Abstract
Background
An automated immunohematology analyzer, DAYMATE M (DAY Medical, Switzerland), has been recently developed. The potential of this analyzer to improve test results has been evaluated.
Methods
A total of 300 blood samples from Seoul St. Mary's hospital and Incheon St. Mary's hospital were tested for ABO and RhD typing. In addition, 336 antibody screening test (AST) samples and 82 patients treated with hematopoietic stem cell transplantation (HSCT) were included. AST results by DAYMATE M were compared with those obtained by a manual method using DS-Screening II (Bio-Rad Laboratories, Switzerland) and red blood cells from Selectogen (Ortho-Clinical diagnostics Inc., USA).
Results
Of the 300 patients enrolled, 87, 73, 79, and 61 had type A, B, O, and AB blood, respectively. The concordance rate was 99.9% for cell typing and 97.0% for serum typing. One discordant case was classified as type B instead of AB, and six discordant serum-typing cases were type A, but classified as type AB. Among the 336 AST samples, the concordance rate was 93.2%. From 136 positive cases, six were discordant. Within the 82 HSCT-treated patients, the concordance rate for ABO blood typing was 92.2%. Among the six discordant cases, DAYMATE M typed four cases as donor type where the standard method typed them as the recipient blood type.
Pre-transfusion compatibility testing is crucial to the transfusion process. Before red blood cell (RBC) transfusion, blood samples from donors and recipients are analyzed to determine their ABO and RhD blood typing, to look for unexpected RBC alloantibodies, and to confirm cross-match compatibility [1]. These tests are crucial for preventing transfusion of incompatible donor red cells that might cause a hemolytic reaction.
Manual immunohematology testing has been performed by centrifuging RBCs and antibodies in test tubes, followed by a visual determination of the extent of RBC agglutination. Although the manual method is still considered the gold standard, this technique has inherent limitations. These include the elution of low affinity antibodies during washing, the variability in results due to differences in the cell-serum ratio, and the inconsistency in reporting due to inter-observer variability [2]. The results observed in blood bank testing are more critical than in other laboratories because an operator error can result in a fatal outcome immediately after transfusion [3].
Many efforts have been made to automate the pre-transfusion test, and a number of automated instruments have been developed and marketed recently. Automation in blood bank serology applications was introduced in developed countries in the 1960s [4]. Column agglutination technology (CAT) and solid-phase RBC adherence assays overcome some deficiencies of the standard manual method [567]. These methods have been commercialized as automated or semi-automated workstations. Transfusion services with a small workload may often prefer a semi-automated, rather than fully automated, system. However, it must be realized that although the number of steps may be reduced, there is still a substantial amount of manual input required in semi-automated systems [8]. Nevertheless, there is improvement in the objectivity and reproducibility of results, as well as the time taken to perform certain tests [9]. The major limitation that remains with semi-automated systems is that there are fewer safety features available compared to those available in fully automated systems and thus there is a greater possibility for human errors due to the manual steps involved, including sample labeling, diluting, reagent addition, and result interpretation [2].
For transfusion centers with a high workload, a fully automated system is required. Automation improves the quality of testing by improving objectivity and reproducibility while decreasing human errors and making storage of immunohematology test results more convenient. In addition, automation has reduced the manual input required for various serology tests and, thus, has improved laboratory efficiency. High-throughput devices with less turnaround time improve the quality of services in large tertiary care settings [2]. For these reasons, automation in blood banks is being adopted by more and more centers and is rapidly becoming a standard test in many countries [10]. The core limitation for automated pre-transfusion testing is cost, which usually requires a large initial investment. Moreover imprecision is still present, including a high degree of inter-observer variability and significant inter-institutional variation [11].
The purpose of validation is to test the competence of an automated system. It is important to ensure compliance with accuracy and safety standards as well as to obtain knowledge regarding equipment maintenance and calibration [2]. In this study, we evaluated a new automated pre-transfusion testing instrument, the DAYMATE M (DAY MEDICAL, Avenches, Switzerland) by comparing its results to those of the standard manual process.
