Abstract
Purpose
The purpose of this study was to identify the construct equivalence of the general five factors of health behavior and to compare the latent means between adolescents with a health problem and those without in Korea.
Methods
The 2009 KYRBS (Korean Youth Risk Behavior Survey) data were used for the analysis. Multi-group confirmatory factor analysis was performed to test whether the scale had configural, metric, and scalar invariances across the existence of health problems in adolescents.
Adolescence is a critical period that determines health habits, and the lifestyle of an individual in this period comes to have significant effects on health in adulthood. Because health behavior becomes a long-term habit, picking up good health habits in adolescence can reduce the possibility of one having a disease in adulthood. However, most people believe that they are healthy during adolescence and sometimes act in a way that does harm to their health (McGuiness & Ahern, 2009). For this reason, adolescents have recently become the target group for health improvement in consideration of the fact that adolescence is a critical period that determines life-long health. To monitor health-threatening behavior in adolescence, Korea has built an Korea Youth Risk Behavior Web-based Survey system [KYRBS] to conduct research on a yearly basis since 2005 (Korean Centers for Disease Control and Prevention [KCDC], 2013a).
Most chronic diseases called lifestyle diseases are caused by complex factors; it is hard to discover their exact causes and see complete recovery from them with the current medical technology, which makes it difficult to make an effective therapeutic approach to them after they have developed. Although their exact causes haven't been discovered, they are caused by changes in lifestyles, such as over-nutrition due to economic growth and lack of exercise due to living automation; for this reason, they are also called lifestyle diseases. These problems are closely related to smoking, drinking, exercise, and diet, have a long latency period mostly with no special subjective symptoms, appear in childhood and develop slowly, and are caused by a mix of several factors (Ko, 2006). Smoking and drinking affect particular groups of lung and liver diseases, respectively (Jung & Kum, 2002; Kim & Lee, 2011), and exercise and diet affect one's general health status rather than specific diseases. It is reported that steady and regular exercise, regular meals, and vegetable diets prevent the outbreak of hypertension, diabetes, heart diseases, cancer, and so on (Ko, 2006).
Adolescence is generally regarded as a healthy period. Thus, research on health in adolescence scarcely deals with health problems or diseases but are mostly focused on health-threatening behavior, such as smoking and drinking (Kim, 2006; Ko et al., 2006; Lee, 2008), suicidal ideation (Kim & Kim, 2008), internet addiction (Park, Kim, Han & Kim, 2012), and so on (Park & Lee, 2002).
While it is necessary to take interest in healthful lifestyles as well as in health-threatening behavior in adolescence, KYRBS in 2010 reported that health behavior, such as exercise, decreased gradually on a yearly basis (Ministry of Education Science and Technology, Ministry of Health and Welfare & KCDC, 2012), while a survey in 2012 showed that the rates of smoking and drinking among secondary school students decreased down to 9.7% and 16.3%, respectively, but that the rates of students drinking soft drink and eating junk food three times a week or more often increased up to 25.5% and 13.1%, respectively, compared with figures from the 2011 survey (KCDC, 2013b).
The outbreak of lifestyle diseases in children and adolescence is actually on the rise. The data on the number of patients who are elementary or secondary school students with an adult disease and the actual medical expenses reported by the Health Insurance Review and Assessment Service (2013) showed that a yearly average of about 47,000 adolescents suffered from an adult disease: 48,392 in 2009, 46,758 in 2010, 45,557 in 2011, 45,346 in 2012, and 23,549 in the first half of 2013. Jang and Choi (2010), who analyzed the results of the National Nutrition Survey in 2007, indicated that adolescents aged 10 years or older showed prevalence rates of 0.3% for diabetes, 0.3% for hypertension, 3.5% for hypertriglyceridemia, and 8.8% for paranasal sinusitis. The National Health and Nutrition Survey indicated that asthma increased from 2.3% to 3.0% and the increase was particularly remarkable among infants and adolescents between 2005 and 2008. The prevalence rate of atopic dermatitis was higher in children and adolescence than in other age groups. It is essential to create positive management to prevent allergic health problems in their early stages because they are connected with each other and appear in a sequential way (allergic march). An allergic disease, which is not properly treated in children and adolescence, can be transferred into adulthood as a severe disease (KCDC, 2010). Despite the facts that children with a chronic kidney disease need strict dietary restrictions and changes in lifestyle and that complications, such as cardiovascular health problems, changes in nutrient metabolism, neurological disorders, and mental problems, are all related to the quality of living, research on children with a chronic kidney disease scarcely examined the quality of living in relation to health but focused on the therapeutic aspect (Jeon, 2011). This result demonstrates that there are adolescents already suffering from a disease, though at a lower rate than the healthy group, and that lifestyle health problems tend to be on the increase.
