Abstract
Purpose
The purpose of this study was to evaluate the effectiveness of case management for patients with hypertension on their health status and medical service utilization.
Methods
This study was a secondary analysis of data collected for a larger study of chronic disease management in 2008 using the National Health Insurance Corporation database. A total of 12,944 patients who received case management for hypertension were included in this analysis. The subjects of case management were classified into subgroups, namely, over-use, under-use, and non-use groups according to the amount of medical service utilization. To compare the medical service utilization, a control group was selected randomly. The data were analyzed through descriptive statistics, McNemar test, and ANOVA.
Results
All the subgroups displayed significant differences in blood pressure, self-management, social support, and their characteristics of medical service utilization. The total medical expense of the under-use and non-use groups increased after case management. However, there was no decrease in the medical expense of the over-use group.
Mortality rate and medical expense caused by cardiovascular disease (CVD) have been increased[1]. Therefore, constant efforts with close attention, have been made to manage hypertension (HT) which is one of the major risk factors of CVD[2]. In Koreans over the age of 30, the awareness rate and treatment rate of HT were 66.0% and 61.1%, the control rate of blood pressure (BP) being 42.9%[3], lower than those of other countries such as England, USA, and Canada[4]. Also, even though a variety of policies and projects are being carried out to manage HT, the medical expense of this disease is continuously rising, about 630 billion won being spent in 2012[5], 13% of the year's total medical expense was spent to treat HT and its complications, particularly CVD, in Korea.
Case management (CM) refers to a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual's and family's comprehensive health needs through communication and available resources to promote quality cost-effective outcomes[6]. CM affects the knowledge and psycho-social factors of patients like social support, resulting in self-care behaviors[7,8,9]. A patient's self-care behaviors and lifestyle are related to short-term outcomes including BP[7,8,9,10,11], which, in turn, affects the patient's long-term health (mortality) and medical service utilization[12,13].
National Health Insurance Corporation (NHIC) has been suffering constant financial difficulties due to the increase in medical expenses of health insurance, since institutional changes were made in 2000, such as medical insurance unification and separation of dispensary from medical practice[14]. One of the major causes is the rapid increase in chronic disease patients and another is the irrational use of medical services by health insurance subscribers, for example, people using more medical services than medical needs or not using medical services even though they need them for medical reasons[15]. To solve these problems, NHIC, with the help of its local branches nationwide, has been running a CM project in community focusing on the goal of improving health status of HT patients who over- or under-use medical services to prevent aggravation and complication of the chronic disease through promoting the health behaviors and encouraging rational medical service utilization[16].
Several studies have reported the positive effectiveness of CM on health behaviors and health status[10,17,18,19]. However, few studies has been conducted to evaluate the effects of CM on the medical expense and use of medical services, even some previous studies showing contradictory results[12,20]. Therefore, in order to evaluate how much impact CM has on its two main goals, health status and appropriate utilization of medical services should be assessed following the CM projects.
The purpose of this study is: (1) to identify the change, before and after the CM program, in clinical measures, self-management, social support, and patterns of medical service utilization in CM groups and (2) to compare the changes of CM group with those of the control group in medical expense and amount of medical service utilization.
The study conducted a secondary analysis on the data collected for a quality improvement project of chronic disease management in 2008. This study was a comparative study to compare the effects of CM for HT patients.
The subjects were chosen among the HT patients who received CM services from NHIC case managers from January 13, 2006 to December 28, 2007. From the total 13,164 patients, 12,944 patients were finally chosen excluding those who dropped out during the CM.
The subgroup of CM was classified according to the amount of medical service a patient used to treat HT during the previous 12 months: non-use, under-use, and over-use[16]. The over-use group was defined as the top 5% in medical expenses due to HT. To classify the under-use group, all the subjects were divided into 9 groups according to their annual hospital visit days and prescription days. Those recording 1~179 medication days and more than 16 visit days (group III), 180~239 medication days and 3~5 visit days (group IV), or 180~239 medication days and 6-15 visit days (group V) were included in the under-use group[16,21]. The criteria of under-use was developed based on clinician's professional opinion, and results of population[21]. More detailed information on developing process of the criteria of under-use can be found in Kim's report[21].
