Abstract
Objectives
People at ultra-high risk for psychosis have heterogenous character and different long-term outcomes. We divided ultra-high risk subjects into two subgroups by presence of familial history and tried to find different pattern of functional connectivity of the default mode network (DMN) between the two groups in order to examine the effects familial loading.
Methods
Eleven subjects at clinical-high risk (CHR) group with familial history of psychiatric illness and nineteen subjects of CHR group without familial history were recruited. All the subjects were scanned using resting-state functional magnetic resonance imaging. A posterior cingulate cortex was the seed region of the analysis, and the DMN of the both high risk group were analyzed with voxel-wise two sample T test.
Results
The CHR group with familial history showed greater functional connectivity in the precuneus area in contrast with the other high risk subjects (peak-level t=5.49, p<0.001). There were no significant differences in total score on the Positive and Negative Syndrome Scale and Scales of Psychosis-risk Syndrome between the two groups.
Figures and Tables
 | Fig. 1(A) Glass brain and (B) axial section view for the brain areas in which clinical high risk group with familial history showed significantly increased functional connectivity than clinical high risk group without familial history. |
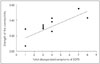 | Fig. 2Positive correlation between disorganized SOPS score and functional connectivity between the PCC seed region and precuneus area in the clinical high risk group with familial history. r=0.739, p=0.009. SOPS : Scales of Psychosis-risk Syndrome, PCC : posterior cingulate cortex. |
Table 1
Demographic and clinical variables of subjects

Data are presented as mean±SD unless otherwise indicated. *: Mann-Whitey test, †: Chi-square test. CHR-F : clinical high risk group with familial history, CHR-NF : clinical high risk group without familial history, M/F : Male/Female, R/L : Right/Left, IQ : intelligence quotient, SOPS : Scale of Prodromal Symptoms, PANSS : Positive and Negative Syndrome Scale, HAM-D : Hamilton Rating Scale for Depression, HAM-A : Hamilton Rating Scale for Anxiety
References
1. Sadock BJ, Kaplan HI, Sadock VA. Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical psychiatry. 2007. 10th ed. Philadelphia: Wolter Kluwer/Lippincott Williams & Wilkins.
2. Kim E, Woo JM, Kwon JS. Cost of Relapse in Patients with Schizohphrenia in Korea. Korean J Psychopharmacol. 2011. 22:29–33.
3. McGue M, Gottesman II, Rao DC. The analysis of schizophrenia family data. Behav Genet. 1986. 16:75–87.

4. Gottesman II, Shields J. A critical review of recent adoption, twin, and family studies of schizophrenia: behavioral genetics perspectives. Schizophr Bull. 1976. 2:360–401.

5. Eaton WW. Epidemiology of schizophrenia. Epidemiol Rev. 1985. 7:105–126.
6. Gottesman II, Bertelsen A. Confirming unexpressed genotypes for schizophrenia. Risks in the offspring of Fischer's Danish identical and fraternal discordant twins. Arch Gen Psychiatry. 1989. 46:867–872.
7. Nicodemus KK, Marenco S, Batten AJ, Vakkalanka R, Egan MF, Straub RE, et al. Serious obstetric complications interact with hypoxia-regulated/vascular-expression genes to influence schizophrenia risk. Mol Psychiatry. 2008. 13:873–877.

8. Gejman PV, Sanders AR, Kendler KS. Genetics of schizophrenia: new findings and challenges. Annu Rev Genomics Hum Genet. 2011. 12:121–144.

9. McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999. 46:899–907.

10. Drake RJ, Haley CJ, Akhtar S, Lewis SW. Causes and consequences of duration of untreated psychosis in schizophrenia. Br J Psychiatry. 2000. 177:511–515.

11. Larsen TK, Moe LC, Vibe-Hansen L, Johannessen JO. Premorbid functioning versus duration of untreated psychosis in 1 year outcome in first-episode psychosis. Schizophr Res. 2000. 45:1–9.

12. Melle I, Larsen TK, Haahr U, Friis S, Johannessen JO, Opjordsmoen S, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004. 61:143–150.

13. McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008. 7:148–156.

14. International Early Psychosis Association Writing Group. International clinical practice guidelines for early psychosis. Br J Psychiatry Suppl. 2005. 48:s120–s124.
15. McGorry PD, Yung AR, Phillips LJ. The "close-in" or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003. 29:771–790.

16. Keith SJ, Matthews SM. The diagnosis of schizophrenia: a review of onset and duration issues. Schizophr Bull. 1991. 17:51–67.