Even healthy adolescents may have good health behavior exert significant influence on life-long health. It is essential for adolescents suffering from a health problem to maintain the necessary habits to recover health and prevent the disease from developing since they are exposed to the disease earlier than others. It is necessary to create an environment that allow vulnerable adolescents exposed to health problems to establish good health habits so that they maintain a healthy status among most healthy adolescents until they reach adulthood. For general lifestyle diseases, good daily control is a prerequisite for preventing complications and maintaining a healthy life rather than trying to heal them completely. Since health problems that appear at young ages persist through life and have a longer duration than those that appear in adulthood, they require significant control in living; however, it is uncertain whether students with a disease can exhibit more desirable health behavior than healthy ones in consideration of the developmental characteristics of adolescents and their socio-environmental situations.
It is believed that students with a disease need to maintain more desirable health behavior than healthy ones by changing their lifestyle to recover their health and prevent a disease from developing. If they don't, further research needs to reveal the causes and a plan has to be made for providing a manageable environment that allows unhealthy adolescents to perform their tasks and recover and maintain their health.
On the basis of the data from the 2009 KYRBS, this study aims to make a latent mean analysis to see if health behavior differs between students with a health problems and those with no health problems.
To do this, the following questions were developed: Do constructs of the health behavior differ between students with a health problem and those with no health problem when measurement errors are controlled?
This study is a secondary data analysis of 2009 KYRBS survey, consisting of data collected from a nationally representative sample of adolescents.
This study was conducted by using the raw data from the 2009 KYRBS (Approval Number 11758). The survey was conducted web-based on line on an anonymous basis through a self-administered questionnaire, with the data from a total of 75,066 respondents analyzed. Of them, 31,319 had a health problem and 43,747 had no health problem. Respondents having a disease marked one or more of the presented options such as atopic dermatitis, rhinitis, asthma, gastritis and enteritis, heart disease, cancer, and diabetes or other health problems and if the disease was not on the list, respondents wrote the name of the disease.
This study was conducted by using the raw data from the 2009 KYRBS. It is comprised of 92 indexes in 14 areas: drinking, smoking, obesity and weight control, physical activities, eating habits, damage prevention, drugs, sexual behavior, mental health, oral health, atopy, asthma, personal hygiene, Internet addiction, equity in health, and others. The raw data from 2009 KYRBS were obtained by submitting a written pledge and a written use plan according to the procedure posted in its homepage on January 6, 2012.
This study drew and used 27 analyzable questions. The factor analysis (principal component analysis) of these questions drew five components, subjective health recognition, meal frequency, negative food intake, physical activities, and personal hygiene and, finally, drew three questions about health recognition, degrees of happiness, and stress for subjective health recognition; three questions about frequency of breakfast, lunch, and supper in the most recent seven days for meal frequency; three questions about frequency of having soft drink, junk food, and instant noodles for negative food intake; three questions about the numbers of intense physical activities, moderate physical activities, and strengthening exercise done for physical activities; and five questions about hand-washing with soap for personal hygiene.
These results were obtained by carrying out Varimax rotation among factors whose Eigen values were found to be 1 or more by factor extraction and by removing questions unclassified in terms of constructs. The total variance was 60.98% and reliability was Cronbach's=.64 for the subjective status, Cronbach's=.69 for meal frequency, Cronbach's=.50 for negative eating habits, Cronbach's=.73 for physical activities, and Cronbach's=.85 for personal hygiene. Construct reliability and average variance extracted were estimated to test the validity of the instrument. As a result, the construct reliability was .662~.860 and the average variance extracted was .395~.560, with variances extracted for negative eating habit factors invalid at less than .40 but the others valid.
Since latent mean analysis is aimed at seeing intergroup differences, is not affected by measurement errors, is contrary to t-test or ANOVA, and is a more careful and accurate method to test wrong intergroup differences (Hong, Malik, & Lee, 2003), this study used it to see differences in health behavior between the two groups. The analysis was carried out in the following way:
The collected data were analyzed by using SPSS 14.0 and AMOS 7.0. SPSS 14.0 was used for the reliability and factor analyses of the measurement instrument while AMOS 7.0 was used for the confirmatory factor analysis and latent mean comparison.
