Abstract
Purpose
This study was conducted to examine the effects of osteoporosis prevention education on Korean breast cancer patients' knowledge and health promoting behavior.
Methods
The participants in this study included breast cancer patients who were registered at a self-help group organized by the Breast Cancer Center of a university hospital in Seoul, Korea. The intervention group received 60 minutes'didactic instruction followed by 30 minutes' interactive session, and reinforcement education with leaflets was given three weeks after the group intervention. In order to measure the effects of the intervention, this study used valid and reliable scales on the knowledge of osteoporosis and health promoting behavior for preventing osteoporosis. A post-test was conducted 12 weeks after the intervention.
Results
The results showed significant improvement in three of the five factors of osteoporosis knowledge including bone physiology, the characteristics of osteoporosis, and preventive behaviors in the intervention group. Overall health promoting behavior for preventing osteoporosis had significantly increased in the intervention group compared to the control group.
Osteoporosis is a progressive systemic bone disease caused by an imbalance between osteogenesis and osteolysis, resulting in a decrease in bone mass and density, which can increase the risk of fractures. One-third of menopausal women are affected worldwide[12]. Two major osteoporosis risk factors are reduced bone mass, which is formed during adolescence and adulthood, and rapid bone loss due to aging and menopause [3]. When middle-aged women develop a fracture caused by osteoporosis, they are suffering not only a physical disability but also a mental disability, such as increased social isolation and depression, due to decreased ability for daily living activities and soaring medical care costs [45]. Considering medical perspectives and social problems, it is critical to detect bone loss at the early stage after middle age, provide appropriate intervention, and prevent or delay complications. However, symptoms of osteoporosis or bone loss rarely appear before it they have advanced to the fracture stage[6]. Therefore, one of the best ways to prevent such complications is to take corrective action through early detection of high-risk groups of women who are vulnerable to fracture[7].
Breast cancer is the second most common form of cancer among women in Korea, and the number of women with breast cancer is increasing steadily[89]. Among women with breast cancer, those who receive medical treatment that adversely affects the skeletal system are highly vulnerable to develop osteoporosis [10111213]. Chemotherapy for breast cancer directly reduces bone mineralization and indirectly deteriorates ovarian function in pre-menopausal women, resulting in decreased concentrations of estrogens and an increased risk of osteoporosis. Furthermore, hormone replacement therapy decreases bone density, and radiation therapy can increase the risk of rib fracture[13]. As a result, women with breast cancer have bones that are more prone to fracture[14151617]. Therefore, women with breast cancer should understand the importance of preventing osteoporosis and actively follow health promoting behavior conducive to prevent osteoporosis.
Little research has been conducted on preventing and managing osteoporosis in women with breast cancer in Korea. Among the few studies, the majority have been survey-based and focused on the importance of osteoporosis education[311]. They did not apply education as an intervention but compared the interventional effect between intervention and control groups. Study was conducted to identify the effect of an osteoporosis educational intervention on osteoporosis knowledge and health promoting behaviors in patients with breast cancer and to allow patients to manage their own health conducive to preventing osteoporosis. The specific objectives of this study was to compare the osteoporosis knowledge and behavior of intervention group to those of control group.
This study had a nonequivalent control group design with pretest and posttest to identify the effect of osteoporosis preventive education on knowledge and behavior conducive to promoting bone health in patients with breast cancer.
Subjects were recruited from February to May 2011 from a breast cancer self-help group organized by the breast cancer center of a university hospital in Seoul, Korea. The inclusion criteria were (a) a breast cancer diagnosis, (b) finish the cancer treatments, (c) no experience of formal education about osteoporosis, and (d) agree to participant in this study. Exclusion criteria were (a) no metastasis, (b) no current surgical, chemotherapy, and/or radiation therapy.
Sample size was estimated with G*Power 3.1 at a .8 effect size, a .05 significance level, and .95 of test power. The intervention and control groups needed 35 subjects[18]. However, considering the possible attrition rate due to the data collection method (mail survey), 96 subjects were recruited, which was 40% more than required. 48 subjects who could participate at the group education were conveniently allocated to the intervention group, and the other 48 subjects were allocated to the control group.
Group education and self-help activity instruction were provided to the intervention group. The group education intervention was offered as a 90-min structured lecture and the topics included physiology of the skeletal system, characteristics and risk factors for osteoporosis, and improving bone health and preventive behaviors for osteoporosis. Instructional media used for group education included a 60-min lecture and a 30-min question-and-answer session.
The educational material for the intervention group were developed by researchers in this study based on a literature review, and the content validity was tested by a physician who specializes in endocrinology and two nursing faculty.
