Abstract
Purpose
In this study an examination was done of the effects of a team-based learning program on enhancement of communication competence for undergraduate nursing students in South Korea.
Methods
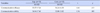
quasi-experimental method with a non-equivalent control group pre- and post-test design was used. Participants were 68 undergraduate nursing students recruited from two universities. The experimental group (n=35) received a 5-week team-based learning program on enhancement of communication competence, while the control group (n=33) received traditional lectures. Data were collected using self-report structured questionnaires before and after the intervention, and were analyzed using χ2 tests, Fisher's exact tests, and t-tests.
The ultimate goal of nursing education is to produce and nurture a nursing workforce with the theoretical knowledge and clinical performance ability needed by society. The Korean Accreditation Board of Nursing Education (KABON) [1] has recently recommended the establishment of a performance-based education system, and the improvement of education programs through nursing education accreditation in order to produce competent nurses. The KABON has included communication ability as one of 12 core competencies that nurses need to acquire through nursing education programs.
The nature of nursing means that a nurse's communication ability is a core competency essential in nursing practice, and is a major factor in determining professional ability enhancement and leadership [2]. For this reason, the need of continuous education to develop nurses' communication competence has been recognized in nursing practice.
To improve the applicability of communication skills, it is crucial to use a wide range of learner-centered teaching methods and to avoid conventional lecture-style instruction [3]. However, according to a study on the current status of communication education [4], more than 90% of domestic nursing colleges were found to implement lecture-based teaching methods, and 95.8% of colleges were evaluating students on the basis of test performance and attendance. The traditional lecture-centered education method for communication has become an underlying cause of the difficulty that nursing students experience when interacting with various subjects and other medical staffs [5]. Moreover, according to new education goals, changes and innovation are essential in overall nursing education-including communication-to keep pace with the rapid changes in current medical practice [6].
Considering the latest trends, a variety of teaching and learning methods have been applied to nursing education to enhance students' learning satisfaction and their ability to apply what they have learnt in clinical practice. In addition to problem-based learning (PBL) and simulation-based learning (SBL) methods, team-based learning (TBL) is one of the leading methods for improving nurses' ability to utilize the skills they have learnt in actual clinical practices. Unlike PBL or SBL, TBL extensively uses learning strategies that maximize learning effectiveness by increasing student participation [7].
One leading strategy is advanced preparation for learning topics in order to promote participation in learning content; this is achieved by encouraging students to attend sessions already prepared to focus on the learning objectives. Moreover, TBL has the advantage that classes are conducted by a single professor, and group activities are organized without additional assistants or facilitators, even in a large-scale lecture. The seven core factors in the TBL conceptual model proposed by Haidet et al [8] imply that a professor can facilitate participation of a large number of students in learning groups. For these reasons, TBL has been increasingly used in recent years for healthcare professionals [9].
TBL has been diversely applied abroad in the field of healthcare education, and its effectiveness has been verified [101112]. The leading effects are seen in the communication ability of learners, interpretation ability, team-work technique, ability to apply acquired knowledge, learning satisfaction, and other benefits. In addition to the promotion of learners' ability to clinically apply acquired knowledge, there are improvements in communication ability and teamwork technique. This is because the TBL program is a learning method that requires a lot of communication between teams [713].
In evaluating the level of readiness, TBL not only determines the degree of individual learning, but also attempts to facilitate team communication until agreement of opinion is reached. Consequently, this learning method balances a student's level of readiness [8]. Moreover, the entire learning process involves communication among team members.
Therefore, the application of the TBL program before the experience of clinical practice, and the verification of its usefulness, is important for the development of this teaching-learning method to enhance communication competence in nursing students. In recent years, studies of the application of TBL as a practice-oriented learning method have been performed in nursing homes and abroad [13]. However, previous nursing studies using TBL have mainly investigated basic nursing procedures [141516].
Therefore, this study aimed to develop a TBL program for enhancement of communication competence in nursing students as an ultimate goal of communication education, and to verify its effectiveness. The results of this study could be used as a comprehensive reference base to develop a teaching-learning method for enhancement of communication ability as one of the core competencies of nurses.
The purpose of this study is to verify the effects of the application of a TBL program on communication efficacy and communication ability in nursing students, to determine whether this method enhances communication competence. The hypotheses of this study are as follows:
Hypothesis 1. Scores of communication efficacy scores will be higher in the experimental group receiving the TBL program than in the control group with the lecture-style instruction.