The non-use group was the ones who had not gotten the treatment for HT during the previous 12 months even after they were clearly diagnosed of HT in a NHIC check-up.
In order to analyze the medical expense and amount of medical service utilization, the study established two control groups. The control groups were created against each category, over-use, and under-use group, subjects randomly chosen from the people with the same gender, age, main disease, and monthly health insurance fees as each CM group. The statistician who did not involve the study selected the control group randomly using statistic program. In case of non-use group, there was no control group because they didn't spend expense for treatment of HT. Therefore, for comparison of non-use group, we used control group for under-use group as those of non-use group.
In this study, CM refers to a supportive service which a case manager provides, such as counseling, education, and information, for HT patients and their family in order to change the patterns of medical service utilization and health behaviors[16]. First, a list of potential subjects is retrieved from the NHIC database. The potential subjects were selected if they used the medical service for HT in the previous year, aged of 30~70 years and used medical service more or less than medical needs. A case manager contacts the subjects through phone or mail. If the subject agrees to receive CM services, they get registered in the CM database. After the enrollment, the case manager visits the subject's house to assess his/her needs. Based on the assessment result, the case manager makes a list of the subject's health problems and a CM plan for him/her. The case manager provides the subject with CM services in line with health problem and care plan through phone calls or home visits (Table 1). Through home visits, case manager provides direct service such as the education, counseling, and information. Through call visit, case manager monitored if they practice as their care plan. When the service is completed, the case manager evaluates the result with the subject through interviews and surveys. All the processes including needs assessment, problem selection, mediation, and evaluation related to the CM are conducted following the standard guideline[16]. More detailed information on the contents of case management can be found elsewhere[11, 16].
A case manager, the one who provides CM services, should complete a training program certified by the NHIC CM certification committee and possess a health-manager certificate (1st grade or 2nd grade)[16]. They are laymen who work at NHIC. 5% of them have a nursing licence and about 18% have a social worker license.
The results of CM service were evaluated by some questionnaires and the data about medical service utilization. The data of general characteristics, clinical measures, self-management, social support, and the characteristics of medical service utilization were directly surveyed before and after the CM program using needs assessment questionnaires developed by NHIC[16]. The study used the data about the medical service utilization of the CM and control group retrieved from the NHIC database.
The study examined the subjects' general characteristics such as gender, age, marriage status, education level, employment status, type of health insurance, and monthly insurance fees. Education level was classified as primary school diploma or less, middle school diploma, high school diploma, and college diploma or more. Type of health insurance was categorized into two groups, regional health insurance and employment-based insurance.
To collect information about the CM process, the study measured the duration of CM services and the number of visits.
The study measured systolic blood pressure (SBP), diastolic blood pressure (DBP), BP control rate, and BP awareness rate of the subjects. The subjects whose SBP was over 140 mmHg and DBP, over 90 mmHg were defined as their BP not being controlled[22].
Health behaviors such as knowledge of HT, smoking status, regular exercise, low-sodium diet, low-cholesterol diet were examined. The knowledge of HT was measured by six questions from which subjects got 0 to 1 points with their answers, yes, no, and don't know[23]. The total score ranges from 0 to 6, higher scores meaning more knowledge. The daily number of cigarettes they smoked during the previous 30 days. Also, they were asked how many times they work out in a week more than 30 minutes until they sweat or feel slightly out of breath. The answer more than 3 times per week was defined as having regular exercise. Concerning the low-sodium diet and the low-cholesterol diet, the subjects received 1 point when they never had, 2 points for keeping it for 1~2 days, 3 points for 3~4 days, 4 points for 5~6 days, and 5 points for more than a week[16,23].