The confirmatory factor analysis was carried out to test goodness of fit for the measurement model applying maximum likelihood estimation while TLI, CFI, and RMSEA values were used to test goodness of fit for the model. Multi-group factor analysis was carried out to test construct equivalence to see configural., metric, and scalar invariances between the groups with and without a disease. Cofigural invariance is to identify if the two group's structures being measured coincide with theoretical model, metric invariance is to identify that the measurement methods between two groups are equivalent. Scala invariance is to identify equivalence of each measurement variable's scala, we can regards that the difference of observed value that was identified through scala invariance varification reflect difference of latent variables between groups. In testing goodness of fit for the model, root mean square error of approximation (RMSEA), which is an index that is less affected by the sample size than other types of goodness of fit and prefers economy of the model, and the comparative fit index (CFI) for measuring model errors under no influence of the sample size, though giving no consideration to economy of the model, were used as the goodness of fit indices.
Latent mean analysis cannot estimate the mean of each factor directly but can only estimate the latent mean for one group with that for the other group fixed at 0; thus, this study fixed the value for the group with no disease at 0. To interpret the latent mean comparison and latent mean differences, Cohen's effect size was estimated. According to the criteria suggested by Cohen (1988), the d value of .2 means a small effect size, .5 a medium effect size, and .8 a large effect size.
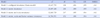
The respondents' general characteristics included genders, parents' education, economic levels, residence types, and school years. The health problem types for the group with a health problem and the results are shown in Table 1. In the group with a health problem, the most frequent type was atopic dermatitis (79.4%), followed by rhinitis (16.7%) and asthma (3%), with gastritis, diabetes, cancer, and kidney disease classified into a single category of others (0.7%)(Table 1).
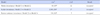
Correlations among latent variables (health behavior factors) used to test the causal structure established in this study were analyzed and the results are shown in Table 2. There were significant correlations among variables other than physical activities, meal frequency, personal hygiene, and negative eating habits in the group with a disease. There was no correlation among negative eating habits, personal hygiene, meal frequency, and physical activities but there was significant correlation among the other latent variables in the group with no disease.
Convergent validity means the extent of correlations between two or more measurement instruments in terms of one latent variable. Methods for assessing it include construct reliability or composite reliability, and extracted average variance extracted.
Construct reliability and average variance extracted were estimated for each variable; as a result, construct reliability values were .662~.860 and average variances extracted were .395~.560, with the variances extracted for negative eating habit factors invalid at less than .40 and the others having a convergent validity.
Discriminant validity aims to assess the extent of differences between one latent variable and the other. In other words, there should be definite differences in estimates among different constructs. Anderson and Gerbing (1988) suggested that when '∅±2·SE' is not 1 at a 95% confidence interval., it has discriminant validity, as a method for determining if the hypothesis of construct equivalence (interconstruct correlation coefficient=1.0) is rejected. The estimates for testing discriminant validities estimated on this basis are distributed between .210 and .156, showing no problem with discriminant validity.
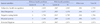
TLI, CFI, and RMSEA values were used to test goodness of fit for the measurement models in terms of five factors: subjective health recognition, meal frequency, negative food intake, physical activities, and personal hygiene. As a result, while Models 2 and 3 were both found to be fit, Model 3 having five factors for the large construct of health behavior (hierarchical model) was determined to be fitter to the basic assumptions of this study than Model 2 having a group of five factors in progressing into the next stage. Consequently, construct equivalence was tested with Model 3 (Table 3).
Comparison was made in terms of models for measuring the five latent variables between the groups with and without a health problem to test the configural invariance of the model for measuring. For goodness of fit for the baseline model to permit correlations among all latent variables and estimate parameters freely, the group with a disease had (df=218, N=75,066)=29, 047.795, p<.000, TLI=.894, CFI=.915, and RMSEA=.042, making it possible to analyze the structural model.
