Abstract
Purpose
The purpose of the study was to investigate the psychological factors such as eating psychopathology, depression, obsessive-compulsion, sleep problem, and stressors that affect the alcohol problems in patients with eating disorders.
Methods
Patients with eating disorders (n=347) who visited "M" clinic for eating disorder were participated in the study. Data were collected from February 2008 to May 2010 using Eating Disorder Inventory-2, Beck Depression Inventory, Maudsley Obsessional-Compulsive Inventory, and Alcohol Use Disorder Identification Test-Korean.
Results
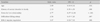
Of the participants, 17.3% had an alcohol problem, 9.2% of them were diagnosed with alcohol dependency. Age, history of mental disorder in family, stress for love relationship, difficulties falling asleep, and 'impulse regulation' (one of eating psychopathologies) were significant associated factors of alcohol problem, but depression and obsessive-compulsion were not significant.
Conclusion
Future interventions for patients with eating disorders should focus on assessing alcohol problems. Assessment should be non-judgmental, especially for those patients with high levels of impulse dysregulation, difficulties falling asleep, and stress in love relationship in order to prevent their early drop-out for the treatment. Alternative treatment for sleep problem and stress management also may be helpful for the patients with alcohol problem and eating disorders.
Figures and Tables
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author;1994.
2. Andrews MM, Meda SA, Thomas AD, Potenza MN, Krystal JH, Worhunsky P, et al. Individuals family history positive for alcoholism show functional magnetic resonance imaging differences in reward sensitivity that are related to impulsivity factors. Biol Psychiatry. 2011; 69:675–683.

3. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test (AUDIT): Guidelines for use in primary care. 2nd ed. Geneva, Switzerland: World Health Organization;2001.
4. Beck AT, Steer RA, Brown GK. BDI-II manual. 2nd ed. San Antonio: The Psychological Corporation;1996.
5. Castro-Fornieles J, Díaz R, Goti J, Calvo R, Gonzalez L, Serrano L, et al. Prevalence and factors related to substance use among adolescents with eating disorders. Eur Addict Res. 2010; 16(2):61–68.

6. Cho DK. The study of objective measurement for obsessional-compulsive behavior: The standardization of the list of obsessional-compulsive behavior in Maudsley obsessional-compulsive inventory. Seoul Univ Stud Rev. 1985; 20:78–90.
7. Cho SH, Cho AR. Personality characteristics of college women group with bulimic and alcohol abuse problem: Based on individual differences in sensitivity of BAS (behavioral activation system)/BIS (behavioral inhibition system). Korean J Health Psychol. 2008; 13(1):57–72.
8. Cooper SE. Chemical dependency and eating disorders: Are they really so different? J Couns Devel. 1989; 68(1):102–105.

9. Courbasson CM, Smith PD, Cleland PA. Substance use disorders, anorexia, bulimia and concurrent disorders. Can J Public Health. 2005; 96:102–106.

10. Duncan AE, Neuman RJ, Kramer JR, Kuperman S, Hesselbrock VM, Bucholz KK. Lifetime psychiatric comorbidity of alcohol dependence and bulimia nervosa in women. Drug Alcohol Depend. 2006; 84:122–132.

11. Garner DM. Eating disorders inventory II. Odessa, FL: Psychological Assessment Resources;1991.
12. Gendall KA, Sullivan PF, Joyce PR, Fear JL, Bulik CM. Psychopathology and personality of young women who experience food cravings. Addict Behav. 1997; 22:545–555.

13. Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010; 33:339–355.

14. Grilo CM, Becker DF, Levy KN, Walker ML, Edell WS, McGlashan TH. Eating disorders with and without substance use disorders: A comparative study of inpatients. Compr Psychiatry. 1995; 36:312–317.

15. Herzog DB, Franko DL, Dorer DJ, Keel PK, Jackson S, Manzo MP. Drug abuse in women with eating disorders. Int J Eat Disord. 2006; 39:364–368.

17. Huas C, Godart N, Foulon C, Pham-Scottez A, Divac S, Fedorowicz V, et al. Predictors of dropout from inpatient treatment for anorexia nervosa: Data from a large French sample. Psychiatry Res. 2011; 185:421–426.

18. Jeong SJ. The effect of impulsiveness and social support on binge eating and drinking problem: The mediation of difficulties in emotional regulation. Kyungnam: Gyeongsang National University;2010. Unpublished master's thesis.
19. Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003; 60:929–937.

20. Keski-Rahkonen A, Sihvola E, Raevuori A, Kaukoranta J, Bulik CM, Hoek HW, et al. Reliability of self-reported eating disorders: Optimizing population screening. Int J Eat Disord. 2006; 39:754–762.

21. Kim MS, Lee IS, Lee CS. The validation study I of Korean BDI-II: In female university students sample. Korean J Clin Psychol. 2007; 26:997–1014.
22. Kim YS. A epidemiological study on the prevalence of alcohol use disorders among the Korean adult population. Korean J Soc Welf. 1999; 37(4):67–88.
23. Lyle RM. Translation of eating disorders inventory II-Korean. Odessa, FL: Psychological Assessment Resources;1996.
24. Ohayon MM, Bader G. Prevalence and correlates of insomnia in the Swedish population aged 19-75 years. Sleep Med. 2010; 11:980–986.

26. Stock SL, Goldberg E, Corbett S, Katzman DK. Substance use in female adolescents with eating disorders. J Adolesc Health. 2002; 31:176–182.

28. Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Boston: Allyn & Bacon;2001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download