Social support was assessed by one question whether family members help the patients control their BP, for example, with diet, exercise, and medication management. The question was answered by the answers, yes, no, no family members, and realistically not available. Assessing the use of local community resources, the subjects were asked whether they had participated in HT classes, HT patient and family gatherings, and other local community services after CM.
In regard to HT, the subjects completed a questionnaire asking whether they had an attending physician, whether they were satisfied with the communication with the doctor, whether there was therapeutic duplication in prescriptions, whether they visited an outpatient clinic less than twice to treat HT during the previous 6 months, and whether they used more than 3 medical institutions as an outpatient to treat the disease during the same period[16,24].
The study collected the data about the medical service utilization of the CM group and the control group for 6 months before the CM and for 6 months and 12 months after the CM from the NHIC database. The medical service utilization for other disease treatment as well as HT treatment were included. The study defines the amount of medical service utilization as a number converted into an annual amount of medical service utilization. The control group against the over-use group included 1,197 patients and its average age was 66.1±9.72. The under-use group's control group included 10,558 patients, with an average age of 66.2±9.73. Gender and monthly insurance fees were the same.
In order to conduct a study on a quality improvement project of chronic disease management in 2008, data were retrieved from the NHIC CM database. In advance of the CM, the subjects agreed the data collected during the CM program could be used for research or statistical analyses. Personal information about the subjects was provided in the form of unique numbers so as not to be identified following the NHIC internal regulation governing information provision.
The data collected were analyzed through the SPSS/WIN 15.0 program in 2008. The general characteristics of the CM subjects were analyzed by frequency, percentage, average, and standard deviation. The effects of CM in clinical measures, self-management, social support, and patterns of medical service utilization were analyzed through the McNemar and paired t-test. In addition, in order to compare the changes in the medical expense and amount of medical service utilization in the CM group with those of the control group, the study used the average change value of them during the 6 months and 12 months following the CM.
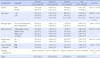
Table 1 presents the general characteristics of the overall subjects and also characteristics according to the CM subgroup. Of the overall subjects, 41.8% were over the age 65 and 59.3% were female. 82.2% were married, 35.8% had college diploma or more, and 44.4% were employed. The average monthly insurance fees were 51,130.3±54,259.38 won.
The subgroups showed a significant difference in general characteristics (p<.001). While there were more women in the over-use and under-use group, 57% and 62.6% each, the non-use group included more men (68.3%) than women. 58.25% were over the age 65 in the over-use group, but the proportion was smaller in the under-use and non-use group, recording 41.8% and 25.1%, respectively. Compared to the over-use group (21.4%), there were fewer non-married/separated subjects in the under-use group (17.5%) and in the non-use group (12.9%). In addition, the under-use (34.8%) and non-use (53.8%) group displayed a higher level of education, having college diploma or more, than the over-use group (26.8%). In terms of employment status, 66.4% of the over-use group had not a job, compared to the under-use group, 56.7%, and the non-use group, 33.7%. The non-use group showed a higher rate of employee health insurance and a lower monthly insurance fee than the over-use and under-use group (Table 2).
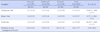
The subjects received 4.2 times of CM service for 9.8±4.77 weeks, in average. The total number of CM visit of the under-use group was 4.2±0.53, significantly less than that of the under-use and non-use group (p<.001)(Table 3).
After the CM, the SBP and DBP of the overall CM group changed by -7.7±14.42 mmHg and -3.8±9.67 mmHg, showing a significant decrease (p<.01). In particular, the non-use group showed the most decrease (SBP difference -14.9 mmHg, DBP difference -7.7 mmHg), the under-use and over-use group also displaying a statistically significant decrease in BP (p<.01). The control rate of BP showed a significant increase by 26.1% in the overall CM group, among which the non-use group showed the most change, 39.0%, followed by the under-use group, 24.6%, and the over-use group, 23.5% (p<.01).The awareness rate of BP also significantly rose by 6.5%, particularly in the non-use group (12.1%, p < .01)(Table 4).
