Abstract
Objectives
Metabolic acidosis frequently develops in patients after neobladder reconstruction. However, the incidence of metabolic acidosis in patients with neobladder and the factors associated with the development of metabolic acidosis have not been well elucidated. We aimed to investigate the incidence and the potential predictors for the development of metabolic acidosis after neobladder reconstruction with intestinal segment.
Methods
We included patients who underwent neobladder reconstruction using intestinal segment at Ewha Womans University Mokdong Hospital between January 1, 2005 and December 31, 2014. A subgroup of patients according to the time of metabolic acidosis occurrence was further analyzed in order to characterize predictors for metabolic acidosis.
Results
Metabolic acidosis was encountered in 79.4% of patients with neobladder during follow up period. When patients were divided into 2 groups according to anion gap (AG), total CO2 (18.9±2.1 mEq/L vs. 20.0±1.3 mEq/L, P=0.001) and chloride (106.6±4.9 mE/L vs. 109.4±3.6 mEq/L, P<0.001) were significant different between groups with AG>12 and AG≤12. Furthermore, when patients were divided into 3 groups; patients with metabolic acidosis at postoperative day (POD) 1; from POD 2 to 14 days; after 14 days, there was significant difference among those subgroups.
Conclusion
Our study showed the rate of metabolic acidosis in patients underwent neobladder reconstruction and the difference between patients with metabolic acidosis and those without metabolic acidosis for the first time in Korea. In the future, well designed prospective study will be needed to prevent metabolic acidosis after neobladder reconstruction.
Figures and Tables
Fig. 1
Changes of serum total CO2 (A) and chloride level (B) between preoperative and at the diagnosis of metabolic acidosis in patients who had metabolic acidosis after neobladder replacement operation. Cl, chloride; pre op., preoperative; post op., postoperative.

Table 3
Comparisons in patients developed metabolic acidosis after neobladder replacement between normal and increased anion gap

Table 4
Comparisons of laboratory findings at diagnosis with metabolic acidosis between normal and increased anion gap

Table 6
Comparisons of baseline variables and preoperative laboratory findings in the patients according to the time of diagnosis with metabolic acidosis

Table 7
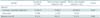
Comparison of laboratory findings in the patients according to the time of diagnosis with metabolic acidosis

Values are presented as mean±standard deviation or number (%). ANOVA and Bonferroni tests were applied for comparisons.
POD, post operative day.
*P=0.010 vs. POD>14. †P=0.046 vs. POD>14. ‡P=0.002 vs. POD>14. §P=0.008 vs. POD>14. ∥P=0.002 vs. POD≤14. ¶Number of included patients were 47, 20 and 12 in group with POD1, group of 1<POD≤14, and group of POD>14 respectively. **P<0.001 vs. POD>14. ††P=0.012 vs. POD>14.
References
1. Hautmann RE. Urinary diversion: ileal conduit to neobladder. J Urol. 2003; 169:834–842.
2. Mills RD, Studer UE. Metabolic consequences of continent urinary diversion. J Urol. 1999; 161:1057–1066.
3. Poulsen AL, Steven K. Acid-base metabolism after bladder substitution with the ileal urethral Kock reservoir. Br J Urol. 1996; 78:47–53.
4. Fujisawa M, Nakamura I, Yamanaka N, Gotoh A, Hara I, Okada H, et al. Changes in calcium metabolism and bone demineralization after orthotopic intestinal neobladder creation. J Urol. 2000; 163:1108–1111.
5. Kristjansson A, Davidsson T, Mansson W. Metabolic alterations at different levels of renal function following continent urinary diversion through colonic segments. J Urol. 1997; 157:2099–2103.
6. Lockhart JL, Davies R, Persky L, Figueroa TE, Ramirez G. Acid-base changes following urinary tract reconstruction for continent diversion and orthotopic bladder replacement. J Urol. 1994; 152(2 Pt 1):338–342.
7. Martinez-Cornelio A, Hernandez-Toriz N, Quintero-Becerra J, Flores-Lopez D, Moreno-Palacios J, Vazquez-Martinez E. Management of bladder cancer with Studer orthotopic neobladder: 13-year experience. Cir Cir. 2009; 77:411–417.
8. Goraya N, Simoni J, Jo CH, Wesson DE. Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Int. 2014; 86:1031–1038.
9. Studer UE, deKernion JB, Zimmern PE. A model for a bladder replacement plasty by an ileal reservoir: an experimental study in dogs. Urol Res. 1985; 13:243–247.
10. Davidsson T, Akerlund S, Forssell-Aronsson E, Kock NG, Mansson W. Absorption of sodium and chloride in continent reservoirs for urine: comparison of ileal and colonic reservoirs. J Urol. 1994; 151:335–337.
11. Austin JC. Long-term risks of bladder augmentation in pediatric patients. Curr Opin Urol. 2008; 18:408–412.
12. Hautmann RE, de Petriconi R, Gottfried HW, Kleinschmidt K, Mattes R, Paiss T. The ileal neobladder: complications and functional results in 363 patients after 11 years of followup. J Urol. 1999; 161:422–427.
13. Hautmann RE, de Petriconi RC, Volkmer BG. 25 years of experience with 1,000 neobladders: long-term complications. J Urol. 2011; 185:2207–2212.
14. Nieuwenhuijzen JA, de Vries RR, Bex A, van der Poel HG, Meinhardt W, Antonini N, et al. Urinary diversions after cystectomy: the association of clinical factors, complications and functional results of four different diversions. Eur Urol. 2008; 53:834–842.
15. Santucci RA, Park CH, Mayo ME, Lange PH. Continence and urodynamic parameters of continent urinary reservoirs: comparison of gastric, ileal, ileocolic, right colon, and sigmoid segments. Urology. 1999; 54:252–257.
16. Perez GO, Oster JR, Rogers A. Acid-base disturbances in gastrointestinal disease. Dig Dis Sci. 1987; 32:1033–1043.
17. Fichtner J. Follow-up after urinary diversion. Urol Int. 1999; 63:40–45.
18. Schmidt JD, Hawtrey CE, Flocks RH, Culp DA. Complications, results and problems of ileal conduit diversions. J Urol. 1973; 109:210–216.
19. Hautmann RE, Hautmann SH, Hautmann O. Complications associated with urinary diversion. Nat Rev Urol. 2011; 8:667–677.
20. McFarlane C, Lee A. A comparison of Plasmalyte 148 and 0.9% saline for intra-operative fluid replacement. Anaesthesia. 1994; 49:779–781.
21. Coran AG, Ballantine TV, Horwitz DL, Herman CM. The effect of crystalloid resuscitation in hemorrhagic shock on acid-base balance: a comparison between normal saline and Ringer's lactate solutions. Surgery. 1971; 69:874–880.
22. Moon PF, Kramer GC. Hypertonic saline-dextran resuscitation from hemorrhagic shock induces transient mixed acidosis. Crit Care Med. 1995; 23:323–331.
23. Vassar MJ, Perry CA, Holcroft JW. Analysis of potential risks associated with 7.5% sodium chloride resuscitation of traumatic shock. Arch Surg. 1990; 125:1309–1315.
24. Waters JH, Miller LR, Clack S, Kim JV. Cause of metabolic acidosis in prolonged surgery. Crit Care Med. 1999; 27:2142–2146.
25. Wang JS, Hong YP. Uretero-ileocystoplasty: a report of one case. Korean J Urol. 1960; 1:147–150.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download