Hypothesis 2. Scores of communication ability will be higher in the experimental group receiving the TBL program than in the control group with the lecture-style instruction.
Hypothesis 3. Scores of learning satisfaction will be higher in the experimental group receiving the TBL program than in the control group with the lecture-style instruction.
This was a quasi-experimental study with a nonequivalent control group pre-post test design to identify the effects of a TBL program for communication competence improvement on communication competence of nursing students.
The subjects were selected through convenience sampling from an accessible population of sophomore students in the Department of Nursing at two 4-year universities with similar size and levels. in G city, South Korea. This study included nursing students without previous experience of communication education, who were informed about the purpose of the research and gave their informed consent for participation. The minimum number of subjects required was 28 to perform an independent samples t-test using the G*Power program, version 3.1.2.
The significance level (a) of p was set at .05, with statistical power at .90 (1-β), and an effect size (d) of .80. The choice of the large effect size was based on the results of previous studies [8141516], which showed that TBL was significantly more effective than a lecture-style teaching method. Some students withdrew from the study, leaving 74 students, 37 of which were in the experimental group and 37 in the control group. From this total two subjects withdrew from the study due to personal circumstances and four subjects' responses were excluded because of response bias. A total of 68 subjects were finally enrolled for analysis, 35 in the experimental group and 33 in the control group.
This study evaluated communication efficacy, communication ability, and learning satisfaction. All instruments were approved for use via email from tool developers. Content validity was tested by eight experts, including a professor in the Department of Psychiatry, three professors in the Department of Mental Health Nursing, a professor on the Education course, and three nurses, each with 2 years of work experience in psychiatry. The study used only items with a content validity index (CVI) score of .80 or higher.
The instrument used to measure communication efficacy was a self-efficacy scale developed by Ayres [17] and translated, revised, and modified by Park and Kweon [18]. The author of this study further revised terms so that they were appropriate for the subjects. The scale included 10 items to be rated on a 7-point scale, and the scale scores ranged from 10 (lowest) to 70 (highest). A higher score indicates a higher level of communication efficacy. Cronbach's α was .57 at the time of development, and .95 in the study by Park and Kweon [18]. Cronbach's α was .92 in this research.
The instrument used to measure communication ability was the revised version of the Global Interpersonal Communication Competence Scale (GICC) developed by Rubin et al. [19], and translated and modified by Hur [20]. The scale included 15 items rated on a 5-point scale, and the scale scores ranged from 15 (lowest) to 75 (highest). A higher score indicates a higher level of communication ability. Cronbach's α was .80 at the time of development, and .93 in this research.
Learning satisfaction was evaluated using a satisfaction scale developed by Kang [21] and revised and modified for this study after verifying content validity of the instrument. The original scale included 12 items, but this study excluded three items with a CVI score of less than .80 in the content validity test. The revised version of the scale included nine items to be rated on a 5-point scale, and the scale scores ranged from 9 (lowest) to 45 (highest). A higher score indicates a higher level of learning satisfaction. Cronbach's α coefficient was .91 in this study.
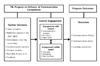
Team-based learning is an instructional strategy that combines independent out-of-class preparation for in-class discussion in small groups [13]. The conceptual framework of the TBL program for communication competence enhancement in nursing students was completed based on analysis of learning needs and the TBL model of Haidet et al. [8] (Figure 1).
The detailed content and development procedure are as follows: In the initial stage of program development, the content of the program was arranged by analyzing the learning needs of 87 sophomore nursing students with prior experience of attending communication-related courses. Students considered that the most effective teaching-learning method for communication education was a case-centered method, and that effective education strategies were role-play and video clips. According to a survey, students expected to improve their communication ability, acquire communication skills, be provided with practice-oriented classes, and become prepared for actual casework through detailed case studies presented in communication education. Students expected to acquire methods applicable to daily living by focusing on case studies.
In the second stage of development, the program was designed by applying the conceptual framework of the TBL model proposed by Haidet et al. [8]. The TBL model comprises three components, including instructor's decision, learner's participation, and academic performance. First, in the instructor's decision process, an instructor begins to prepare for a lecture to enhance learning. The seven core factors of the instructor's preparation are as follows: (1) Team organization, (2) Development of readiness assurance tests (Individual Readiness Assurance Test [IRAT] and Group Readiness Assurance Test [GRAT]), (3) Prompt feedback, (4) Written appeals, (5) Four S factors (significant problem, same problem, specific choice, simultaneous reporting), (6) Structured reward system, and (7) Peer review.
Second, the learner's participation is the core concept of the TBL model. The second component is classified into individual-level participation in learning content and the learner's participation in a team. The third component is academic performance, composed of communication knowledge, communication efficacy, problem-solving ability, perceived communication ability, communication performance ability, and learning satisfaction.