Self-management showed a significant improvement among overall CM group after the CM. The subjects' knowledge of HT increased (by 1.8 points), particularly in the non-use group. In addition, almost every variable in the self-management category displayed a significant improvement; a decrease in rate of smoking (1.3%) and in the amount of smoking (2.7 cigarettes/month) and an increase in the rate of regular exercise (17.0%), and in the number of eating low-sodium diet (20.8%) and low-cholesterol diet (19.8%)(p<.01). The changes were most prominent in the non-use group. As of social support, the help of family members increased by 4.1~5.3% and the education and support utilizing local community resources also increased by 3.0~7.4%(Table 4).
The rate of patients having an attending physician increased by 5.4% after the CM (p<.01), particularly the non-use group showing the most growth. Also, the satisfaction with the communication with the attending physician rose by 5.4%, in average, the over-use group and the non-use group recording a 6.0% and 6.5% increase, respectively (p<.01). The rate of duplicate prescriptions concerning HT fell by 0.6% among the overall subjects, a significant decrease. The rate decreased by 0.8% in the over-use group and 0.6% in the under-use group.
The rate of visiting outpatient clinics twice or less in six months decreased by 2.1% in the overall CM group. The biggest decrease was observed in the non-use group (9.9%). While the rate of visiting more than 3 hospitals to treat HT fell by a mere 0.4% in the overall group, the decrease in the over-use and under-use group was significant (Table 4).
The changes in medical expense over the 6 months and 12 months after the CM were converted into annual figures, setting the amount of the 6 months previous to the project as the criteria. The figures are presented as Table 5. In terms of inpatient medical service utilization, the under-use and non-use group, compared to their under-use control group, showed an increase in the rate and days of admission, the days of treatment during admission, and medical expense for admission, 6 months and 12 months after the CM. The over-use group, compared to the control group, showed a decrease in the rate of admission when 6 months past after the CM, slightly reducing the medical expense for admission. However, the trend weakened after 12 months, with a large increase in the number of days of admission and treatment during admission, resulting in an annual increase of 1,424,174 won in the medical expense for admission.
As of outpatients, aspects, such as the rate and days of outpatient visits, the days of medication in outpatient, and the medical expense for outpatient, slightly increased in the under-use group 6 months after the CM, compared to the control group, but after 12 months, the numbers went down. Likewise, the non-use group experienced a rise in the rate and days of outpatient visit, the days of medication in outpatient, and the medical expense for outpatient 6 months after the intervention, yet after 12 months the figures fell. Compared to its control group, the over-use group, after the CM, showed an increase in the rate of outpatient visit, yet a decrease in the number of days of outpatient visit, the days of medication in outpatient, and the medical expense for outpatient.
The increase in the total medical expense of the under-use and non-use group was less than that of the control group, 6 months and 12 months after the CM. Nevertheless, while the over-use group's total medical expense decreased 6 months after the CM, compared to its control group, after 12 months, the total medical expense exceeded its control group.
This study examined the effects of CM medical service utilization as well as health status. As a result, in all CM subgroups, there was a significant improvement in clinical measures, self-management, social support, characteristics of medical service utilization. However, in the follow-up survey on the medical expense and amount of medical service utilization 12 months after the CM, while the medical service utilization of the under-use and non-use group improved, the over-use group's utilization of outpatient clinics merely shifted to hospitalization. Also, the over-use group's medical service utilization reduced until 6 months after the CM but returned to the state of excessive utilization later on.
