Abstract
Purpose
This study was to ascertain whether there are differences in health care utilization and expenditure for Type I Medical Aid Beneficiaries before and after applying Copayment.
Methods
This study was one-group pretest posttest design study using secondary data analysis. Data for pretest group were collected from claims data of the Korea National Health Insurance Corporation and data for posttest group were collected through door to-door interviews using a structured questionnaire. A total of 1,364 subjects were sampled systematically from medical aid beneficiaries who had applied for copayment during the period from December 12, 2007 to September 25, 2008.
Results
There was no negative effect of copayment on accessibility to medical services, medication adherence (p=.94), and quality of life (p=.25). Some of the subjects' health behaviors even increased preferably after applying for copayment including flu prevention (p<.001), health care examination (p=.035), and cancer screening (p=.002). However, significant suppressive effects of copayment were found on outpatient hospital visiting days (p<.001) and outpatient medical expenditure (p<.001).
The Medical Aid system in Korea that was introduced in 1977 is a national system designed to provide free medical services to those people who cannot afford to pay health insurance fees on their own and to guarantee the minimum standard of living of low-income households. Health Care Financing come from taxpayers' money and Medical Aid system have played a tremendous role in sustaining the quality of life for the poor by guaranteeing them free medical services in Korea.
Korea has continued to increase the number of subjects and the scope of Medical Aid in order to improve medical services benefits for the poor. This has led to an increase in the budget of the Korean government for Medical Aid from 2.4631 trillion won in 2004 to 4.6753 trillion won in 2008, which is an increase of 190% in the budget of the Medical Aid program. The budget is projected to grow to 20.5 trillion won by 2015[1].
The continually increasing financial burden on the program, due to the rapid increase in Medical Aid expenditures, is a potential risk factor for the viability of sustaining the Medical Aid system in Korea. This rapid increase in cost of the Korea Medical Aid system can be attributed to several factors including expanded number of recipients and the broadened scope of Medical Aid. However, the lack of awareness of medical expenditures by/of beneficiaries and medical service providers as well as the absence of strict post-management system for Medical Aid has also been considered significant factors in the rising costs[2].
The Korean government introduced the Copayments system for outpatient and pharmacy costs of the Medical Aid I Medical Aid Beneficiaries on July 1, 2007. These beneficiaries had previously been provided medical services for free. This Copayments system was implemented in order to stabilize the rapidly increasing financial burden on the Medical Aid and encourage appropriate medical care by recipient, regardless of outpatient and inpatient visitations. Under the Copayments system, the Medical Aid I Medical Aid Beneficiaries should make copayments, ranging from 1000 won to 2000 won, for outpatient treatment. However, the new system was criticized for ignoring the difficulties of patients' economic burden[3]. That is, Copayments can help to cut the financial burden of the Medical Aid program, but can limit medical access for the lower class due to their economic burden (even at a reduced rate), which leads to decreased health care accessibility for the general public. This would require careful management for Copayments[4,5]. In addition, it was reported that Copayments have worsened health care behavior of Copayment clients[6] and decreased adherence to medication prescription[7].
In light of the above criticism, the Ministry of Health and Welfare introduced a system to provide 6,000 won per Type I Medical Aid Beneficiary (72,000 won annually) to redress the drawbacks of the Copayments system to support the cost of maintaining a healthy life. By supplying the amount needed to keep a healthy life, the government is determining the outpatient cost on the beneficiary types and providing the amount for the Type I Medical Aid Beneficiaries. Then the balance of the cost is passed on to the beneficiaries. Therefore, the introduction of a system of financially supporting the cost of keeping a healthy life to beneficiaries is designed to lower the burden of Copayments and, at the same time, discourage medical service overuse by recipients. However, civic groups have defined Copayments as a policy which seriously violates the rights of health and life of Medical Aid Beneficiaries as well as a policy against human rights, because it maximizes class stigma by differentiating health insurance according to wealth. Additionally, they insist that Copayments should be abolished because accessibility of Medical Aid Beneficiaries to medical organizations is limited[8].
The purpose of this study is to define the effect of Copayments on accessibility to medical services, health behavior, medication adherence, QoL, medical visitation days and medical expenditure of Type I Medical Aid Beneficiaries.
This is one-group pretest-posttest design study using secondary data analysis. The data used in this study came from pre-existing 1s and 2nd large scale survey. In the 1st study surveyed on Dec 12, 2007[9], 2510 subjects were extracted using systematic sampling. For a systematic sampling method to select nationally representative samples, all administrative areas were divided based on population into large (1,000,000 population), medium (500,000 population) and small cities (50,000 population), and rural regions. In the 2nd survey, 1,364 people among 2,510 were followed[10]: Even though the exact reason for the drop-out were not examined, death and being newly included to other Medical Aid system to be excluded from the burden of copayment were guessed to be main causes. In summary, the subjects of this study were those who were applied copayment system from Dec 12, 2007 to September 25, 2008, the period between the two survey. For the medical service use, claims data submitted from medical institutions to the Korea National Health Insurance Corporation (NHIC) was used.
In both two survey on which this study is based, the Ministry sent an official mailing to potential participants, explaining the purpose and methods of the study and asking for their cooperation prior to data collection. Case managers gave more concrete explanations about the purpose while their home visiting was made. Data were collected after recipients agreed to participate in the study. To minimize data variation among case managers, they were educated regarding to data collection process.