The second education intervention included self-care educational activities, such as diet and exercise, using an educational leaflet, which was sent to the subjects via mail 3 weeks after the group education. The reason for sending the educational materials three weeks later was that it is considered a critical time when the effect of group education decreases[19]. The educational leaflet developed by the breast cancer center of the hospital under study was called 'Osteoporosis: You should take care of your bones while you have healthy bones' and consisted of the definition, risk factors, major symptoms and problems, diagnosis, treatment and prevention of osteoporosis, changes in bone density with age, symptoms of fractures caused by osteoporosis, nutrition and diet management for osteoporosis, and a self-diagnostic index for osteoporosis risk-factors. After sending the educational materials to the subjects, it was confirmed whether or not the subjects received the materials, and they were encouraged by telephone to perform self-care activities according to the instructions.
The osteoporosis knowledge was measured with an instrument developed by Choi et al.[20], consisting of 31 items divided into five factors of bone physiology (5 items), characteristics of osteoporosis (6 items), risk factors (5 items), improving bone health (5 items), and preventive behaviors (10 items). This instrument was developed to measure the level of knowledge and awareness of osteoporosis. In this study it was measured on a 3-point scale, with yes, no, and do not know. A correct answer was given one point and a wrong or "do not know" answer was given zero points. Possible rage of mean score was 0 to 1, and higher score indicated better the knowledge of osteoporosis. At the time of tool development, Cronbach's α was .95, whereas Cronbach's α for this study was .76.
Health promoting behavior was measured by a tool originally developed by Yeum[21] and modified by Yoon[22]. The tool was comprised of 18 items in three subcategories of diet, exercise, and unhealthy food intake. To assess the frequency of each behavior, 4-point scale (1=less than once per week, 2=once to twice a week, 3=three to four times per week, and 4=more than five times per week) was used, and higher mean score indicated a better healthy lifestyle. At the time of tool development, Cronbach's α was .79, whereas Cronbach's α for this study was .76.
This study was approved by the Institutional Review Board of the university hospital where data was collected (No. CUMC11UO40). A full explanation of the study purpose, procedures, and advantages and disadvantages resulting from participating in the study was given to the participants, and they were informed that all information and data would be treated with complete confidentiality and would not be used for any purpose other than for this study. After the study was completed, the education material was sent to those in the control group.
The pretest was conducted on the appointment day at the outpatient clinic with those who agreed to participate and after they signed a consent form. The posttest was conducted via mail twelve weeks after the pretest.
Of the 48 participants allocated to the intervention group, eight did not complete the group education and twelve did not participate in the posttest, resulting in 28 participants in the intervention group, whereas 19 participants in the control group did not participate in the posttest, resulting in 29 participants in the control group. Total data of 57 was collected from both intervention and control groups.
No differences were found between the intervention and control groups in terms of general characteristics, such as age, education, having a spouse, or health-related characteristics, such as height, body weight, menstrual history, and fracture experience (Table 1).
The pretest results indicated a significantly lower osteoporosis knowledge level in the intervention group than that in the control group (p=.010), and improving bone health factor appeared to be statistically lower in the intervention group (p=.032). No difference in the overall health promoting behavior score was observed between the groups on the pretest. However, among the subcategories of health promoting behavior, the intervention group was more likely to score low on diet (p=.027) and exercise (p=.015) than those in the control group on the pretest (Table 2).
The ANCOVA (factor: group; covariate: pretest score of osteoporosis knowledge) was performed to assess the effect of education intervention compared to control on score change at the end of intervention. As shown in table 3, there was significant changes that osteoporosis knowledge of intervention group had significantly increased as compared to the control group (p<.001). In the three of the five factors of osteoporosis knowledge, including bone physiology, characteristics of osteoporosis, and preventive behaviors, the mean scores of the intervention group were significantly increased compared to the control group.
The ANCOVA (factor: group; covariate: pretest score of health promoting behavior) revealed that the mean score of the health promoting behavior of the intervention group had significantly increased those of the control group (p<.001). In the exercise subcategory of health promoting behavior, mean score of the intervention group was significantly increased as compare to the control group (p<.001). However, there was no significant differences between two groups on the subcategory of unhealthy food intake (Table 4).
As the overall five year breast cancer survival rate is increasing, the need to understand and manage the long-term effects of chronic diseases is growing[23]. Therefore, this study was conducted to identify the effect of osteoporosis preventive education on the osteoporosis knowledge and health promoting behavior in patients with breast cancer in Korea.
