Abstract
Purpose
The purpose of this study was to explore factors related to the medication compliance by severity levels of children on Attention Deficit Hyperactive Disorder (ADHD) medication.
Methods
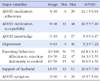
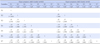
The method employed in this study was a descriptive correlational and cross-sectional survey design using face-to-face interviews. The survey was conducted from September, to October, 25, 2010 through a self-report questionnaire following consent of 143 mothers. Interview instruments, which were used in the study were CARS, PAI, ADHD knowledge instrument, BDI, a maternal behavior instrument, TAQ, and TAB instrument. Descriptive statistics, t-test, analysis of variance, and Pearson' correlation were used for data analysis.
Results
Mothers who perceived their children as not hyperactive were significantly higher in accepting medication and positive maternal behaviors than mothers who perceived their children as hyperactive. The mother perceived their children as not hyperactive showed positive correlation to adherence with ADHD medication and ADHD knowledge but a negative correlation with depression and children's ADHD symptoms. There was, however, no correlation between medication adherence and any other variables in the mothers of children with hyperactivity.
Figures and Tables
References
2. Arcia E, Fernandez MC, Jaquez M. Latina mothers' stances on stimulant medication: Complexity, conflict, and compromise. J Dev Behav Pediatr. 2004. 25:311–317.

3. Brinkman WB, Sherman SN, Zmitrovich AR, Visscher MO, Crosby LE, Phelan KJ, et al. Parental angst making and revisiting decisions about treatment of ADHD. Pediatrics. 2009. 124:580–589.
4. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: Adherance, effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004. 43:559–567.
5. Chou WJ, Chou MC, Tzang RF, Hsu YC, Gau SS, Chen SJ, et al. Better efficacy for the osmotic release oral system methylphenidate among poor adherents to immediate-release methylphenidate in the three ADHD subtypes. Psychiatry Clin Neurosci. 2009. 63:167–175.
6. Cormier E. ADHD: A review and update. J Pediatr Nurs. 2008. 23:345–357.
7. Gau SS, Shen HY, Chou MC, Tang CS, Chiu YN, Gau CS. Determinants of adherence to methylphenidate and the impact of poor adherence on maternal and family measures. J Child Adolesc Psychopharmacol. 2006. 16:286–297.
8. Groenewald C, Emond A, Sayal K. Recognition and referral of girls with ADHD: Case vignette study. Child Care Health Dev. 2009. 35:767–772.
9. Hwang JH. An analysis of the effects of enneagram program for parent on communication style, child-rearing attitude, and self-esteem. 2008. Daegu: Yeungnam University;Unpublished doctoral dissertation.

10. Jackson D, Peters K. Use of drug therapy in children with attention deficit hyperactivity disorder. J Clin Nurs. 2008. 17:2725–2732.

11. Jerome L, Gordon M, Hustler P. A comparison of American and Canadian teachers' knowledge and attitudes towards ADHD. Can J Psychiatry. 1994. 39:563–567.

12. Johnston C, Hommersen P, Seipp C. Acceptability of behavioral and pharmacological treatments for attention-deficit/hyperactivity disorder: Relations to child and parent characteristics. Behav Ther. 2008. 39:22–32.

13. Krain AL, Kendall PC, Power TJ. The role of treatment acceptability in the initiation of treatment for ADHD. J Atten Disord. 2005. 9:425–434.

14. Lee YH, Song JY. A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991. 10:98–113.

15. Leslie LK, Plemmons D, Monn AR, Palinkas LA. Investigating ADHD treatment trajectories: Listening to families' stories about medication use. J Dev Behav Pediatr. 2007. 28:179–188.
16. Letourneau NL, Tramonte L, Willms JD. Maternal depression, family functioning and children's longitudinal development. J Pediatr Nurs. 2012. 31:1–12.
17. Nam HA, Yang S. Parenting stress and parenting role stress in parents of primary school students. J Korean Acad Psychiatr Ment Health Nurs. 2005. 14:323–334.
18. Oh HY, Kim S, Kim JS. Knowledge and attitudes of school nurses to ADHD. J Korean Acad Child Health Nurs. 2008. 14:243–251.
19. Oh KJ, Lee HR. Assessment of ADHD with abbreviated conners rating scale. Korean J Clin Psychol. 1989. 8:69–81.

20. Oh WO, Park ES. Parenting experiences of parents of children with ADHD: Approaching the normal. J Korean Acad Nurs. 2007. 37:91–104.

21. Pham AV, Carlson JS, Kosciulek JF. Ethnic differences in parental beliefs of ADHD and treatment. J Atten Disord. 2009. 13:584–591.

22. Rogers MA, Wiener J, Marton I, Tannock R. Parental involvement in children's learning: Comparing parents of children with and without ADHD. J Sch Psychol. 2009. 47:167–185.

23. Seo MJ, Chang EJ, Jung CH, Chei SY. The study of the parenting stress, depression and parenting efficacy on the mother of attention deficit hyperactivity disorder children. Korean J Woman Psychol. 2003. 8:69–81.
24. Shin SJ. Effects od stress, social support and efficacy on mother's parenting behaviors. 1997. Seoul: Yonsei University;Unpublished doctoral dissertation.
25. Szobot CM, Ketzer MA, Parente J, Biederman J, Rohde LA. The acute effect of methylphenidate in Brazilian male children and adolescents with ADHD: A randomized clinical trial. J Atten Disord. 2004. 8:37–43.

26. Tarnowski JK, Simonian SJ. Assessing treatment acceptance: The abbreviated acceptability rating profile. J Behav Ther Exp Psychiatry. 1992. 23:101–106.

27. Trostl JA. Gochman DS, editor. The history and meaning of patient compliance as an ideology. Handbook of health behavior research. 1997. New York: Plenum Press.

28. Yang J, Yoon BM, Lee MS, Joe SH, Jung IK, Kim SH. Adherence with electronic monitoring and symptoms in children with ADHD. Psychiatry Investig. 2012. 9:263–268.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download