As a result of the evaluation of clinical measures after the 10-week CM, all CM subgroups experienced an improved BP level and control rate of BP. In particular, the most decrease occurred in the non-use group, with 14.9 mmHg of SBP and 7.7 mmHg of DBP, in average. This study's result accords with the existing research suggesting CM positively affects BP control[8,9,10]. A project in which public health nurses provided CM services to seniors for 3 months also achieved a significant outcome in reducing BP[9]. In addition, as a result of interactive patient education sessions provided by nurses, the subjects' BP decreased significantly at 12 months of follow-up management[8]. In Korea, a health care project of customized home visiting applying CM methods to uncontrolled HT patients produced 64% of increase in the control rate of BP[10]. This indicates CM have been known to encourage health behaviors and self-management[25,26] had a positive impact on BP control as well as self-management behaviors.
As a result of a survey, carried out right after the CM program, questioning the changes in the characteristics of medical service utilization, the subjects in the under-use group and the non-use group replied they now had an attending physician for their main disease and their satisfaction with the doctor-patient communication increased. Compared to the control group, even though the days of admission and outpatient visit to treat HT increased in the under-use group and the non-use group 6 months after the CM, the amount tended to decrease 12 months after CM.
Due to the insufficiency of existing research, there is a need to be discreet when interpreting the effects of CM on the under-use group and the non-use group. The change in medical service utilization shown in the non-use group is similar to the result of an existing study suggesting that a HT check-up program for seniors was effective in reducing medical expense in the long-term [27]. Also, this study's findings make a partial accordance with a study result that there was a decline in outpatient medical service utilization, despite there being no change in the amount of hospitalization[7] and also with another research result that HT management had a positive impact in reducing medication expense[20]. Therefore, an increase of medical expense among under- or non-user in this study will expect to prevent unnecessary expense spending in the long run.
The change in the medical expense among the non-use group and the under-use group may be due to their socioeconomic status. The non-use group and the under-use group were relatively young, employed, and had a high level of education. Thus, the result is considered to be an effect of education through CM. According to Williams and Wold[28], low social status leads to a lack of self-management knowledge and, in turn, leading to poor health status and an increased expense for treating preventable diseases. Therefore, CM will have a positive effect on reducing medical expense providing CM service to people who had not been receiving HT treatment due to their lack of knowledge with information about HT treatment and self-management in community.
The over-use group replied their duplicate prescriptions of HT medicine declined and the rate of visiting more than three hospitals for HT treatment also decreased after the CM. However, when comparing the medical expenses before and after the CM against those of the control group, even though the over-use group showed a decrease in hospital admission and outpatient visits 6 months after the CM, after 12 months, the increase in the days of admission and treatment during admission resulted in an overall rise of medical expense in spite of the reduced number of outpatient clinic visit. In other words, the over-use group's utilization of outpatient department merely shifted to hospitalization, leading to no eventual change. Applying health improvement programs to the over-use group had no impact in reducing the use of clinics by HT patients[12]. Additionally, as shown in a study that the provision of CM services for excessive medical care users didn't reduce the out-of-pocket money and the overall medical expense after using the designated doctor system[29], a short-term CM service for medical service over-users is considered ineffective in eventually cutting back medical service utilization. In Korea, because hospitalization is decided not only by doctor but also patients and family, it is not easy to control the total medical expense and amount of medical service utilization by case management. Therefore, it will be needed to cooperate with doctor who treated patient's disease in case management for over-user. Yet, since there are insufficient studies about the application of CM to medical service overusers, the results should be reaffirmed through repetitive studies.
Considering the result of a precedent study that a follow-up survey after a short-term CM program discovered that the lowered BP thanks to the program didn't last long[11], there is a need for continuous management of the over-use group after the CM program is completed. In this study, the subjects in the over-use group were mostly female, living alone, old, with low level of education and jobless. Going along with the finding that among the subscribers of health insurances, those with low level of income and education showed higher medical service utilization[30], this socio-economically vulnerable group has a possibility of using more medical services as they are more likely to miss the right time for treatment or to aggravate the disease due to various obstacles. Hence, in case of the vulnerable, there is a need for early intervention for disease management to prevent the over-use of medical service. Considering the fact that appropriate utilization of medical service is an outcome achieved through collaboration of patients, family members, and medical staff for the patient's satisfaction of personal requests and his/her best health status as well as sufficient knowledge and understanding of resources[6], the cause of excessive use of medical services observed in the over-use group should be analyzed in-depth, complementing the contents of CM.