In the third stage of development, the purpose and topic of the program were established. The author chose important communication theories and methods commonly featured in communication education.
The author confirmed four learning topics, including Eric Bern's transactional analysis, Satir's congruent communication, the I-message, effective communication skills, and five academic goals, including orientation, based on advice from four professors in the Department of Mental Health Nursing.
The fourth stage of development organized the application methods and assessment tools of the program. The program was designed to apply scenario-based learning modules for team problem solving, and to carry out reporting and debriefing according to topics and goals. In the last session, time was given to examine communication performance ability utilizing standardized patients to improve communication competence.
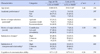
The TBL program was carried out for 120 minutes in each session, for 5 weeks. The learning process is shown in Table 1. Excluding the first session of orientation and team building, a scenario-based learning module was taught each week for 4 weeks. The program was conducted using four different scenarios, by applying instances of communication, and was performed according to the following phases by session.
In the first phase, the author instructed learners to use the Internet to go through the concept and content of learning in advance, by providing a reading assignment at the online learning center a week before every session. In the second phase, 5 minutes were allocated to the beginning of a lecture session to introduce the learning topics and goals. In the third phase, the author performed the IRAT, consisting of 5~8 questions with 5 multiple choices, in each session. Through this process, the study checked understanding of major prerequisite concepts in individual learners. Immediately after the test, questionnaires were placed in envelopes and distributed to each team, and these were returned to the investigator. Five minutes were given for this process. In the fourth phase, the GRAT was conducted, and team members were asked to find answers to questions by integrating different opinions through discussion and agreement, comparing answers of each member and team. After submission of answers, seven teams were asked to present answers to each question at the same time using a smartphone number board application programming in order to compare different answers. The correct answers to questions were provided immediately, to enable learners to check answers; 10 minutes were allowed for this process. The fifth phase featured written appeals, where learners were required to ask questions about curious or unclear parts they had identified when reading the assignment. A document was provided for learners to make objections on readiness assurance tests. Ten minutes were given for this process. The sixth phase consisted of instructor feedback, in which a short lecture was given for 15 minutes, mainly on primary concepts, in response to students' questions and the results of the readiness assurance tests. The seventh phase comprised written appeals on learning topics, where learners were encouraged to participate in situations featuring applied scenarios. Students' interest and concentration were encouraged by requiring them to produce learning scenarios in the form of animated videos of about 5 minutes in length. The eighth phase featured team problem solving after presenting an assignment; this involved applying the concept of learning content to solve given problems by distributing learning scenarios as a document. Results were written on an easel pad and posted on the wall of the lecture room by each team. This process took about 40 minutes. In the ninth phase, each team demonstrated the results through role-play by sharing roles with team members, and feedback was provided by peers and instructors through debriefing; about 20 minutes were spent on this process. In the tenth phase, each team was asked to vote for two outstanding teams-excluding their own team-by assigning stickers; the two teams with the highest number of stickers were complimented and given reward points. Each session finished by notifying students of the next session and requesting advanced preparation of the learning topics. This last process took about 10 minutes.
Traditional lecture-style sessions were given to the control group, containing exactly the same learning topics as given to the experimental group. The learning time was the same for both groups: 120 minutes per session. After all the experimental procedures were completed, the control group also provided educational programs similar to those provided to the experimental group.
This study was conducted after gaining IRB approval (IRB No. 13-009) from C University. All subjects were fully informed about the purpose and methods of the study and that there were no potential side effects or risks from participation. Participation was voluntary and written consent was obtained. Subjects were guaranteed confidentiality of gathered data, anonymity, and the choice of withdrawing from participation at any time. All data for analysis were stored on the investigator's laptop computer, and a security password was used for access. During the program, feedback from the students in the experimental group on their participation in the program was collected as a qualitative data. Treatment and data collection were conducted six times in the experimental group, from May 1 to June 15, 2013. All treatment was done during communication class, one of the regular curriculum. The lecture and TBL program proceeded after approval of the head of the school. The program was conducted by a researcher who was not involved in evaluating students at the university. The researcher is qualified as a mental health nurse, completed 12 years of psychiatric care, 8 years of mental nursing and communication lectures, and a team-based learning curriculum for the first time four years ago and then participated in the training each year. The appropriate number of TBL members is eight or less, since learning is conducted by students' own collection of data as a basis for problem solving and exchanging opinions through discussion [20]. For this reason, this study assigned about five to six members to each of seven experimental groups, in order to apply TBL. A pretest survey was performed at the first session, for both experimental and control groups. Respondents were given about 10~15 minutes to complete the questionnaire. A posttest survey of both groups was performed immediately after examining communication.
