Abstract
Purpose
The purpose of this study was to explore practice-based evidence for health promotion in vulnerable populations with hypertension in primary health care settings.
Methods
Two methodological procedures were adopted for this triangulation study. In the first phase, the sample was obtained from the computerized clinical data repository of a community nursing center. A total of 286 clients were assessed for hypertension as an actual circulation problem as coded in the Omaha System. In the second phase, a qualitative focus group was surveyed through semi-structured interviews conducted by nine advanced practice nurses who had been serving the hypertensive patients.
Results
The community nurses provided essential primary healthcare services including health teaching guidance and counseling, and surveillance to vulnerable populations living in medically underserved community. There was a significant positive correlation between knowledge and behavior (r=.53, p<.01), between knowledge and health status (r=.40, p<.05), and between behavior and health status (r=.48, p<.01).
Conclusion
This triangulation study encompassed not only quantitative findings from the computerized records of clients but also other information acquired from advanced practice nurses. This study contributes to understanding the importance of health promotion nursing interventions even with populations already diagnosed with chronic diseases such as hypertension.
High blood pressure (HBP) is a common, powerful, and independent risk factor for cardiovascular disease (CVD)[1]. Efforts to prevent morbidity and mortality from chronic diseases, including HBP, have largely focused on drug therapy and required much expense[1]. Depending on pharmacologic management alone, however, raises several problems related to blood pressure control[25]. First, drug therapy for HBP requires endless cycle of detection, treatment and maintenance. Second, drug therapy can cause side effects, can be expensive, and can effectively control BP for only about 50% of those treated in the US[3]. Furthermore, a lack of access to health care in some population groups and lack of adherence to BP-lowering medication are a major reason for poor control of HBP worldwide and hinder the potential effectiveness of drug therapy[4]. Despite progress in prevention, detection, treatment, and control HBP remains an important public health problem. The Writing Group of the PREMIER Collaborative Research Group[5] conducted a randomized clinical trial to determine the effects of comprehensive lifestyle intervention programs on BP and established recommendations with scientific rationale for the lifestyle modifications that can reduce BP and prevent and control other chronic conditions such as CVD.
The need for clinical management of HBP through accessible community health resources that include early detection, medication adherence, maintenance of health status and HBP treatment is considerable. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure recommended that lifestyle modifications should be extended to non-hypertensive individuals[6]. The latest recommendations for management of HBP have considerably emphasized individual's promoting health through the modification of their lifestyle in community settings[720]. Although lifelong diseases such as HBP usually cannot be cured, in most cases they can be prevented and controlled toward higher level of health with healthy lifestyle modifications[589101119]. Among the strategies used to promote health knowledge, behavior, and status, nursing practice interventions in primary health care appears to offer a promising avenue to better meet the needs of vulnerable populations with HBP[10]. The purpose of this study was 1) to describe the nursing interventions related to health promotion in adults with HBP in a community nursing center (CNC) based on evidence recommended by practice extant; 2) to identify the relationships between the nursing diagnoses, nursing interventions, and outcomes related to HBP as represented by the Omaha System (OS) in a CNC; 3) to explore nurses's opinions in relation to the quantitative findings of health promotion in adults with HBP using the OS in the CNC.
Two methodological procedures were adapted for this triangulation study: 1) a quantitative approach of practice-based evidence from clinical information system; and 2) qualitative approach of expert opinions from a focus group interview to provide a critical validity check on quantitative method.
The setting of this study was a community nursing center (CNC) located in a low-income, urban neighborhood in Wisconsin. The population for the quantitative clinical data study was limited to client records from this CNC coded with a standardized nursing terminology based on the Omaha System (OS). The sample for this quantitative analysis was the computerized client records data set from the CNC. Criteria for inclusion of client records in the study were clients over 18 years of age who were diagnosed with the circulation problem of "Abnormal BP reading" according to the OS. The records of 286 hypertensive clients were selected for the study from a total of 3,963 clients served at the urban community nursing center.
This nursing diagnosis had to be coded as an actual problem during at least one CNC encounter for a client to be included in the study. Actual BP values readings were not assessed for client inclusion in the study. Although it is possible that an abnormal BP reading could be coded in the OS for Low BP as well as HBP, according to CNC nursing staff interviewed including the director of the CNC during the entire study period, the use of "abnormal BP" as an OS code in the CNC client's records at this CNC always indicated HBP.