Our findings demonstrate that the knowledge level increased significantly in the intervention group compared to that in the control group. It was not possible to compare our results to those of other studies, as no study has been conducted on osteoporosis preventive education using patients with breast cancer. However, our results were consistent with another study done in male subjects who had received a 90-min osteoporosis education program. Changes in knowledge level were measured three weeks later and showed an increase in osteoporosis knowledge level[24]. Another study with young female subjects, who had received a 45-min group education program with additional education using a booklet for calcium and vitamin D intake, also demonstrated an increase in knowledge eight weeks after the intervention[25]. However, the results of that study did not agree with those of a study done with elderly subjects who received a 60-min osteoporosis education program with slides and booklets, followed by 30-min of reinforcement instruction one year after the initial education. Gaines et al.[26], measured knowledge levels one and two year after an education intervention and did not show any significant gain in knowledge. Existing studies and our study may be different, as no substantial diversity in the frequency or length of time to provide education was used, and the difference might result from different subject age brackets or the time that the posttest was conducted. Therefore, the frequency and method of intervention implemented in our study was effective for female patients in their fifties to gain knowledge. Further studies should focus on repeated measurements to determine when the most appropriate time point is to reinforce education and consolidate the effect of education.
The results demonstrate that the health promoting behavior scores were significantly higher in the intervention group than those in the control group 3 months after intervention[24]. In contrast, two studies did not show any improvement in health behavior. One study [27] was conducted with pre-menopausal women who received a two hour per week educational intervention over four weeks using leaflets containing diet, exercise, cigarette smoking, and calcium intake information. Behavioral changes were measured two year after the intervention and showed no change in health behavior. Another study with elderly subjects also showed no change in behavior[26]. A possible explanation for the discrepancy may be different time points to effectively assess the intervention. In other words, Tung and Lee [24] measured behavioral changes three weeks after the intervention, whereas both Gaines et al.[26], and Winzenberg et al.[27], measured changes two year after the intervention. We measured behavioral changes three months after the intervention. Therefore, other studies focusing on repeat education and/or reinforcement education every three months to maintain educational effectiveness emphasized that the effect of education intervention on behavioral change appears to increase three months after an intervention but declines thereafter[19].
More specifically, we demonstrated that although female patients with breast cancer participated in significantly less physical exercise since the intervention, no behavioral changes in dietary habits were observed among the health promoting behavior subcategories. These findings are not consistent with a study on osteoporosis by Chan et al.[28], on women in Hong Kong. Although they applied a similar intervention to that used in our study, the dietary habit change improved one month later the intervention, but physical exercise, which focuses on a combined intervention of lectures with exercise therapy, did not improve. A change in dietary habits can occur in a relatively short time, whereas education-induced changes in exercise frequency cannot be accomplished with only one education intervention. The improvement in exercise performance in our study resulted from the education intervention and self-care activities. Further studies on the effectiveness of self-care activities to prevent osteoporosis are needed.
We revealed no difference in unhealthy food or drink intake, such as caffeine, carbonated drinks, alcohol, and tobacco, in the intervention group before and after the intervention. No difference was observed between the two groups before and after the intervention. Sedlak et al.[29], investigated osteoporosis prevention in female college students living in a community with nurses. That study showed that only the college group, which received intensive education intervention on caffeine intake, significantly decreased caffeine intake after the intervention. This result indicates that providing an education intervention once is not expected to change behavior, as a repeated and enriched educational approach to change behavior was demanded for addictive substances.
Our results demonstrate that osteoporosis preventive education provided in a group and including self-care activities for patients with breast cancer appeared to improve patient knowledge and behavior conducive to preventing osteoporosis and was significantly effective for improving and changing physical exercise behaviors. Therefore, the significance of the results for nursing science can be explained by the relationship between breast cancer and osteoporosis emphasized in other studies. Health education to prevent osteoporosis should be provided as early as possible during breast cancer treatment. The education should take all measures to prevent osteoporosis and to transfer the patient's knowledge into action. This study appeared to play a critical role inducing voluntary participation of patients in self-care activities. We suggest that nurse specialists, such as advanced practice registered nurses with expertise in oncology, should be involved in the program to support the patients with breast cancer and enhance their self-care activities.
Figures and Tables
Table 1
Homogeneity Test of Characteristics of the Subjects