Collected data were analyzed using SPSS version 20.0, and differences were considered statistically significant at p<.05. The general characteristics and dependent variable scores of both groups were analyzed using the χ2 test, Fisher's exact probability test, and t-tests, to verify pre-homogeneity between the two groups. An independent samples t-test was conducted to identify differences between the two groups before and after applying the TBL program.
Hypothesis 1. Table 4 represents differences in communication efficacy between the two groups before and after applying the TBL program. Significant differences (t=2.58, p=.012) were found between the experimental group who received the program and the control group who received lecture-style learning. Hypothesis 1 was supported by the results obtained.
Hypothesis 2. Table 4 represents differences in communication ability between the two groups before and after applying the program. Significant differences (t=12.01, p<.001) were observed between the two groups. Hypothesis 2 was supported by the results obtained.
Hypothesis 3. Table 4 represents differences in learning satisfaction between the two groups after implementing the program. Significant differences (t=2.11, p=.039) were found between the two groups. Hypothesis 3 was supported by the results obtained.
The TBL program developed in this study was found to be effective in improving communication competence in nursing students. The implications of the study are as follows:
First, the TBL program designed to enhance communication competence was effective in improving communication efficacy. In general learning-related efficacy is associated with students' belief that they can substantially apply lecture content [22]. This study indicated that this belief was enhanced in the experimental group compared to the control group with lecture-style learning. The results of this study were comparable to those of previous studies by Ayres [17], who reported enhancement of learning efficacy in nurses and nursing students after communication education. Those studies [1718] applied a small team-based approach, and students were provided with opportunities to explore solutions for given cases in cooperation with team members, and to make corrections through team discussion.
In this study, nursing students created new, effective communication circumstances by actively participating in learning themselves during the TBL program, and demonstrating the outcome through role-play. Moreover, communication efficacy enhancement is thought to be attributable to improved self-confidence and reduced fear of communication by exchanging feedback among members through debriefing. The subjects reported that they were able to do better in case studies after learning how to communicate by analyzing the learning scenarios provided and searching for effective communication skills. Moreover, one student stated, “I feel like I definitely have acquired communication skills by demonstrating in role-play learning content that I would have previously only expressed in written form. During the learning process, learners are anticipated to gain confidence with effective communication when they are provided with opportunities to express themselves through role-play, by proactively searching for solutions to given scenarios. The study findings suggest that a TBL program can enable self-directed learning based on actual cases, and is likely to be beneficial in enhancing communication efficacy in nursing students.
For TBL to be effective in helping students learn to apply specific theories, advanced preparation of both instructor and learner is crucial. In this study, the reading assignment provided by the investigator, and the learner's readiness, had a considerable effect on knowledge improvement. The easy reading assignment was given to nursing students to facilitate advanced preparation for learning, and understanding of basic concepts was promoted through IRAT and GRAT. Moreover, prompt feedback was provided to correct errors in knowledge. The subjects stated that repeated study of major concepts through the reading assignment, tests, and a short lecture facilitated their learning, although more ambiguous theories and concepts of communication were difficult to understand. In working with their teams to apply and analyze communication theories with respect to learning scenarios, repeated exploration and confirmation of concepts were encouraged, and communication efficacy enhancement was attributable to the self-directed search for necessary information. Learning efficacy is likely to be improved by iterative learning within a limited time. TBL is considered a very effective learning method because it enables a high standard of communication through interaction with team members [678].
Second, the TBL program was effective in enhancing communication ability. The present findings support previous work indicating that TBL can boost communication ability in students majoring in healthcare related fields [12], and in nursing students [1323]. Communication among learners was sustained in the process of summarizing, reporting, and debriefing on the outcome of effective communication, which was analyzed in terms of the scenarios. Thus, TBL is based on group solidarity and reliability. Learners share responsibility for the quality level of individual and group assignments [9]. In traditional lecture-style learning, learners-unlike instructors- have no responsibility. Learners who were previously concerned only about their own academic performance in lecture-style learning have to take responsibility for both the quality and quantity of individual and group assignments in the TBL program. For this reason, participating students must, in addition to individual learning, engage in continual discussion with team members in order to find better solutions to problems. Significant problems were structured by suggesting the actual events or circumstances that could occur in the daily life of students.