Qualitative research approaches, such as focus group interviews, can provide a critical validity check on quantitative (statistical) methods. Evidence-based nursing practice (EBP) relies not only on published materials, valid research findings, but also on clinical records, expert opinions, and community standards[12]. In this case, the researcher felt that it was important to solicit data including the nurses' professional opinions in relation to clinical documentation of health promotion in adults with HBP from the nurses who were involved in the practice and coding of the data analyzed for the study.
The only inclusion criteria for focus group inclusion was that the participants were registered nurses who provided nursing services to clients at the CNC. A purposive sampling was adopted to recruit participants. Potential focus group members included a co-worker (an executive administrator) and ten registered nurses who provided services to clients at the CNC. Invitation letters to join the focus group discussion were sent to the ten advanced practice nurses (APN) explaining the purpose of the study and procedures and contents.
The nine APNs agreed to participate in the focus group interview. The total sample included two doctoralprepared nurses, two doctoral candidate nurses, and five master-prepared nurses in nursing. The use of focus groups for idea generates that participants in a group interaction with each other enrich data generation[22] The focus group interview lasted approximately 90 minutes. An informal, semi-structured group interview method was used. The group session was audio-taped and the interview was transcribed verbatim.
The University of Wisconsin-Milwaukee (UWM) Automated Community Health Information System (ACHIS) was the data collection tool used for the phase one of the study. The ACHIS was developed by Lundeen and her research team[13] to document the broad scope of services provided by nurses in a CNC. The ACHIS utilized the OS, a nursing taxonomy developed by Martin and Scheet[14]. The ACHIS enabled the CNC nurses to code nursing focus areas of nursing diagnoses, target areas of nursing interventions and outcome evaluations, as well as traditional treatment of acute and chronic problems. The ACHIS clinical data was coded by community health nurses and APN who had extensive and continuing training for the OS. Reliability was reported by Martin and Scheet[1415], the developers of the OS, through an independent review of randomly-selected records using the OS Problem Classification Scheme (PCS). Inter-rater reliability was also reported for use during the clinical practice, with correlations ranging from 0.53 for knowledge to 0.86 for status. The Problem of Rating Scale for Outcomes (PRSO) is a 5-point Likert scale by which the nurse rates the patient's knowledge, behavior and status relative to an identified problem [14]. The Knowledge, Behavior, and Status subscales of the OS, Outcomes Rating Scale also have been evaluated for inter-rater reliability and content validity[14151622]. Psychometric analysis of the OS revealed acceptable content validity and inter-rater reliability. Clinical data are coded by nurses in the course of their daily practice using the OS codes and stored in a computerized database as a part of the ACHIS. The OS served to standardize the process of data collection, classification and analysis for this study.
Clinical data were abstracted from the relational data repository created for the ACHIS. A data file was created that linked all of the nursing interventions provided to CNC clients to nursing diagnosis, modifiers and outcome rating scale data. The sample represents all CNC clients for this study with "Abnormal blood pressure" coded under the OS focus area of "Circulation." Analysis using cross tables, χ2 test of independence, was conducted to examine the prevalence of HBP and client demographics factors. Nursing care elements of nursing problems, interventions and outcome variables based on the OS were analyzed using descriptive statistics, bivariate correlation and Wilcoxon Matched Pairs Signed Ranks test with the Statistical Package for Social Sciences.
The analysis of the qualitative data collected from the focus group discussion started immediately after the focus group session. The principal investigator reviewed notes and observations about the intensity of the discussion and the nonverbal behaviors showed during the group discussion. A written record of this meeting was used to supplement the data obtained from the recorded voice records. Focus group discussion was transcribed by a graduate student and the principal investigator examined the data in detail.
To get a better sense from the data, the principal investigator listened to the recorded interviews repeatedly, reread the manuscript several times and noted self reflections. The principal investigator chose to analyze the interview by reviewing the entire narrative for themes that reflected the key elements of the discussion. Major categories were identified and refined throughout the process. Each successive reading resulted in a more succinct categorization of participants' statements and some new insight into the meaning of the data related to the quantitative findings. For qualitative data analysis, a form of content analysis called thematic analysis was used.