The metric invariance model is a model with invariance restrictions and identical factor loadings on latent variables for the groups with and without a disease. In this study, the baseline model (Model 1) permitting correlations among all latent variables and estimating parameters freely exhibited satisfactory goodness of fit (Table 5) and the metric invariance model (Model 2) imposing identical loading on both groups had almost the same goodness of fit. RMSEA and TLI are indices also considering conciseness of the model and identification restrictions are not rejected unless the index of the model imposing metric invariance restrictions becomes worse than that of the baseline model (Kim, Kim & Hong, 2009); therefore, metric invariance is confirmed in this study because the index of goodness of fit for the metric invariance model has not become worse than that for the configural invariance model (Table 4).
The scalar invariance model suggests identical scalars of measurement variables for the groups with and without a disease. Scalar invariance was tested after configural and metric invariances were confirmed. Comparison was made in goodness of fit between the metric invariance model (Model 2) and the scalar invariance model, imposing identification restrictions on the scalars of each measurement variable (Model 3); therefore, scalar invariance is confirmed because its index of goodness of fit has not become worse than that for the metric invariance model.
As for the general youth health behavior, subjective health recognition got a mean of 2.705 (5 for too unhealthy-1 for very healthy), showing low recognition of health, and the number of meals got a mean of 4.477 (5 for eating everyday-1 for almost no eating), showing almost no meal skipping. Negative eating habits got a mean of 1.784 (5 for very negative eating habits-1 for good eating habits), showing less negative eating habits. Exercise got a mean of 2.2175 (5 for lots of physical activities-1 for almost no physical activities), showing little exercise. Personal hygiene got a mean of 2.874 (5 for good habits-1 for bad habits), showing the middle level of hygiene. According to the simple mean comparison, students with a disease showed a little higher recognition of bad health in terms of health recognition, with almost no difference in the other items between two groups (Table 5).
Since configural., metric, and scalar invariance assumptions for latent mean comparison were all verified, latent mean comparison analysis was carried out to see if health behavior latent variables differed by the presence of a health problem. The latent mean for the group with no health problem was fixed at 0 for latent mean comparison in this study. As a result, there were significant differences in five health behavior components, subjective health recognition, meal frequency, negative eating habits, physical activities, and personal hygiene between the youth groups with and without a disease; however, the differences were small, the size of effects on them being .2 or less in all latent variables.
This study was conducted to see if health behavior differed between adolescents with and without a health problem. Factor analysis was carried out to draw five constructs, subjective health recognition, meal frequency, negative eating habits, physical activities, and personal hygiene and sub-variables for each construct. Health behavior was defined in different ways by different researchers, generally including nutrition and eating habits, safety and accident prevention, stress control and mental health, disease prevention, exercise, drug use, smoking, drinking, and medical checkup (Park & Lee, 2002), which can vary with studies. This study did not include safety accident prevention, disease prevention, drug use, smoking, and drinking. Since this study aimed to see if students with a health problem practiced more healthful actions to prevent a health problem from developing or becoming chronic in daily living than general ones rather than taking interest in health-threatening behavior, it may be possible to confirm differences in health behavior in general living with the five health behavior constructs included in this study.
After confirming construct equivalence, the multi-group latent mean analysis of health behavior between the groups with and without a disease was used to see statistically significant differences, whereas Cohen's effect size was found to be less than .2 for all of the five constructs; consequently, there was no difference in health behavior between the two groups. The statistically significant differences are considered to be related to the large sample size.
These results were different from the expectation that the group with a health problem would do better health behavior. Besides the results, while the group with a health problem was expected to do more desirable health behavior than the healthy group, regardless of age, previous research also didn't meet the expectation all the time. Oh (2011) and Gu (2006), who investigated differences in health improvement behavior by the presence of a disease among the elderly, found no difference between the two groups. It was also reported that health improvement behavior didn't differ by the presence of a chronic disease in terms of general characteristics, such as age and gender (Gu, 2006; Oh, 2011). Kim et al., (2001), who investigated health behavior, including eating habits and exercise habits, and risk behavior between the allergic and normal groups aged 19 years or older, found that there was no difference by the presence of allergy in terms of exercise, smoking habits, and drinking and that the allergic group ate significantly more meat than the normal group in terms of eating habits, contrary to the expectation. That is, the group, despite allergy, didn't avoid meat which was likely to be an allergy source. This result demonstrated that although long-term health-threatening behavior caused the disease, there had been no change in health behavior. Yang et al.,(2009), who made comparative research in eating habits and food patterns by the presence of an allergic disease, also reported that there was no difference in diverse health actions and that drinking frequency was significantly higher in the allergic patient group than in the normal group, contrary to the expectation. Despite the allergic disease, the group with a disease showed no differences in drinking, eating habits, or food patterns but drank more than the group with no disease, thus making no change in health behavior and maintaining even worse habits.