Yedidia et al. [24] proposed that, in addition to lectures, case study practice exercises are needed in communication education to enable students to acquire communication skills more effectively. These TBL measures facilitated cooperative learning and communication, and promoted student participation. Learners were also provided with the opportunity to demonstrate appropriate solutions to a given case; they engaged in substantial communication and cooperative learning within a short period of time by sharing roles and expressing themselves. Kesten [25] suggested that communication education enhanced communication performance ability in nursing students through demonstration, such as role-play. Through this process, students become more cooperative. Baghcheghi, Koohestani, and Rezaei [26] verified that cooperative learning during the TBL program was very effective in enhancing subjects' communication skills. Therefore, the ability of a TBL program to generate cooperative learning is thought to be beneficial in improving nursing students' communication ability.
Third, the level of learning satisfaction was found to be higher in the experimental group receiving the TBL program than in the control group who received the lecture-style learning. This outcome reflects that of previous work suggesting that TBL increased learning satisfaction in students [27]. Learning satisfaction accelerates acquisition of knowledge and skills in students by enhancing confidence in studying and self-efficacy. Thus, learning satisfaction is profoundly associated with academic performance, and the correlation is more distinct in difficult curriculum subjects [8]. When students actively participate in learning, problem solving elicits a sense of challenge, rather than one of boredom, and this eventually leads to an increase in academic achievement level [9].
In a well-designed TBL program, students are more actively involved in the learning process and their satisfaction levels increase, along with a remarkable level of interaction between learners and instructors. Therefore, an instructor needs to be prepared for the program, to aid students in achieving satisfaction through positive learning experiences [28]. The subjects of this study stated that they enjoyed interactions with team members, and that the new learning program was interesting and effective in tackling the given problems. Their responses reflected their positive evaluation: “I had a chance to become acquainted with unfamiliar teammates, and I was interested in the program because many members came up with good ideas,” and “I was worried about reading the assignment at first, but later, it was interesting and meaningful to tackle problems during the program because I was prepared for discussion.” These responses support the proposal of Rosenbaum and Ferguson [29] that active participation of students improves learning satisfaction. Sufficient readiness and preparation for learning topics on the part of both instructors and learners were found to be helpful in generating interest in learning content and promoting active participation [30].
To sum up the above findings, the TBL program had a favorable effect on communication efficacy and communication ability in nursing students, and improved students' learning satisfaction. In a rapidly changing healthcare field, it is more important to educate nursing students to utilize communication effectively to better adapt themselves to clinical practice. This study addressed this issue by applying a TBL program developed for communication competence enhancement to nursing students. Further studies need to investigate the effects of the TBL program on communication competence in newly graduated nurses.
This study aimed to develop a program for communication education and identify its effects. The results of this study revealed that the TBL program developed for communication competence enhancement was more effective in improving communication efficacy, communication ability, and learning satisfaction compared to traditional lecture-style learning. The TBL teaching-learning method was found to be appropriate for communication education, substantially enhancing communication competence by having favorable effects on students' participation, satisfaction, knowledge, and learning attitudes and skills. The results of this study might be useful as a comprehensive reference base from which to develop and apply effective education programs for improving communication competence, one of the core competencies in nurses. Such programs could contribute to producing well-prepared nurses who display effective communication skills and problem solving ability in working with a variety of healthcare professionals, patients, and peers.
Figures and Tables
Notes
References
1. Korean Accreditation Board of Nursing Education. Accreditation assessment standard for education of Korea. [Internet]. 2012. cited 2014 Feb 23. Available from: http://kabon.or.kr/kabon02/120120319133351.pdf.
2. Kim HK. Influence of interpersonal relations, communication skills, creative behaviors and nursing service on self-leadership among nurses in hospital. Clin Nurs Res. 2007; 13(1):25–36.
3. Idczak SE. I am a nurse: Nursing students learn the art and science of nursing. Nurs Educ Perspect. 2007; 28(2):66–71. DOI: 10.1043/1536-5026(2007)028[0066:IAANNS]2.0.CO;2.
4. Son HM, Kim HS, Ko MH, Yu SJ. Analysis of the communication education in the undergraduate nursing curriculum of Korea. J Korean Acad Soc Nurs Educ. 2011; 17(3):426–434. DOI: 10.5977/JKASNE.2011.17.3.424.