17. Cornblatt B, Lencz T, Obuchowski M. The schizophrenia prodrome: treatment and high-risk perspectives. Schizophr Res. 2002. 54:177–186.

18. Yung AR, McGorry PD. Is pre-psychotic intervention realistic in schizophrenia and related disorders? Aust N Z J Psychiatry. 1997. 31:799–805.

19. Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull. 1996. 22:283–303.

20. Kwon JS, Shim GS, Park HY, Jang JH. Current concept of prodrome from the experience of the Seoul Youth Clinic high risk cohort in Korea. Clin Neuropsychiatry. 2010. 7:56–62.
21. Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003. 29:703–715.

22. Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk ("prodromal") group. Schizophr Res. 2003. 60:21–32.

23. Woods SW, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009. 35:894–908.

24. Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010. 67:241–251.

25. Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with'at-risk mental states'. Schizophr Res. 2004. 71:227–237.

26. Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008. 65:28–37.

27. Schlosser DA, Jacobson S, Chen Q, Sugar CA, Niendam TA, Li G, et al. Recovery From an At-Risk State: Clinical and Functional Outcomes of Putatively Prodromal Youth Who Do Not Develop Psychosis. Schizophr Bull. 2012. 38:1225–1233.

28. Simon AE, Umbricht D. High remission rates from an initial ultra-high risk state for psychosis. Schizophr Res. 2010. 116:168–172.

29. Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011. 168:800–805.

30. Simon AE, Velthorst E, Nieman DH, Linszen D, Umbricht D, de Haan L. Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophr Res. 2011. 132:8–17.

31. Fornito A, Yung AR, Wood SJ, Phillips LJ, Nelson B, Cotton S, et al. Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol Psychiatry. 2008. 64:758–765.

32. Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ, et al. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet. 2003. 361:281–288.

33. Fusar-Poli P, Perez J, Broome M, Borgwardt S, Placentino A, Caverzasi E, et al. Neurofunctional correlates of vulnerability to psychosis: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2007. 31:465–484.

34. Shin KS, Kim JS, Kang DH, Koh Y, Choi JS, O'Donnell BF, et al. Pre-attentive auditory processing in ultra-high-risk for schizophrenia with magnetoencephalography. Biol Psychiatry. 2009. 65:1071–1078.

35. Armando M, Girardi P, Vicari S, Menghini D, Digilio MC, Pontillo M, et al. Adolescents at ultra-high risk for psychosis with and without 22q11 deletion syndrome: A comparison of prodromal psychotic symptoms and general functioning. Schizophr Res. 2012. 139:151–156.

36. Greenwood TA, Braff DL, Light GA, Cadenhead KS, Calkins ME, Dobie DJ, et al. Initial heritability analyses of endophenotypic measures for schizophrenia: the consortium on the genetics of schizophrenia. Arch Gen Psychiatry. 2007. 64:1242–1250.

37. Reitz C, Mayeux R. Endophenotypes in normal brain morphology and Alzheimer's disease: a review. Neuroscience. 2009. 164:174–190.

38. Brotman MA, Guyer AE, Lawson ES, Horsey SE, Rich BA, Dickstein DP, et al. Facial emotion labeling deficits in children and adolescents at risk for bipolar disorder. Am J Psychiatry. 2008. 165:385–389.

39. Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. 2007. 8:700–711.

40. Gusnard DA, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001. 2:685–694.

41. Fransson P. Spontaneous low-frequency BOLD signal fluctuations: an fMRI investigation of the resting-state default mode of brain function hypothesis. Hum Brain Mapp. 2005. 26:15–29.

42. Shim G, Oh JS, Jung WH, Jang JH, Choi CH, Kim E, et al. Altered resting-state connectivity in subjects at ultra-high risk for psychosis: an fMRI study. Behav Brain Funct. 2010. 6:58.

43. Zhou Y, Liang M, Tian L, Wang K, Hao Y, Liu H, et al. Functional disintegration in paranoid schizophrenia using resting-state fMRI. Schizophr Res. 2007. 97:194–205.

44. Garrity AG, Pearlson GD, McKiernan K, Lloyd D, Kiehl KA, Calhoun VD. Aberrant "default mode" functional connectivity in schizophrenia. Am J Psychiatry. 2007. 164:450–457.

45. Pomarol-Clotet E, Salvador R, Sarro S, Gomar J, Vila F, Martinez A, et al. Failure to deactivate in the prefrontal cortex in schizophrenia: dysfunction of the default mode network? Psychol Med. 2008. 38:1185–1193.