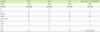
This was a multi-center, prospective study at Seoul St. Mary's hospital and Incheon St. Mary's hospital from March to August 2016. Patients from Seoul St. Mary's hospital and Incheon St. Mary's hospital were enrolled after approval from their respective institutional review boards. In total, 108 and 192 EDTA-treated blood and serum samples were collected from Seoul and Incheon St. Mary's hospitals, respectively (Table 1). Additionally, 244 and 132 samples were collected for the antibody screening test (AST) from Seoul and Incheon St. Mary's hospitals, respectively, while 82 samples from patients who received hematopoietic stem cell transplantation (HSCT) were collected from Seoul St. Mary's hospital (Table 1). CLSI guideline I/LA33-A and ISBT guidelines for validation of automated systems were used [1213].
Bioscot anti-A, anti-B, and anti-RhD (IgM/IgG) reagents (Merck Millipore, Darmstadt, Germany) were employed for manual testing using the plate method. AST by DAYMATE M was compared to the manual method using DS-Screening II (Bio-Rad Laboratories, Cressier, FR, Switzerland) and red blood cells from Selectogen (Ortho-Clinical diagnostics Inc., Raritan, NJ, USA). The automated immunohematology analyzer DAYMATE M utilized a column method, and gel was automatically injected into empty columns before each test. For AST, three kinds of cells were utilized. The reagents used were as follows: DAY anti-A, anti-B, and anti-D for cell typing of ABO and RhD; DAY cell A1 and B for serum typing; and DAY cell I, II, and III for AST. The manual method was regarded as the standard method, and the DAYMATE M test was performed at the Laboratory for Development and Evaluation Center in Seoul St. Mary's Hospital.
The automated system DAYMATE M uses solid-phase red cell adherence (SPRCA) assays and other microtiter plate formats. It uses column agglutination on discs with initially empty wells. These wells contain capillaries where column agglutination takes place. After requesting a test, one disc is placed in a centrifuge and remains there until the end of the test. First, the required gel (neutral or AHG) is added to the wells and drawn into the capillaries through centrifugation. The sample to be tested and the appropriate reagent are pipetted into the upper part of the reaction well. The individual reaction wells requiring incubation at 37℃ are automatically heated, while the other reaction wells remain at room temperature. After incubation, erythrocytes are centrifuged through the capillary gel, allowing a clear reaction reading that is identical to the known column agglutination gel test. Test results performed by the DAYMATE M were compared to results obtained using each hospital's standard manual procedures.
A total of 300 samples collected in EDTA tubes were tested. For A, B, O, and AB blood types, there were 87, 73, 79, and 61 samples, respectively; five Rh-negative samples were included. At both hospital sites, the configuration of blood typing reagents and reagent RBCs conformed to conventional formats for serologic testing in transfusion services. Incheon St. Mary's hospital uses ORTHO VISION (Ortho Clinical Diagnostics, Raritan, NJ, USA). For samples from Seoul St. Mary's hospital, forward typing on a plate and reverse typing by tube techniques were tested repeatedly by different operators using standard methods, with results described as negative or positive.
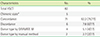
Samples were tested according to an ID card for the AST (Bio-Rad Laboratories). The ID-Card ID-DiaScreen consists of four microtubes containing polyspecific AHG for the indirect antiglobulin tests (IAT) and two microtubes containing neutral gel for the two-stage enzyme technique. The AST confirmed 37 positive cases (Table 2).
Samples from 82 patients treated with HSCT were collected to test the isoagglutinin titer (Table 1). The A blood type donor and blood type recipient was the most frequent group (19.5%, 16/82) and there were no examples of an O blood type donor and AB blood type recipient. The tested results were compared to those of DAYMATE M. The median number of days after HSCT was 23, but ranged from 0 to 799. For eight patients, follow-up titers of anti-A and anti-B, as well as the degree of A cell and B cell agglutination were collected. These titers or degrees of agglutination were compared between the standard method and DAYMATE M. For the standard method, the immediate spin (IS) and AHG tube methods were performed. Both methods were performed as outlined in the American Association of Blood Banks (AABB) Technical Manual [14]. Briefly, for the IS tube method, 10 tubes were labeled for the appropriate dilutions and serial dilutions of 100 µL serum in saline were prepared. Saline-suspended group A or B RBCs (3%) were added to each dilution. After incubation at room temperature (22–25℃) and centrifugation at 1,000 g for 25 sec, test results were determined macroscopically by two medical technicians and two laboratory physicians. The titer endpoint was the reciprocal of the highest dilution yielding weak agglutination. For the AHG tube method, after the IS tube test, the tubes were incubated at 37℃ for 30 min and washed three times using normal saline. After adding 100 µL of polyspecific AHG (Millipore, Livingston, UK), the tubes were centrifuged at 1,000 g for 15 sec. Test results were interpreted in the same manner as the IS tube method.