The study has several limitations. First, since the study was not based on a rigorous research design, other factors else than CM could have influenced the subjects' medical service utilization. Second, even though it is expected that the under-use group and the non-use group received direct and indirect HT treatment, increasing the compliance and accuracy of medication and contributing to BP control and medical expense reduction, the direct causal relationship is unable to be confirmed through this study. Thirdly, in case of data of medical service, we received not the raw data but the data processing which couldn't identify the individual patients, so we didn't test the difference of medical service utilization statistically. Fourth, the criteria of appropriate use of medical service utilization is not presented and defined. Therefore, objective criteria to decided whether the subject use medical service appropriately or not should be developed. Finally, the subject in this study have other disease as well as HT. We didn't control medical service utilization for treatment of other disease. Treatment for other disease may have influenced medical expense and the amount of medical service utilization during study periods.
Recently, the excessive use of medical service and the increase in the medical expense for chronic diseases are a serious issue. The CM approach based on local communities is an effective way to help HT patients control their BP from close range. In this study, we discovered providing CM for those who under-used medical service was effective. However, for the subjects who over-used medical service, the CM encouraging appropriate medical service utilization was ineffective. Therefore, the cause of excessive medical use should be reexamined, supplementing and revising the specific strategies for appropriate medical service utilization. Since the socially vulnerable are more likely to over-use medical services, early intervention for disease control is required to prevent over-use.
Figures and Tables
References
1. Grover SA, Coupal L, Kaouache M, Lowensteyn I. Preventing cardiovascular disease among Canadian: What are the potential benefits of treating hypertension or dyslipidemia? Can J Cardiol. 2007; 23(6):467–473.
2. Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: The Suita study. Hypertension. 2008; 52(4):652–659. http://dx.doi.org/10.1161/HYPERTENSIONAHA.108.118273.
3. Korea Centers for Disease Control and Prevention. Report No.: 11-135 1159-000027-10. National health statistics in 2011: Fifth 2nd year national health and nutrition examination (2011). Seoul: Ministry of Health and Welfare;2012.
4. Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: A cross-sectional study. BMJ Open. 2013; 3(8):e003423. http://dx.doi.org/10.1136/bmjopen-2013-003423.

5. National Health Insurance Corporation. Report No.: 11-B550928-000001-10. 2012 national health insurance statistical yearbook. Seoul: National Health Insurance Service and Health Insurance Review & Assessment Service;2013.
6. Yamamoto L, Lucey C. Case management "Within the Walls": A glimpse into the future. Crit Care Nurs Q. 2005; 28(2):162–178.
7. Kim YM, Shin EY, Lee KS. Effects of the case management program for the elderly with hypertension. J Korea Gerontol Soc. 2006; 26(3):477–492.
8. Patton K, Meyers J, Lewis BE. Enhancement of compliance among patients with hypertension. Am J Manag Care. 1997; 3(11):1693–1698.
9. Yim ES. Cost-benefit analysis of the case management for the elderly patients with hypertension [dissertation]. Seoul: Yonsei University;2009. p. 149.
10. Lu KY, Lin PL, Tzeng LC, Huang KY, Chang LC. Effectiveness of case management for community elderly with hypertension, diabetes mellitus, and hypercholesterolemia in Taiwan: A record review. Int J Nurs Stud. 2006; 43(8):1001–1010. http://dx.doi.org/10.1016/j.ijnurstu.2005.11.013.

11. So AY, Kim YM, Kim EY, Kim CY, Kim CH, Kim HG, et al. Effects of community-based case management program for clients with hypertension. J Korean Acad Nurs. 2008; 38(6):822–830. http://dx.doi.org/10.4040/jkan.2008.38.6.822.