46. Meyer-Lindenberg AS, Olsen RK, Kohn PD, Brown T, Egan MF, Weinberger DR, et al. Regionally specific disturbance of dorsolateral prefrontal-hippocampal functional connectivity in schizophrenia. Arch Gen Psychiatry. 2005. 62:379–386.

47. Camchong J, MacDonald AW 3rd, Bell C, Mueller BA, Lim KO. Altered functional and anatomical connectivity in schizophrenia. Schizophr Bull. 2011. 37:640–650.

48. Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012. 8:49–76.

49. Whitfield-Gabrieli S, Thermenos HW, Milanovic S, Tsuang MT, Faraone SV, McCarley RW, et al. Hyperactivity and hyperconnectivity of the default network in schizophrenia and in first-degree relatives of persons with schizophrenia. Proc Natl Acad Sci U S A. 2009. 106:1279–1284.

50. Liu H, Kaneko Y, Ouyang X, Li L, Hao Y, Chen EY, et al. Schizophrenic patients and their unaffected siblings share increased resting-state connectivity in the task-negative network but not its anticorrelated task-positive network. Schizophr Bull. 2012. 38:285–294.

51. Ziermans TB, Schothorst PF, Schnack HG, Koolschijn PC, Kahn RS, van Engeland H, et al. Progressive structural brain changes during development of psychosis. Schizophr Bull. 2012. 38:519–530.

52. Glahn DC, Winkler AM, Kochunov P, Almasy L, Duggirala R, Carless MA, et al. Genetic control over the resting brain. Proc Natl Acad Sci U S A. 2010. 107:1223–1228.

53. Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJ. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009. 33:279–296.

54. Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007. 62:429–437.

55. Zhao XH, Wang PJ, Li CB, Hu ZH, Xi Q, Wu WY, et al. Altered default mode network activity in patient with anxiety disorders: an fMRI study. Eur J Radiol. 2007. 63:373–378.

56. Chung YS, Kang DH, Shin NY, Yoo SY, Kwon JS. Deficit of theory of mind in individuals at ultra-high-risk for schizophrenia. Schizophr Res. 2008. 99:111–118.

57. Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005. 39:964–971.

58. Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage. 2002. 15:273–289.

59. Bluhm RL, Miller J, Lanius RA, Osuch EA, Boksman K, Neufeld RW, et al. Spontaneous low-frequency fluctuations in the BOLD signal in schizophrenic patients: anomalies in the default network. Schizophr Bull. 2007. 33:1004–1012.

60. Castellanos FX, Margulies DS, Kelly C, Uddin LQ, Ghaffari M, Kirsch A, et al. Cingulate-precuneus interactions: a new locus of dysfunction in adult attention-deficit/hyperactivity disorder. Biol Psychiatry. 2008. 63:332–337.

61. Kjaer TW, Nowak M, Lou HC. Reflective Self-Awareness and Conscious States: PET Evidence for a Common Midline Parietofrontal Core. Neuro Image. 2002. 17:1080–1086.

62. Lou HC, Luber B, Crupain M, Keenan JP, Nowak M, Kjaer TW, et al. Parietal cortex and representation of the mental Self. Proc Natl Acad Sci U S A. 2004. 101:6827–6832.

63. Fransson P, Marrelec G. The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: Evidence from a partial correlation network analysis. Neuro Image. 2008. 42:1178–1184.

64. Calhoun VD, Sui J, Kiehl K, Turner J, Allen E, Pearlson G. Exploring the psychosis functional connectome: aberrant intrinsic networks in schizophrenia and bipolar disorder. Front Psychiatry. 2011. 2:75.

65. Bleuler E. [Dementia praecox or the group of schizophrenias]. Vertex. 2010. 21:394–400.
66. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders I Mania and schizophrenia. Arch Gen Psychiatry. 1987. 44:13–20.
67. Kerns JG, Berenbaum H. Cognitive impairments associated with formal thought disorder in people with schizophrenia. J Abnorm Psychol. 2002. 111:211–224.

68. van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull. 2008. 34:1066–1082.

69. Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003. 160:636–645.

70. Schulze TG, Akula N, Breuer R, Steele J, Nalls MA, Singleton AB, et al. Molecular genetic overlap in bipolar disorder, schizophrenia, and major depressive disorder. World J Biol Psychiatry. 2012.

71. Lichtenstein P, Yip BH, Bjork C, Pawitan Y, Cannon TD, Sullivan PF, et al. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet. 2009. 373:234–239.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download