5. Yoo MS, Chae SM. Effects of peer review on communication skills and learning motivation among nursing students. J Nurs Educ. 2011; 50(4):230–233. DOI: 10.3928/01484834-20110131-03.

6. Lubeck P, Tschetter L, Mennenga H. Team-based learning: An innovative approach to teaching maternal-newborn nursing care. J Nurs Educ. 2013; 52(2):112–115. DOI: 10.3928/01484834-20130121-02.

7. Michaelsen LK, Parmelee DX, McMahon KK, Levine RE, editors. Team-based learning for health professions education: A guide to using small groups for improving learning. Sterling, VA: Stylus Publishing;2008.
8. Haidet P, Levin RE, Parmelee DX, Crow S, Kennedy F, Kelly PA, et al. Perspective: Guidelines for reporting team-based learning activities in the medical and health sciences education literature. Acad Med. 2012; 87(3):292–299. DOI: 10.1097/ACM.0b013e318244759e.
9. Roh YS, Ryoo EN, Choi DW, Baek SS, Kim SS. A survey of student perceptions, academic achievement, and satisfaction of team-based learning in a nursing course. J Korean Acad Soc Nurs Educ. 2012; 18(2):239–247. DOI: 10.5977/jkasne.2012.18.2.239.

10. Cho AR, Han SI, Yoon SH, Park JH, Yoo NJ, Kim S. Methods of effective Team-based learning administration and expected effects on medical education. Korean J Med Educ. 2010; 22(1):47–55. DOI: 10.3946/kjme.2010.22.1.47.