12. Dally DL, Dahar W, Scott A, Roblin D, Khoury AT. The impact of a health education program targeting patients with high visit rates in a managed care organization. Am J Health Promot. 2002; 17(2):101–111.

13. Skaer TL, Sclar DA, Markowski DJ, Won JK. Effect of value-added utilities on prescription refill compliance and health care expenditures for hypertension. J Hum Hypertens. 1993; 7(5):515–518.
14. Yoo SH, Moon SH. Evaluating performance of finance stabilizing program for national health insurance. Korean Policy Stud Rev. 2006; 15(3):241–271.
15. Lee BY. The points and improvement plan of case management project of national health insurance corporation - centering on program of human resource development, education and training [master's thesis]. Deajeon: Daejeon University;2007. 106.
16. National Health Insurance Corporation. Job manual for proper utilization of medical care. Seoul: National Health Insurance Corporation;2007.
17. Korean Society of Hypertension. 2013 Hypertension treatment guidelines of the Korean society of hypertension. Committee on Establishment of Treatment Guidelines. Seoul: Korean Society of Hypertension;2013.
18. Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, et al. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996; 9(4 Pt 1):285–292.

19. Whelton PK, Appel LJ, Espeland MA, Appleqate WB, Ettinger WH, Kostis JB, et al. Tone collaborative research group. Sodium reduction and weight loss in the treatment of hypertension in older persons: A randomized controlled trial of nonpharmacologic interventions in the elderly(TONE). JAMA. 1998; 279(11):839–846.
20. Ginsberg GM, Viskoper JR, Fuchs Z, Drexler I, Lubin F, Berlin S, et al. Partial cost-benefit analysis of two different modes of nonpharmacological control of hypertension in the community. J Hum Hypertens. 1993; 7(6):593–597.
21. Kim CY, Kim YM, Kim EY, Kim CH, Kim HS, Kim HG, et al. Study on the application and expansion of pilot project of case management. Seoul: National Health Insurance Corporation;2004.
22. Drevenhorn E, Kjellgren KI, Bengtson A. Outcomes following a programme for lifestyle changes with people with hypertension. J Clin Nurs. 2007; 16(7B):144–151.

23. Choi IH. Changes of blood pressure and the performance of self-management of hypertension patients following the case-management [master's thesis]. Busan: Kosin University;2007. 19.
24. Lee WW. A study on the medical service use of high blood pressure patients through the case management program and on the effect of their self-management performing level [master's thesis]. Gyeongsan: Yeungnam University;2007. 73.
25. Ko IS, Kim CJ, Lee TW, Lee KJ, Kim ES, Ma HY, et al. Evaluation of government assisted visiting nursing services of health center in 2000. J Korean Acad Nurs. 2002; 32(3):344–354.

26. Yu SJ, Song MS, Lee YJ. The effects of self-efficacy promotion and education program on self-efficacy, self-care behavior, and blood pressure for elderly hypertensives. J Korean Acad Adult Nurs. 2001; 13(1):108–122.
27. Deng BH, Lui HW, Pan PC, Mau LW, Chiu HC. Cost-effectiveness of elderly health examination program: The example of hypertension screening. Kaohsiung J Med Sci. 2007; 23(1):17–24.

28. Williams A, Wold J. Nurses, cholesterol, and small work sites: Innovative community intervention comparisons. Fam Community Health. 2000; 23(3):59–75.

29. Lim SJ. The effects of case management for medicaid on healthcare utilization by the medicaid system. J Korean Acad Community Health Nurs. 2010; 21(4):375–385.

30. Lee HJ, Lee TJ, Jeon BY, Jung YI. Factors related to health care utilization in the poor and the general population. Korean J Health Econ Policy. 2009; 15(1):79–106.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download