the dosage, efficacy and safety of this potential treatment modality.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download