Abstract
Objectives
The purpose of this study was to investigate the relationship of cord blood levels of soluble fms-like tyrosine kinase 1 (sFlt-1), placental growth factor (PlGF), and vascular endothelial growth factor (VEGF) in preterm infants with maternal preeclampsia.
Methods
Thirty six preterm infants born at Ewha Womans University Mokdong Hospital from January 2006 to August 2006 were studied after prior parental consent at mid-pregnancy. sFlt-1, PlGF, and VEGF levels in the cord blood of preterm neonate, with or without maternal preeclampsia, were measured using enzyme-linked immunosorbent assay.
Results
There was no difference in sFlt-1 between infants with and without maternal preeclampsia. Infants with maternal preeclampsia had significantly lower PlGF levels (P=0.035) and higher sFlt-1/PlGF ratio (P=0.080) with borderline significance. Cord blood VEGF levels were not related to maternal preeclampsia. Infants with maternal preeclampsia had lower birth weight (P=0.030), lower neonatal platelet count without statistical significance (P=0.064) and more likely to be small for gestational age (P=0.057). Neonatal platelet count was significantly correlated with cord blood PlGF levels (r=0.674, P=0.032).
Figures and Tables
 | Fig. 2Comparison of cord blood placental growth factor (PlGF) level in infants with maternal preeclampsia and controls. The thick line denotes median for each group. Analysis by Mann Whitney U test. |
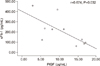 | Fig. 3Linear correlation between cord blood sFlt-1 and PlGF levels in infants with maternal preeclampsia. sFlt-1, soluble fms like tyrosine kinase 1; PlGF, placental growth factor. |
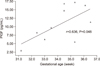 | Fig. 4Linear correlation between cord blood placental growth factor (PlGF) levels and gestational age in infants with maternal preeclampsia. |
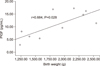 | Fig. 5Linear correlation between cord blood placental growth factor (PlGF) levels and birth weight in infants with maternal preeclampsia. |
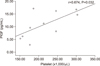 | Fig. 6Linear correlation between cord blood placental growth factor (PlGF) levels and platelet counts in infants with maternal preeclampsia. |
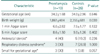
Table 2
Cord blood levels of sFlt-1, PlGF, and VEGF in infants with maternal preeclampsia and controls

Acknowledgments
This study was supported by Seoul Research & Business Development (2005-1547-1) Republic of Korea.
References
1. Fraser SH, Tudehope DI. Neonatal neutropenia and thrombocytopenia following maternal hypertension. J Paediatr Child Health. 1996; 32:31–34.
2. Burrows RF, Andrew M. Neonatal thrombocytopenia in the hypertensive disorders of pregnancy. Obstet Gynecol. 1990; 76:234–238.
3. Tsao PN, Teng RJ, Tang JR, Yau KI. Granulocyte colony-stimulating factor in the cord blood of premature neonates born to mothers with pregnancy-induced hypertension. J Pediatr. 1999; 135:56–59.
4. Tsao PN, Teng RJ, Chou HC, Tsou KI. The thrombopoietin level in the cord blood in premature infants born to mothers with pregnancy-induced hypertension. Biol Neonate. 2002; 82:217–221.
5. Chiswick ML. Prolonged rupture of membranes, pre-eclamptic toxaemia, and respiratory distress syndrome. Arch Dis Child. 1976; 51:674–679.
6. Skjaeraasen J. Amniotic fluid phospholipid concentrations in pregnancies with pre-eclampsia and/or intrauterine growth-retardation of the fetus. Acta Obstet Gynecol Scand. 1979; 58:191–195.
7. Zapata A, Hernandez-Garcia JM, Grande C, Martinez I, Perez J, de la Fuente P, et al. Pulmonary phospholipids in amniotic fluid of pathologic pregnancies: relationship with clinical status of the newborn. Scand J Clin Lab Invest. 1989; 49:351–357.
8. Baud O, Zupan V, Lacaze-Masmonteil T, AudibertF , Shojaei T, Thebaud B, et al. The relationships between antenatal management, the cause of delivery and neonatal outcome in a large cohort of very preterm singleton infants. BJOG. 2000; 107:877–884.
9. Lassus P, Ristimaki A, Ylikorkala O, Viinikka L, Andersson S. Vascular endothelial growth factor in human preterm lung. Am J Respir Crit Care Med. 1999; 159(5 Pt 1):1429–1433.
10. Tsao PN, Wei SC, Su YN, Lee CN, Chou HC, Hsieh WS, et al. Placenta growth factor elevation in the cord blood of premature neonates predicts poor pulmonary outcome. Pediatrics. 2004; 113:1348–1351.
11. Roberts JM, Pearson GD, Cutler JA, Lindheimer MD. National Heart Lung and Blood Institute. Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertens Pregnancy. 2003; 22:109–127.