The research protocol for the quantitative research was approved as exempt by UWM Institutional Review Board (IRB) for the Protection of Human Subjects. This study was considered exempt under category four since it involves only analysis of pre-existing data. The principal investigator for this secondary analysis has no contact with participants. Ethical approval also was obtained from IRB at UWM (IRB#: 06.004) for the protocol of the focus group. The purpose and procedure of the focus group discussion were explained to the participants. Each participant provided written consent to being audio-taped. Participants were informed that they could leave the group or end the interview at any time. Assurance was made that data being published would not be attributable to a particular individual.
The sample was obtained from the computerized clinical data repository for the CNC. The sample included the records for a total of 286 clients aged over 18 years who were assessed with HBP as an actual circulation problem. This sample of 286 adults ranged in age from 18 to 93 years with a mean age of 52.9 years. There was a higher percentage of females (67.51%), and African Americans (53.81%) in the total sample than males (31.83 %) or Caucasian (42.73%). The racial/ethnic distribution was African American (53.81%), Caucasian (42.73%), Hispanic or Latino heritage (1.02%), and Native Americans (0.74%). A total of 29.03% of the clients were married. Income was a missing variable for about 59% of the sample; of the 40% with income coded, 39% reported annual family income of less than $25,000. Demographic characteristics for the study sample are presented in Table 1.
There are significant associations in gender (χ2=16.42, p<.001), age (χ2=282.01, p<.001), and ethnicity groups (χ2=49.22, p<.001), indicating that male clients older than 61years in this population were most likely to be assessed with HBP. There is also greater HBP prevalence in the Caucasian clients than in the group of the African American clients in this CNC population (Table 2).
The nurses at the CNC documented nursing practice using the OS Intervention Scheme (IS). Multiple nursing interventions can be provided and documented for each nursing diagnosis assessed by CNC nurses. A total of 35,424 nursing interventions were provided for the study sample in the intervention categories of Teaching Guidance and Counseling (n=17,207, 48.61%), Treatment and Procedures (n=2,803, 7.94%), Case Management (n=7,150, 20.22%) and Surveillance (n=8,264, 23.33%) (Table 3).
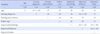
The relationships among the variables of client age, health problems of nursing diagnoses, number of nursing interventions, number of follow-ups and improved scores of knowledge, behavior, and status outcomes were tested using Pearson correlation coefficients (Table 4).
There is a weak negative correlation between client age and the number of the health problems identified with HBP (r=-.27, p<.01) indicating that as the age of clients is younger, the number of the health problems increases. There is a moderate negative correlation between the health problems identified with BP and improved behavior (r=-.58, p<.01) indicating that as the number of the health problems increases, the level of the improved healthy behavior decreases. There are also significant positive correlations between improved knowledge and improved behavior (r=.53, p<.01), improved knowledge and improved status (r=.40, p<.05), and improved behavior and improved status (r=.48, p<.01).
In order to gain further perspective on the quantitative findings in this study a focus group session was conducted with the CNC nurses who participated in coding the OS data analyzed. The semi-structured interview questions used to guide group discussion are provided for the nine APN. In the group interview, the nurses were asked to review the populations' demographic characteristics.
In the group interview, the nurses were asked to review the populations' demographic characteristics. Although the majority of African American adults with HBP for whom there was financial information (n=57) had less than $11,999 annual income, nearly 60 percent of the annual income data were missing in the data base. One respondent observed:
One comment about your demographics… we never coded income very well… It seems very uncomfortable when you are trying to establish a relationship with someone to automatically ask someone's income, and then you never get back to it. It felt like it gets in the way of establishing relationships… there were so many people that were low income. Virtually 96% were under $25,000 a year. Virtually everyone. We didn't ask the question, because we just assumed they were low income; everybody was.
Among the four categories of nursing interventions, the category of Teaching, Guidance and Counseling was the intervention coded most frequently (n=2,011, 45.5%) as a health promotion intervention by CNC nurses for adult clients with HBP. The nurses were asked to comment on this issue specifically in relation to medication management with the question "What is your role in controlling BP if you are not the primary medical provider? And how do you see the role of nursing in the CNC?"
You [the nurse] do all the teaching, you do all the assessing for side effects, you do all the physical exams for high blood pressure… And you know what they might have been on. So you review what the side effects are…a lot of teaching…So you do everything [related to medication management] by teaching except write the actual prescriptions.