While those with a disease are generally expected to do better health behavior to prevent the disease from developing, there was actually no difference between the groups with and without a disease and the former tended to fail to perform health behavior well, contrary to the expectation. This tendency made it possible to expect that it would be difficult to demonstrate health improvement behavior despite the disease in adolescence when admission exams and keeping company with peers were important. Among the studies on adolescents with a health problem, the research in subjective disease recognition among adolescents with diabetes classified them into the receptive reliance coping type for accepting the fact that they had diabetes and were positively practicing diet and exercise; the extroverted support-pursuing type for informing that they were diabetic and trying to get assistance; the negative emotional coping type for denying the fact that they had diabetes and rejecting diet and blood sugar tests; the conflicting belief-pursuing type for believing that they would recover and were being anxious about the future due to a disease at the same time; and the realistic burden-reinforcing type for feeling exhausted from diabetes control and getting disappointed and anxious about poor control (Choi, Kwon & Kim, 2006). This implied that students with a health problem in adolescence could face different conflicts from what adults had and that they needed special management even in living.
Even if the health problem was expected to become chronic and cause serious problems, students in adolescence, who could hardly neglect their study due to anxiety about their future and fear of being alienated from their peer group, hardly seemed to leave school and lead a health-maintaining life. It was also expected that they would have difficulty keeping their own health behavior habitual while maintaining school life in school environment where everything, including meals, physical activities, and learning, was centered on healthy students.
As for research and consideration of youth health behavior, very few studies were conducted on health improvement behavior related to the presence of a disease and research was mostly conducted on the actual status of health behavior and prevention of healthy adolescents from committing risk behavior (Park & Lee, 2002). Previous research took interest in adolescents' health problems and focused on emotional problems, such as depression, stress, and bullying. Since adolescence was generally regarded as a physically healthy period, there were poor concerns about and few studies on some unhealthy adolescents and their health recovery and maintenance.
It was hard to find out research on health problem in adolescence, except some studies on juvenile diabetes, kidney problems, and atopy, which focused on identifying psychological effects of the disease and relevant factors, not on making the patients practice good lifestyle or health behavior (Choi et al., 2006; Joen, 2011; So & Yeo, 2012).
However, as can be seen from this study, students with a disease accounted for 41.7% and there were diverse health problems, including atopy, rhinitis, asthma, heart diseases, cancer, and diabetes, most of which needed control in living and prevention from worsening and becoming chronic. Jang and Choi (2010), who analyzed the data about 425 adolescents aged 12 to 18 in the data from the National Health and Nutrition Survey in 2007, found that hepatitis B antigen positive, innate heart diseases, attention deficit hyperactivity disorder, paranasal sinusitis, urinary tract infection, diarrhea, varicella, pneumonia, diabetes, hypertension, hypercholesterolemia, hypertriglyceridemia, and anemia had a morbidity of 42.6%; thus, the disease type differed slightly but it had a similar prevalence rate.
A consistent result in terms of health behavior factors for adolescents was that the younger an adolescent, the higher the health behavior level (Park & Lee, 2002); however, a continuous result was that no particular effort exerted for exercise or diet was on the increase on a yearly basis, probably because competition in admission examinations reduced the amount of time for health improvement behavior and increased health-threatening behavior as school years proceeded (KCDC, 2008: Ministry of Education Science and Technology, Ministry of Health and Welfare & KCDC, 2012: So, Kim, & Kim, 2011). The environment where even generally healthy students felt the stress of competition in admission examinations was expected to get those with a disease in more trouble.
As for chronic health problems, good daily control was an important prerequisite for preventing complications and maintaining a healthy life rather than trying to heal them completely. Since health problems that appear in childhood persist through life and have a longer duration than those that appear in adulthood, they require significant control from the early stage. Diabetes is a typical chronic disease and juvenile diabetes primarily appears at the ages of 10 to 12, has a higher prevalence rate, and leads to complications at an early age (Choi et al., 2006). While diabetes needs management to keep blood sugar at the normal level through diet, exercise, diabetes mellitus test, insulin injection, and hypoglycemia (Choi et al., 2006), diabetic adolescents are expected to have difficulty maintaining self-control in getting together with healthy peers and in the process of preparing for admission examinations and also experience difficulty keeping controlled while leading a school life without personal., special concerns about or management of students with a disease.