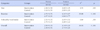
Table 2
Homogeneity Test for Research Variables

Table 3
Effect of Group Education on Osteoporosis Knowledge (N=57)

Table 4
Effect of Group Education on Health Promoting Behavior for Osteoporosis (N=57)
References
1. Hadji P. Reducing the risk of bone loss associated with breast cancer treatment. Breast. 2007; 16(3):S10–S15. DOI: 10.1016/j.breast.2007.10.004.

2. Korean Society for Bone and Mineral Research. Physician guide for diagnosis and treatment of osteoporosis. Seoul: Korean Society for Bone and Mineral Research;2008. p. 131.
3. Camacho PM, Dayal AS, Diaz JL, Nabhan FA, Agarwal M, Norton JG, et al. Prevalence of secondary causes of bone loss among breast cancer patients with osteopenia and osteoporosis. J Clin Oncol. 2008; 26(33):5380–5385. DOI: 10.1200/JCO.2008.17.7451.

4. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17(12):1726–1733. DOI: 10.1007/s00198-006-0172-4.

5. Shin CS, Cho NH, Kim Y, Kim SW, Park JH, Kim MH, et al. Study of an osteoporosis management program in Korea. Research Report. Seoul: Korea Health Promotion Foundation;2007. 07.
6. Munch S, Shapiro S. The silent thief: Osteoporosis and women's health care across the life span. Health Soc Work. 2006; 31(1):44–53. DOI: 10.1093/hsw/31.1.44.

7. Han CH, Kwon DJ, Kim JH. Association of LRP5 gene polymorphisms with bone mineral density and bone responsiveness to hormone therapy in postmenopausal Korean women. Korean J Obstet Gynecol. 2007; 50(8):1115–1124.
8. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, et al. Cancer statistics in Korea: Incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010; 25(8):1113–1121. DOI: 10.3346/jkms.2010.25.8.1113.

9. National Cancer Center. Report No.: 11-1352000-000145-10. Annual report of cancer statistics in Korea in 2011. Annual Report. Seoul: Ministry of Health and Welfare;2013. 12.
10. Cheung AM, Heisey R, Srighanthan J. Breast cancer and osteoporosis. Curr Opin Endocrinol Diabetes Obes. 2013; 20(6):532–538. DOI: 10.1097/01.med.0000436195.10599.dd.

11. Hadji P, Ziller M, Alber US, Kalder M. Assessment of fracture risk in women with breast cancer using current vs. emerging guidelines. Br J Cancer. 2010; 102(4):645–650. DOI: 10.1038/sj.bjc.6605548.