For the research variables, accessibility to medical services, health behavior, medication adherence, Quality of life and medical variables were included corresponding to the aim of case management of Korean ministry of health and welfare[9].
The degree of limits in medical services use due to The Copayment System was measured in the following categories: very limited, limited, uncertain, not limited, and not limited at all.
Health behavior was measured in three categories: health examination, vaccination for influenza, and cancer screening[10]. The number of recipients who undertook those health behaviors before and after applying copayment was compared.
Medication adherence is defined as a concept related to medication, which means the level of medication patients take as prescribed[11]. One of the leading tool for medication adherence is Morsky tools[12] was revised by Case Management Society of America (2007) into six different questions[13]. This tool was reorganized into 5 items by extracting 1 item which is thought to be redundant conceptually. Each item was scored based on the five-point Likert scale (range, 1~5) indicating that the higher point represents more desirable health behavior. The result from this survey showed high reliability (Cronbach's α=.89).
QoL was measured using the QoL for Medical Aid Beneficiaries developed by Shin et al.[9] The tool used was made up of 8 categories (28 items): physical function (9 items), emotional function (7 items), physical symptoms (5 items), social support (2 items), sexual life (2 items), chronic disease management (1 item), perceived health status, and recognition of change of health status (1 item). Five-point Likert scale was used indicating higher score means better QoL. The tools used in this study showed high reliability (Cronbach's α=.90).
Hospital visiting days means the sum of the number of days for outpatient clinic visit, medication days and inpatient days. The medical expenditures are sum of the cost for inpatient services, outpatient services and medication. Those were calculated from the claims data for the year of 2007 and 2008 which was published by the Korea NHIC.
The study used SAS/WIN version 9.1 to analyze the data collected. Descriptive statistical methodology (frequency, percentage, and standard deviation) was utilized to describe the characteristics of study subjects. In order to compare the before and after difference, χ2 tests, and paired t-test were used.
The socio-demographic characteristics of study subjects are indicated in Table 1. There were 919 female and 445 male clients among study subjects, and a high percentage of subjects (60.6%) in the sample were 65 and over in age. Most of clients came under bereavement (56.6%) in marital status, no education (43.6%) in educational background and living alone (50.5%) in generation.
The degree of limitation in access to medical services, caused by The Copayment System, was measured. Results show that there is an overwhelmingly large percentage of not limited at all (21.8%) and not limited (58.6%), followed by limited, uncertain and very limited (10.1%, 9.0%, and 0.6%, respectively) among the entire clients. According to their responses, health care accessibility to medical services was not negatively affected by The Copayment System.
In Table 2, data from '07 and'08 were analyzed to compare changes in health behavior of The Copayment System clients. Compared to 2007, when The Copayment System had not yet been introduced, the health behavior of subjects increased positively after applying Copayments: flu prevention (p<.001), health care examinations (p=.035), and cancer examinations (p=.002).
There was no significant effect in medication adherence (p=.94) because the average value in '07 and'08 indicated 3.8 and 3.8 respectively (Table 3).
There was no significant effect in quality of life (p=.25) after implementing The Copayment System because the average value from '07 and'08 indicated 2.9 and 2.9 respectively in Table 4.
There was a significant change in hospital visiting days per capita, after implementing The Copayment System (Table 5). That is, hospital visiting days decreased by 8.5% compared to'07 (p<.001). There was no significant effect on medical expenditure. Instead, the amount of medical expenditure increased by 2.6%. Hospital visiting days and medical expenditure are categorized into 3 sections: Outpatient, in-patient and pharmacy. Outpatient days and medical cost decreased by 12.8%(p<.001) and 8.2% (p<.001) respectively, which indicates there was a significant difference between 07' and 08'. However, there was no significant effect of in-patient. Instead, in-patient days and cost increased by 8.7% (p=.400) and 11.6%(p=.336) respectively. Pharmacy days significantly decreased by 7.9%(p<.001), but pharmacy cost increased by 5.9%(p<.001).
This study sought to find the effect of Copayments on health and medical use of Medical Aid Beneficiaries. Above all, one question was asked to measure the degree of subjective limit of medical use by the study subjects. For this question, only 10.7% answered to 'Limited' and 'Very Limited', which demonstrated that the effect of Copayments was not significant.
According to existing documents, The Copayment System has had negative effects on preventive behavior because patients consider preventive services less important than medical care services. However, The Copayment System did not impact emergency room use due to acute myocardial infarction or serious diseases [14]. As a result of reviewing 300,000 cases for 65 to 69 aged women among 174 data for Medicare managedcare plans, when Copayment clients paid 10% of medical cost, the frequency of mammography use decreased by 8.3%. The above data demonstrates that a more cautious approach would be needed, if Copayments was applied in the preventive medical services such as mammography[6]. However, in this study, there was a significant increase in using preventive services including health examination, cancer examination and vaccination for influenza. That is, Copayments did not greatly influence health behavior.
It is assumed that these results come from Korea's medical service system. In Korea, senior citizens of low-income family are offered health examination services for free and also offered cancer examination or vaccination for influenza for free or with a low cost. Like this, Medical Aid Beneficiaries can be offered preventive services, though they have difficulties using medical institutions due to Copayments.