They are also expected to differ from adults in coping emotionally with chronic health problems. Adolescents are characterized by the tendency of believing that they are healthy. Jang and Choi (2010) reported that 15.9% experienced a sense of discomfort over the recent two weeks, whereas 95.3% believed that they were healthy; thus, they tended to believe that they were healthy although they experienced a sense of discomfort. It was therefore expected that even if they had a disease, they would not take it as seriously as adults. Adolescents in the process of physical., psychological., and social maturation were also expected to discover differences between their expectation and those they would actually be given, feel anxious about their future, identify the differences from their peers, and experience a conflicting crisis situation when they were diagnosed with a disease. And, many studies have shown that children who have chronic health problems are more exposed to greater stress than normal children. But, in fact what they are really stressed out by are mainly study and relationships with friends rather than physical problems. Furthermore they recognize themselves negative about study and relations with friends compared to healthy children (Choi, Shin, Chung, & Kim, 2000). These situations may be the main reason why they focus more on the friendship or studying rather than maintaining health behavior to maintain good health.
It was essential to prevent a disease from persisting into adulthood however mild or severe health problems appeared in adolescence. Since chronic health problems were particularly developed due to a bad long-term lifestyle, it was necessary to make the most intense efforts to establish health habits so that the disease that had already appeared in adolescence could not become chronic in adulthood. Chronic health problems affect the quality of living through life. Therefore, even if only a few students experience a health problem in adolescence, it is necessary to develop a specific supporting program and implement a practical policy so that they can prevent the health problem from developing and recover and improve health while leading a school life.
This study was conducted by using the raw data from the 2009 KYHBS determine if health behavior differed between adolescents with and without a health problem; thus, 5 constructs of health behavior (subjective health recognition, meal frequency, negative food intake, physical activities, and personal hygiene) and 22 sub-items were drawn. After testing construct equivalence among these five constructs, the differences between the groups with and without a health problem were analyzed by using them as latent variables. It was found that 41.7% of the adolescents had a health problem and their health behavior didn't differ from that of the group with no health problem. While this study made a comparison between the groups with and without a health problem, regardless of the health problem type, further research was needed to investigate health behavior according to the health problem or disease type with the objective of developing a health management program particularly required for each disease group. To develop a program for allowing students with a health problem promote their health behavior and for preventing the disease from worsening and becoming chronic, the first priority should be given to research for identifying more specific factors affecting health behavior practice among adolescents with a disease.
Figures and Tables
References
1. Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull. 1988; 103(3):411–423.

2. Choi MH, Kwon EK, Kim SK. A study on subjective perception of their disease by adolescents with IDDM. J Korean Acad Child Health Nurs. 2006; 12(3):322–332.
3. Choi SM, Shin MS, Chung CY, Kim ZS. Psychological characteristics in children with Chronical Physical illness and handicapped: Self-concept and stress coping strategy. J Child Adolesc Psychiatry. 2000; 11(2):252–261.
4. Cohen J. Statistical power analysis for behavioral sciences. New Jersey: Lawrence Erlbaum Associates, Hillsdale;1988.
5. Gu MO. A review of research on health promoting behaviors of Korean older adults. Perspect Nurs Sci. 2006; 3(1):17–34.
6. Health Insurance Review and Assessment service. Annual statistical report (Disease categories by age). 2013. 10. 22. Retrieved November 11, 2013. from: http://www.hira.or.kr/dummy.do?pgmid=HIRAA020045010000&cmsurl=/cms/information/05/03/01/1321469_13603.html&subject=2012%eb%85%84+%ea%b1%b4%ea%b0%95%eb%b3%b4%ed%97%98+%ed%86%b5%ea%b3%84%ec%97%b0%eb%b3%b4.
7. Hong SH, Malik ML, Lee MK, et al. Testing configural, metric, scalar and latent mean invariance across genders in sociotropy and autonomy using a non-western sample. Educ Psychol Meas. 2003; 63(4):636–654.

8. Jang EH, Choi EH. Health behavior and disease of children and adolescents. J Korean Soc Sch Health Educ. 2010; 11(1):57–66.
9. Joen SK. Nutritional status and health-related quality of life in children with chronic kidney disease. Seoul: Kyung Hee University;2011. Unpublished master's thesis.