The focus group participants reviewed the findings, including the frequencies of nursing intervention in teaching, counseling and guidance, including physical exams with signs and symptoms. Findings related to nursing diagnoses, interventions, and outcomes of nursing service for the vulnerable population from the nurses' perspectives in the major focus areas of health promotion and HBP were identified. These five themes are as follows: 1) establishing rapport is a key with vulnerable populations; 2) health education is central to nursing services for health promotion; 3) holistic approaches are necessary for the vulnerable population; 4) reasons exist that explain more health problems with younger clients; and 5) external factors affect nursing services (grants and programs) at the CNC.
This study was conducted with two phases: 1) practice based-evidence related to health promoting nursing services for vulnerable population with HBP living in a inner city in Milwaukee; 2) a focus group interview to increase the validity of the results from the quantitative approach. In the first phase of the study, practice-based evidence documented by nurses in a community nursing center was analyzed to determine the nursing process elements, including diagnoses, interventions, and outcomes, related to health promotion with vulnerable adult clients with HBP as coded in the OS. A quantitative method was used to examine a subset of the standardized clinical data drawn from a clinical data repository.
In the second phase, a focus group session was conducted to validate the quantitative clinical findings with the nurse clinicians who collected the data. The CNC nurses were invited who participated in the clinical documentation with coding the OS data and asked to provide feedback on the statistical findings. The purpose of the focus group was to solicit these CNC nurses' feedback on factors that might have affected their nursing practice or their coding of data and to solicit their comments on the quantitative findings. The focus group allowed the principal investigator to review the preliminary quantitative findings of the data and to glean from nurses' interpretations and opinions about the findings.
Nurses serve as primary care givers and advocates for the population served by the CNC and promote health for all clients regardless of socioeconomic status and ethnic backgrounds by providing a comprehensive set of services[171819]. A two-year trial evaluation study addressed the importance of a health care provider's role as an educator in primary settings to increase patient's knowledge about risk factors associated with HBP and to increase ability of adherence to HBP regimen[1718]. The researchers recommended that as the level of knowledge increases, it may affect positive changes in health behaviors. For this study, health teaching, counseling, lifestyle modifications, nursing case management, health promotion, and surveillance of chronic condition variables are selected from the health promotion principles.
This triangulated design of research included two approaches. The first phase included a secondary data analysis of selected data elements from an aggregated client database for a community nursing center, as coded in the OS. In the final phase a qualitative focus group method was used to further clarify and maximize the validity of the findings of the quantitative analysis. The qualitative research approach is a means of exploring the depth, richness, and the inherent qualities of the complexity in the phenomena. This study provided practice-based evidence related to health promotion practices in adults with HBP from nursing documentation coded by the OS in a primary setting and professional opinions related to health promotion with chronic disease such as HBP from the focus group interview.
Significant positive correlations between improved knowledge and positive changes in behavior, improved knowledge and improved status, and positive changes in healthy behavior and improved status were found in the CNC data. These findings highlight the importance of health teaching as a key nursing intervention in adults with HBP.
The nature of the analysis of the focus group data was determined by the research questions and the purposes for which the data are collected. The focus group data provided valuable information that could not possibly be obtained from the quantitative findings. The participants in the focus group session helped the researcher to better understand the population characteristics that are a critical part of interpretation. The nurses stated that without the primary health care services from the CNC in that area, there would be no health prevention or health promotion services for the this vulnerable population.
This triangulation study encompasses not only research findings from quantitative and quantitative data, but also other information acquired from a standardized nursing taxonomy such as the OS. The use of triangulation approach was useful in terms of increasing validity, capturing more complete, holistic depiction of nursing practice. This study adds to the understanding of the importance of health promotion nursing practice even with populations already diagnosed with chronic diseases such as HBP and contribute to understanding the significance of nursing research with hypertensive patients to make sound health policy for chronic disease management in community settings.
Figures and Tables
Table 1
Demographic Characteristics of the Study Subjects (N=286)