It is known that Copayments influences medication behavior. Generally, it is expected that medication adherence is getting higher because patients try to reduce medical costs and doctors also try to reduce patients' burden. In reality, however, it rarely happens[6]. Instead, medication adherence decreases according to the study on the effect of Copayments on diabetes medicines by Gibson[7]. In addition, the study where registrants of health insurance, covered by corporations, were analyzed on more than 20 million cases, demonstrated that medication adherence would be lowered by 5.4, when medical costs of patients increased by 10 dollars. Certainly, some study concludes that medication adherence is impacted by existing characteristics of medication, rather than simply by Copayments.
One of leading studies on the effects of Copayments is the Rand study, whose topic was about whether Copayments could reduce overuse of medical service users, studied by random allocation for 5 years[15]. RAND research demonstrated that the higher level of one's partial medical costs reduced medical service use of Copayment clients, which included medical services necessary as well as unnecessary to patients. In particular, Copayments brought out different effects on recipients, based on the economic level and health of the subjects.
Recipients, who were healthy with more than a certain amount of income, were not influenced by Copayments. However, those recipients who were poor and suffering from chronic diseases appeared to use less medical services, which influenced their health. For instance, when low-income patients suffering from severe high blood pressure were supposed to pay the partial medical costs of Copayments, their mortality rate increased by 14%. That is, the effects of Copayments on the health of patients varied, based on socio-economic characteristics or their susceptibility to chronic diseases, or disease severity[16,17].
This study demonstrates that there is no change of medication adherence due to Copayments. It is possibly assumed that medical costs paid by Medical Aid Beneficiaries were so small, which did not impact medication adherence. Additionally, this study did not have time enough to see the effects of Copayments because it was done one year after the introduction of Copayments.
There was no significant effect of Copayments on quality of life in this study. The results and data from this study concluded that partial medical costs of Korea's Copayments were not significant enough to impact the health of patients. In particular, patients with severe diseases had alternatives, including inpatient services. Therefore, the health of recipients was not influenced directly by Copayments.
In the present study, the total days of medical visitation declined significantly one year after the implementation of Copayments. In particular, outpatient visitation days and medical expenditures decreased significantly. Additionally, pharmacy visitation reduced. However, contradictory to the reduction of pharmacy visitation days, the total pharmacy costs increased, which shows similar results to the above. That is, medical expenditures for medical services increased, which did not impact the total amount of medical expenditures[18,19]. However, some studies demonstrate that Copayments influence medical serviceuse[20].
In this study, the reason that pharmacy visitation days reduced was related to outpatient visitation in almost all cases. However, pharmacy costs increased. That is, outpatient visitation to medical institutions, unnecessary to patients, declined, but pharmacy costs increased, which means that actual quantity of medication increased.
It is known that Copayments influenced medication and that a 10% Copayment increases reduced medication by 2 to 6%[21]. Unlike the existing results, this study demonstrated that the reason why Copayments did not reduce pharmacy costs was that Copayments did impact patients' visitation behavior to medical institutions, but did not impact doctors and actual medical suppliers.
A phenomenon of not being able to control medical suppliers was also applied in the increase of inpatient visitation. As a result of this study, inpatient visitation days and costs increased significantly, this played a major factor in the increase of all medical expenditures. Certainly, the study results come from a primary purpose of Copayments to suppress outpatient visitation as well as the fact that the previous policy of free medical costs for inpatient remained. Despite this fact, a rapid increase of inpatient days and costs demonstrates that patients with minor illness had possibilities to avoid limitation of Copayments for outpatient services and then overused inpatient services due to free medical costs for inpatient and reflected controlling suppliers was in need in the procedure of deciding inpatient services for patients[22,23].
As the Ministry of Health and Welfare has been operating copayments since July 1, 2007 and also set up Qualification Management System for Medical Aid. By doing so, the ministry could be offered real-time data for Medical Aid days from Medical Aid institutions to manage Medical Aid Days. However, any national system to prevent excessive and repeated treatment by medical institutions is not prepared yet.
There was a limitation in that the study did not have control groups, because the entire group of beneficiaries was the study subjects. In addition, when it comes to selecting variables to measure the effect of The Copayment System, a systematic approach was not applied and several variables were randomly chosen based on existing data. There was also a limitation in that the study used combined existing questions to measure when there were not enough measuring tools.
In the future, various measures should be implemented, such as strengthening counseling, education, linking services between health and welfare, alternative services for community in order to induce patients to use medical services properly, rather than raising the awareness of medical expenditures[2]. In addition, persistent research for health afterward and various measures for recipients and suppliers management should be put into action to ensure Copayments pursue the effect of saving Medical Aid costs effectively.
The study is to define the differences in health care utilization and expenditure for Type I Medical Aid Beneficiaries before and after applying Copayments. In conclusion, Copayments does not seem to be a great influencing factor in accessibility to medical service, medication adherence and QoL of beneficiary subjects even though it have suppressive effect of health care cost was limited. This study needs persistent research afterward because of limited data of just two years after applying Copayments.
Figures and Tables
Table 1
Individual Characteristics of Client Characteristics of the Study Population (N=1,364)