10. Jung JI, Kum MH. The relation of health hazard behavior and health state in the elderly. Pap Kyungbuk Coll. 2002; 21:357–374.
11. Kim DS, Kim HS. Early initiation of alcohol drinking, cigarette smoking and sexual intercourse linked to suicidal ideation and attempt: Findings from the 2006 Korean youth risk behavior survey. Yonsei Med J. 2010; 51(1):18–26.
12. Kim JH, Kim MG, Hong SH. Writing the articles with structural equation model. Seoul: Communication Books;2009.
13. Kim MH, Lee DH. Factors related to health-promoting behaviors and chronic diseases in the elderly. J Korean Soc Health Educ Promot. 2011; 28(2):99–107.
14. Kim YM. The relationship between family structure and social control factors on adolescents smoking and alcohol. Korean J Youth Stud. 2006; 13(6):151–178.
15. Kim YS, Park JW, Song YS, Kim GY, Kim SW, Park JW, et al. The comparison of lifestyle patterns between allergy and non-allergy people food intake, exercise, smoking, alcohol intake. J Korean Community Nurs. 2001; 12(1):269–277.
16. Ko SJ. The effect of living habits on medical expenses. Seoul: Korea University;2006. Unpublished master's thesis.
17. Ko YK, Yoo IY, Kang KH, Lim JY, Kim MJ, Yoo HJ. Factors related to high-risk health behavior in middle school adolescents. J Korean Acad Child Health Nurs. 2006; 12(3):341–350.
18. Korean Centers for Disease Control and Prevention. Results of Korea youth risk behavior web-based survey (KYRBWS), 2006-2007, Report material. 2008. 11. 01. Retrieved October 10, 2013. from http://www.cdc.go.kr/CDC/notice/CdcKrInfo0301.jsp?menuIds=HOME001-MNU0004-MNU0036-MNU0037&cid=12193.
19. Korean Centers for Disease Control and Prevention. Guide book for model school for atopy and asthma management. 2010. 10. 05. Retrieved October 10, 2013. http://www.cdc.go.kr/CDC/together/CdcKrTogether0302.jsp?menuIds=HOME001-MNU0004-MNU0085-MNU0088&fid=51&q_type=&q_value=&cid=9892&pageNum=1.
20. Korean Centers for Disease Control and Prevention. History of Youth Risk Behavior Web-based Survey (KYRBWS). 2013a. Retrieved October 10, 2013. from http://yhs.cdc.go.kr/.
21. Korean Centers for Disease Control and Prevention. Results of Korea Youth Risk Behavior Web-based Survey (KYRBWS). 2013. Report material. 2013b. 10. 24. Retrieved October 10, 2013. from http://www.cdc.go.kr/CDC/intro/CdcKrIntro0201.jsp?menuIds=HOME001-MNU0005-MNU0011&cid=21764.
22. Lee JH. Health risk behaviors of adolescents out of school. Suwon: Sungkyunkwan University;2008. Unpublished master's thesis.
23. Ahern NR. Risky behavior of adolescent college students. J Psychosoc Nurs Ment Health Serv. 2009; 47(4):21–25.

24. Ministry of Education Science and Technology. Ministry of Health and Welfare. Korean Centers for Disease Control and Prevention. A statistical analysis of 7th online survey on adolescents' health behavior in 2011. 2012. Retrieved October 10, 2013. http://stat.mw.go.kr/front/statData/publicationView.jsp?menuId=47&bbsSeq=13&nttSeq=18847&searchKey=&searchWord=&nPage=2.
25. Oh HJ. The study on the affluence factors on elderly health. Busan: Inje university;2011. Unpublished doctoral dissertation.
26. Park JM, Kim MW, Han EK, Kim HY. Related factors of internet addiction of Korean adolescence: Using the 5th Korean youth health behavior survey. J Korean Data Anal Soc. 2012; 14(4B):2067–2080.
27. Park NH, Lee HJ. A Critical review of health behavior studies of adolescents conducted in Korea. J Korean Community Nurs. 2002; 13(1):98–114.
28. So ES, Yeo JY. Relationship between health status and life styles and atopic dermatitis in adolescents. J Korean Acad Child Health Nurs. 2012; 18(3):143–149.

29. So SS, Kim HK, Kim CS. Comparative study of gender and school grade differences in adolescent health. Korean J Youth Stud. 2011; 18(10):317–340.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download