Table 2
Relationship of the Prevalence of HBP and Client Characteristics

Table 3
Nursing Interventions Identified in the OS Categories (N=35,424)

Table 4
Correlations among Client Characteristics, Nursing Diagnoses, Interventions and Outcomes
References
1. Grover SA, Coupal L, Kaouache M, Lowensteyn I. Preventing cardiovascular disease among Canadians: What are the potential benefits of treating hypertension or dyslipidemia? Can J Cardiol. 2007; 23(6):467–473. DOI: 10.1016/S0828-282X(07)70786-9.

2. Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: The Suita study. Hypertension. 2008; 52(4):652–659. DOI: 10.1161/HYPERTENSIONAHA.108.118273.
3. Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, et al. Prevalence of hypertension in the US adult population: Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension. 1995; 25(3):305–313. DOI: 10.1161/01.HYP.25.3.305.
4. Domino FJ. Improving adherence to treatment for hypertension. Am Fam Physician. 2005; 71(11):2089–2090.
5. Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control. JAMA. 2003; 289(16):2083–2093. DOI: 10.1001/jama.289.16.2131.
6. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003; 42(6):1206–1252. DOI: 10.1161/01.HYP.0000107251.49515.c2.

7. U.S. Department of Health and Human Services. The seventh report of the joint national committe on prevention, detection, and treatment of high blood pressure. JNC 7. National high blood pressure education program. Washington, DC: National Institute of Health, National Heart, Lung, and Blood Institute;U.S. Department of Health and Human Services;2003. 12. Report No.: 03-5233.
8. Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ, et al. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. J Hum Hypertens. 2005; 19(1):21–31. DOI: 10.1038/sj.jhh.1001770.

9. Svetkey LP, Simons-Morton DG, Proschan MA, Sacks FM, Conlin PR, Harsha D, et al. Effect of the dietary approaches to stop hypertension diet and reduced sodium intake on blood pressure control. J Clin Hypertens (Greenwich). 2004; 6(7):373–381. DOI: 10.1111/j.1524-6175.2004.03523.x.

10. Hong WH. Evidence-based nursing practice for health promotion in adults with hypertension in primary settings [dissertation]. [Wisconsin]: University of Wisconsin-Milwaukee;2007. 226.
11. American Diabetes Association. Hypertension management in adults with diabetes. Diabetes care. 2004; 27:S65–S76. DOI: 10.2337/diacare.27.2007.S65.
12. Malloch K, Porter-O'Grady T. A new age for practice: Creating the framework for evidence. In : Malloch K, editor. Introduction to evidence-based practice in nursing and health care. 2nd ed. Sudbury, MA: Jones and Bartlett;2010. p. 115–207.
13. Lundeen SP, Friedbacher BE. The automated community health information system (ACHIS): A relational database application of the omaha system in community nursing centers. In : Grobe S, Pluter-Wenting E, editors. Nursing informatics: An international overview for nursing in a technological era. New York: Elsevier;1994. p. 23–31.
14. Martin KS. The omaha system: Application for community health nursing. Philadelphia: Saunders Company;1992. p. 258.
15. Martin KS. The omaha system: A key of practice, documentation, and information management. Philadelphia: Elsevier Saunders;2005. p. 484.
16. Martin KS, Norris J, Leak GK. Psychometric analysis of the problem rating scale for outcomes. Outcomes Manag Nurs Pract. 1999; 3(1):20–25.
17. Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, et al. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005; 57(1):5–14. DOI: 10.1016/j.pec.2004.03.011.

18. Bosworth HB, Olsen MK, Goldstein MK, Orr M, Dudley T, McCant F, et al. The veterans' study to improve the control of hypertension (V-STITCH): Design and methodology. Contemp Clin Trials. 2005; 26(2):155–168. DOI: 10.1016/j.cct.2004.12.006.

19. Hong WH, Lundeen SP. Using ACHIS to analyze nursing health promotion interventions for vulnerable populations in a community nursing center: A pilot study. Asian Nurs Res. 2009; 3(3):130–138. DOI: 10.1016/S1976-1317(09)60024-4.

20. Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: A cross-sectional study. BMJ Open. 2013; 3(8):e003423. DOI: 10.1136/bmjopen-2013-003423.

21. Blaha MJ, Kusz KL, Drake W, Elasy TA. Hypertension prevalence awareness, treatment and control in North Nashville. Tenn Med. 2006; 99(4):35–37.
22. Rubin HJ, Rubin IS. Qualitative interview. The auto hearing data. Thousand Oaks: Sage;1995. p. 385.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download