11. Thomas PA, Bowen CW. A controlled trial of team-based learning in an ambulatory medicine clerkship for medical students. Teach Learn Medicat. 2011; 23(1):31–36. DOI: 10.1080/10401334.2011.536888.

12. Thompson BM, Schneider VF, Haidet P, Levine RE, McMahon KK, Perkowski LC, et al. Team-based learning at ten medical schools: Two years later. Med Educ. 2007; 41(3):250–257. DOI: 10.1111/j.1365-2929.2006.02684.x.

13. Clark MC, Nguyen HT, Bray C, Levine RE. Team-based learning in an undergraduate nursing course. J Nurs Educ. 2008; 47(3):111–117.

14. Kang HY, Choi EY, Kim HR. Nursing student's experiences in team based simulation learning. J Korean Acad Soc Nurs Educ. 2013; 19(1):5–15. DOI: 10.5977/jkasne.2013.19.1.5.

15. Kim SO, Kim SM. Effects of team-based learning applying for nursing students on critical thinking ability, problem solving ability and communication ability. J Korean Data Anal Soc. 2016; 18(2B):1151–1161.
16. Sisk RJ. Team-based learning: Systematic research review. J Nurs Educ. 2011; 50(12):665–669. DOI: 10.3928/01484834-20111017-01.

17. Ayres HW. Factors related to motivation to learn and motivation to transfer learning in a nursing population [dissertation]. Los Angeles: North Carolina State University;2005. 325. https://www.lib.ncsu.edu/resolver/1840.16/3773.
18. Park SY, Kweon YR. The effect of using standardized patients in psychiatric nursing practice training for nursing college students. J Korean Acad Psychiatr Ment Health Nurs. 2012; 21(1):79–88. DOI: 10.12934/jkpmhn.2012.21.1.79.

19. Rubin RB, Martin MM, Bruning SS, Power DE. Interpersonal communication competence: Scale development and test of a self-efficacy model. Paper presented at: The meeting of the communication
association. 1991; Atlanta.
20. Hur GH. Construction and validation of a global interpersonal communication competence scale. Korean J Journal Commun Stud. 2003; 47(6):380–408.
21. Kang EJ, Cheon SM. The effect of a group cinematherapy program on the emotional regulation ability and problem behaviors of the youth at-risk. Korean J Youth Couns. 2011; 19(2):23–46.

22. Midgley C, Kaplan A, Middleton M. Performance approach goals: Good for what, for whom, under that circumstances, and at what cost. J Educ Psychol. 2001; 93(1):77–86. DOI: 10.1037/0022-0663.93.1.77.

23. Mennenga HA, Smyer T. A model for easily incorporating team-based learning into nursing education. Int J Nurs Educ Scholarsh. 2010; 7:Article4. DOI: 10.2202/1548-923X.1924.

24. Yedidia MJ, Gillespie CC, Kachur E, Ockene J, Chepaitis AE, Snyder CW, et al. Effect of communications training on medical student performance. JAMA. 2003; 290(9):1157–1165. DOI: 10.1001/jama.290.9.1157.

25. Kesten KS. Role-play using SBAR technique to improve observed communication skills in senior nursing students. J Nurs Educ. 2011; 50(2):79–87. DOI: 10.3928/01484834-20101230-02.

26. Baghcheghi N, Koohestani HR, Rezaei K. A comparison of the cooperative learning and traditional learning methods in theory classes on nursing students' communication skill with patients at clinical settings. Nurse Educ Today. 2011; 31(8):877–882. DOI: 10.1016/j.nedt.2011.01.006.

27. Andersen EA, Strumpel C, Fensom I, Andrews W. Implementing team based learning in large classes: Nurse educators' experiences. Int J Nurs Educ Scholarsh. 2011; 8:pii: /j/ijnes.2011.8.issue-1/1548-923X.2197/1548-923X.2197.xml. DOI: 10.2202/1548-923X.2197.

28. Arthur C, Kable A, Levett-Jones T. Human patient simulation manikins and information communication technology use in Australian schools of nursing: A cross-sectional survey. Clin Simul Nurs. 2011; 7(6):219–227. DOI: 10.1016/j.ecns.2010.03.002.

29. Rosenbaum ME, Ferguson KJ. Using patient-generated cases to teach students skills in responding to patients' emotions. Med Teach. 2006; 28(2):180–182. DOI: 10.1080/01421590500314165.

30. Vasan NS, DeFouw DO, Holland BK. Modified use of team based learning for effective delivery of medical gross anatomy and embryology. Anat Sci Educ. 2008; 1(1):3–9. DOI: 10.1002/ase.5.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download