12. Peppone LJ, Mustian KM, Rosier RN, Carroll JK, Purnell JQ, Janelsins MC, et al. Bone health issues in breast cancer survivors: A Medicare Current Beneficiary Survey(MCBS) study. Support Care Cancer. 2014; 22(1):245–251. DOI: 10.1007/s00520-013-1967-4.
13. Hirbe A, Morgan EA, Uluckan O, Weilbaecher K. Skeletal complications of breast cancer therapies. Clin Cancer Res. 2006; 12(20 Pt 2):6309s–6314s. DOI: 10.1158/1078-0432.CCR-06-0652.

14. Chen Z, Maricic M, Bassford TL, Petting M, Ritenbaugh C, Lopez AM, et al. Fracture risk among breast cancer survivors: Results from the women's health initiative observational study. Arch Intern Med. 2005; 165(5):552–558. DOI: 10.1001/archinte.165.5.552.
15. Choksi P, Williams M, Clark PM, Van Poznak C. Skeletal manifestations of treatment of breast cancer. Curr Osteoporos Rep. 2013; 11(4):319–328. DOI: 10.1007/s11914-013-0179-7.

16. Edwards BJ, Samaras A, McKoy JM, Boyle S, Bennett CL. Als: implications for fractures in perimenopausal women with breast cancer. Community Oncol. 2008; 5(11):625–626.
17. Tsai CH, Muo CH, Tzeng HE, Tang CH, Hsu HC, Sung FC. Fracture in Asian women with breast cancer occurs at younger age. Plos One. 2013; 8(9):e75109. DOI: 10.1371/journal.pone.0075109.

18. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2):175–191.
19. Lee HY, Kim SY. The effect of education for prevention of osteoporosis patients with bone fracture. J Korean Acad Nurs. 2001; 31(2):194–205.

20. Choi E, Kim J, Chung M, Hwang K. Development of as osteoporosis awareness scale for women. J Korean Acad Nurs. 2008; 38(6):813–821. DOI: 10.4040/jkan.2008.38.6.813.
21. Yeum SK. A study on the relation of cognitive-perceptual factors and behaviors about middle age women's health promotion- focus on the prevention of osteoporosis. [dissertation]. [Seoul]: Chung-Ang University;1996. 101.
22. Yoon EJ. The model explaining variance in and quality of life in women with osteoporosis. [dissertation]. [Seoul]: Kyung Hee University;2001. 142.
23. Mols F, Vingerhoets AJ, Coebergh JW, Van de. Quality of life among long-term breast cancer survivors: A systematic review. Eur J Cancer. 2005; 41(17):2613–2619. DOI: 10.1016/j.ejca.2005.05.017.

24. Tung WC, Lee IFK. Effects of an osteoporosis educational programme for men. J Adv Nurs. 2006; 56(1):26–34. DOI: 10.1111/j.1365-2648.2006.03976.x.

25. Bohaty K, Rocole H, Wehling K, Waltman N. Testing the effectiveness of an educational intervention to increase dietary intake of calcium and vitamin D in young adult women. J Am Acad Nurse Pract. 2008; 20(2):93–99. DOI: 10.1111/j.1745-7599.2007.00281.x.

26. Gaines JM, Narrett M, Parrish JM. The effect of the addition of osteoporosis education to bone health screening program for older adults. Geriatr Nurs. 2010; 31(5):348–360. DOI: 10.1016/j.gerinurse.2010.04.011.
27. Winzenberg T, Oldenburg B, Frendin S, De Wit L, Riley M, Jones G. The effect on behavior and bone mineral density of individualized bone mineral density feedback and educational interventions in premenopausal women: A randomized controlled trial. BMC Public Health. 2006; 6:12. DOI: 10.1186/1471-2458-6-12.

28. Chan MF, Ko CY, Day MC. The effectiveness of an osteoporosis prevention education programme for women in Hong Kong: A randomized control trial. J Clin Nurs. 2005; 14(9):1112–1123. DOI: 10.1111/j.1365-2702.2005.01224.x.
29. Sedlak CA, Doheny MO, Jones SL. Osteoporosis education program: Changing knowledge and behaviors. Public Health Nurs. 2000; 17(5):398–402. DOI: 10.1046/j.1525-1446.2000.00398.x.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download