Table 2
Health Behavior of Copayment Client (N=1,364)
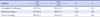
| Variables | 2007 | 2008 | χ2 | p |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Vaccination for influenza | 815 (60.4) | 872 (64.6) | 15.25 | <.001 |
| Health examination | 587 (43.9) | 688 (51.1) | 4.44 | .035 |
| Cancer screening | 483 (36.3) | 544 (40.9) | 10.02 | .002 |
Table 3
Medication Adherence of Copayment Client (N=1,364)

Table 4
Quality of Life in Copayment Client (N=1,364)

Table 5
The Change of Hospital Visiting Days and Medical Expenditure per Capita in Copayment Client (N=1,364)

References
1. Ministry Health and Welfare. Introduction for medical aid program in 2010. Seoul: Ministry Health and Welfare;2009. p. 401.
2. Kim US, Nam JJ, Kim MY, Goh IS, Lee DM, Choi JS, et al. Long-term medical service use status of medical aid beneficiaries and its improvements (2007-12). Seoul: Ministry of Health and Welfare;2007. p. 399.
3. Lee YJ. A study of the factors and the regional difference of medical Aid Program recipient's medical utilization. Soc Welf Policy. 2007; 28:233–251.
4. Kephart G, Skedgel C, Sketris I, Grootendorst P, Hoar J. Effect of copayments on drug use in the presence of annual payment limits. Am J Manag Care. 2007; 13(6):328–334.
5. Kim JY, Ko SK, Yang BM. The effects of patient cost sharing on ambulatory utilization in South Korea. Health Policy. 2005; 72(3):293–300.

6. Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in medicare health plans. N Engl J Med. 2008; 358(4):375–383. DOI: 10.1056/NEJMsa070929.

7. Gibson TB, Song X, Alemayehu B, Wang SS, Waddell JL, Bouchard JR, et al. Cost sharing, adherence, and health outcomes in patients with diabetes. Am J Manag Care. 2010; 16(8):589–600.
8. Oh JJ, Choi JM, Yu WS. Job analysis and methods for enhancing efficiency of medical aid client managers. Seoul: Ministry of Health, Welfare and Family Affairs, Dankook University;2008. p. 199.
9. Shin YE, Shin HC, Shin HW, Park EJ, Hong SW, Shin SM, et al. Study on the health status and hospital service utilization of Korea medicaid clients. Seoul: Korea Human Resource Development Institute for Health and Welfare;2007. p. 430.
10. Kang EJ, Choi EJ. 2005 the third Korea national health and nutrition examination survey: Health behaviors of adults. Seoul: Korean Institute for Health and Social Affairs;2006. p. 272.
11. Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med. 1984; 100(2):258–268. DOI: 10.7326/0003-4819-100-2-258.

12. Morisky DE, Levine DM, Greene LW, Shapiro S, Russell RP, Smith CR. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983; 73(2):153–162.

13. Jun FW, So KJ, Kim AY, Kim HG, Kim CW, Lee YM, et al. Case management society of America 'case management adherence guidelines 2.0'. Seoul: Hyunmoonsa;2007. p. 937.
14. Magid DJ, Koepsell TD, Every NR, Martin JS, Siscovick DS, Wagner EH, et al. Absence of association between Insurance copayments and delays in seeking emergency care among patients with myocardial infarction. N Engl J Med. 1997; 336(24):1722–1729. DOI: 10.1056/NEJM199706123362406.

15. Dranove D. The economic evolution of American health care. New Jersey, NJ: Princeton University Press;2000. p. 224.
16. Gruber J. The role of consumer copayment for health care: Lessons from RAND health insurance experiment and beyond. Washington DC: The Henry J. Kaiser Family Foundation;2006. p. 15.
17. Wong MD, Andersen R, Sherboume CD, Hays RD, Shapiro MF. Effects of cost sharing on care seeking and health status: Results from the medical outcomes study. Am J Public Health. 2001; 91(11):1889–1894.

18. Cole JA, Norman H, Weatherby LB, Walker AM. Drug copayment and adherence in chronic heart failure: Effect on cost and outcomes. Pharmacotherapy. 2006; 26(8):1157–1164. DOI: 10.1592/phco.26.8.1157.

19. Wallace NT, McConnell KJ, Gallia CA, Smith JA. How effective are copayments in reducing expenditures for low-income adult medicaid beneficiaries?experience from the oregon health plan. Health Serv Res. 2008; 43(2):515–530. DOI: 10.1111/j.1475-6773.2007.00824.x.
20. Hartung DM, Carlson MJ, Kraemer DF, Haxby DG, Ketchum KL, Greenlick MR. Impact of a medicaid copayment policy on prescription drug and health services utilization in a fee-forservice medicaid population. Med Care. 2008; 46(6):565–572. DOI: 10.1097/MLR.0b013e3181734a77.

21. Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: Associations with medication and medical utilization and spending and health. JAMA. 2007; 298(1):61–69. DOI: 10.1001/jama.298.1.61.
22. Yang JH. The evaluation on the effect of outpatient visit copayment policy for medicaid in Korea [dissertation]. Seoul: Korea University;2010. 120.
23. Hong SW. The effects of copayments on healthcare utilization in the type I medicaid beneficiaries [dissertation]. Seoul: Seoul National University;2009. 103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download