12. Tsao PN, Wei SC, Su YN, Chou HC, Chen CY, Hsieh WS. Excess soluble fms-like tyrosine kinase 1 and low platelet counts in premature neonates of preeclamptic mothers. Pediatrics. 2005; 116:468–472.
13. Shibata E, Rajakumar A, Powers RW, Larkin RW, Gilmour C, Bodnar LM, et al. Soluble fms-like tyrosine kinase 1 is increased in preeclampsia but not in normotensive pregnancies with small-for-gestational-age neonates: relationship to circulating placental growth factor. J Clin Endocrinol Metab. 2005; 90:4895–4903.
14. Lee ES, Oh MJ, Jung JW, Lim JE, Seol HJ, Lee KJ, et al. The levels of circulating vascular endothelial growth factor and soluble Flt-1 in pregnancies complicated by preeclampsia. J Korean Med Sci. 2007; 22:94–98.
15. Lam C, Lim KH, Karumanchi SA. Circulating angiogenic factors in the pathogenesis and prediction of preeclampsia. Hypertension. 2005; 46:1077–1085.
16. Ahmad S, Ahmed A. Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res. 2004; 95:884–891.
17. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004; 350:672–683.
18. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003; 111:649–658.
19. Casella I, Feccia T, Chelucci C, Samoggia P, Castelli G, Guerriero R, et al. Autocrine-paracrine VEGF loops potentiate the maturation of megakaryocytic precursors through Flt1 receptor. Blood. 2003; 101:1316–1323.
20. Zhou Y, Damsky CH, Fisher SJ. Preeclampsia is associated with failure of human cytotrophoblasts to mimic a vascular adhesion phenotype. One cause of defective endovascular invasion in this syndrome? J Clin Invest. 1997; 99:2152–2164.
21. Shibuya M. Structure and function of VEGF/VEGF-receptor system involved in angiogenesis. Cell Struct Funct. 2001; 26:25–35.
22. Carmeliet P, Moons L, Luttun A, Vincenti V, Compernolle V, De Mol M, et al. Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat Med. 2001; 7:575–583.
23. Hattori K, Heissig B, Wu Y, Dias S, Tejada R, Ferris B, et al. Placental growth factor reconstitutes hematopoiesis by recruiting VEGFR1(+) stem cells from bone-marrow microenvironment. Nat Med. 2002; 8:841–849.
24. Livingston JC, Chin R, Haddad B, McKinney ET, Ahokas R, Sibai BM. Reductions of vascular endothelial growth factor and placental growth factor concentrations in severe preeclampsia. Am J Obstet Gynecol. 2000; 183:1554–1557.
25. Polliotti BM, Fry AG, Saller DN, Mooney RA, Cox C, Miller RK. Second-trimester maternal serum placental growth factor and vascular endothelial growth factor for predicting severe, early-onset preeclampsia. Obstet Gynecol. 2003; 101:1266–1274.
26. Nagamatsu T, Fujii T, Kusumi M, Zou L, Yamashita T, Osuga Y, et al. Cytotrophoblasts up-regulate soluble fms-like tyrosine kinase-1 expression under reduced oxygen: an implication for the placental vascular development and the pathophysiology of preeclampsia. Endocrinology. 2004; 145:4838–4845.
27. Ahmed A, Dunk C, Ahmad S, Khaliq A. Regulation of placental vascular endothelial growth factor (VEGF) and placenta growth factor (PIGF) and soluble Flt-1 by oxygen-a review. Placenta. 2000; 21:Suppl A. S16–S24.
28. Lash GE, Taylor CM, Trew AJ, Cooper S, Anthony FW, Wheeler T, et al. Vascular endothelial growth factor and placental growth factor release in cultured trophoblast cells under different oxygen tensions. Growth Factors. 2002; 20:189–196.
29. Speake PF, Glazier JD, Ayuk PT, Reade M, Sibley CP, D'Souza SW. L-Arginine transport across the basal plasma membrane of the syncytiotrophoblast of the human placenta from normal and preeclamptic pregnancies. J Clin Endocrinol Metab. 2003; 88:4287–4292.
30. Daayana S, Baker P, Crocker I. An image analysis technique for the investigation of variations in placental morphology in pregnancies complicated by preeclampsia with and without intrauterine growth restriction. J Soc Gynecol Investig. 2004; 11:545–552.
31. Lassus P, Turanlahti M, Heikkila P, Andersson LC, Nupponen I, Sarnesto A, et al. Pulmonary vascular endothelial growth factor and Flt-1 in fetuses, in acute and chronic lung disease, and in persistent pulmonary hypertension of the newborn. Am J Respir Crit Care Med. 2001; 164:1981–1987.
32. Bhatt AJ, Pryhuber GS, Huyck H, Watkins RH, Metlay LA, Maniscalco WM. Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 164:1971–1980.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download