The concordance rates for ABO cell typing and serum typing by DAYMATE M were 99.9% (299/300) and 97.0% (294/300), respectively. The overall concordance rate was 97.7% (293/300) (Table 1). One discrepancy in cell typing was from a patient with the AB blood type, but who was typed as B. Six discrepant cases of serum typing involved the type A blood group where DAYMATE M reported no agglutination using B cells to detect anti-B.
The concordance rate was 93.2% (313/336) between the standard method and DAYMATE M for the AST (Table 1). Seven discrepant cases with identification test results are listed in Table 2. Six discrepant cases were falsely typed as having a negative result by DAYMATE M, among 136 positive cases. Among the 17 discrepant cases within the 200 negative cases, all were falsely typed as having a positive result.
A total of 82 samples from patients treated with HSCT were enrolled (Table 1). As both the standard method and DAYMATE M reported five of them as being chimeric, these cases were discarded from the analysis (Table 3). Among 77 cases, 71 revealed concordant and six revealed discordant results when comparing between the standard method and DAYMATE M. Among the six discordant results, four were typed as the donor blood type by DAYMATE M and two by the standard method. This resulted in a concordance rate for ABO typing of 92.2% (71/77) among HSCT patients.
Eight patients with follow-up titer data of anti-A, and anti-B and degree of A cell and B cell agglutination were compared between the standard method and DAYMATE M (Fig. 1). Three of the patients were type A donor with type O recipient, while two of them were type O donor with type B recipient. There was one case each for type B donor with type AB recipient, type AB donor with type B recipient, and type A with type B recipient. Most of these cases revealed that the DAYMATE M titer was higher compared to that of the standard method, but the degree of agglutination by A cell and B cell was higher using the standard method.
The DAYMATE M automatically adds gel to 18 empty test wells and benefits from high flexibility. Moreover, the DAYMATE M requires only seven minutes for incubation and seven minutes for centrifugation, thus reducing sample turnaround time. It is capable of 400 tests per hour and up to 3,000 tests per day. Due to this ease of use, the DAYMATE M greatly reduces the time necessary for both operator training and hands-on operation.
The DAYMATE M yielded reliable results when compared to the standard method, especially for ABO and RhD blood typing tests. These results indicated that the DAYMATE M performed routine blood bank tests with an accuracy rate comparable to the standard manual method typically performed in hospital blood banks. Automation could improve test quality by diminishing pre-analytical, analytical, and post-analytical errors, and this is the main objective of automation in diagnostic blood typing instruments.
For ABO and RhD blood typing, agreement between the DAYMATE M and the reference method was 99.9% for cell typing and 97.0% for serum typing, resulting in an overall accuracy of 97.7%. These results are in line with other automated immunohematology analyzer results, and the overall concordance rate ranged from 99.1% to 100% [41516]. One discrepancy in cell typing was from a patient with the AB blood type, which was typed as B. This patient had chronic obstructive pulmonary disease and did not have any history of transfusion or stem cell transplantation. It is possible that the blood type can be cis-AB or there may have been a problem with the test reagents. Six discrepancies were observed in serum typing, with all cases exhibiting a failure to detect anti-B. Discrepancies in serum typing could be caused by weak RBC antibodies or weak antigens in typical grouping B cell products. The weak serum reaction of DAYMATE M might be due to the concentration difference between red cell reagents. The DAYMATE M uses a 1.6% red cell reagent while the manual method uses 3% red cells. Discrepancies in serum typing have been observed with other automated immunohematology analyzers for pre-transfusion tests [1718]. Even though such weak reactions in ABO and RhD typing might be insignificant findings caused by cold or allo- or auto-antibodies, such discrepancies may lead to increased costs and delays in transfusion because of the repeat testing required for resolution. Weak positive results from instruments should be confirmed by operators using the manual method to avoid controversial results and reduce unnecessary repeat testing. More careful handling of cards during transport or storage should also be considered. CAT is a very sensitive and discriminating method compared to previous manual tube methods; however, false positive results caused by human error persist [7]. Automated instruments are expected to reduce repeated ASTs, delays in transfusions, unnecessary identification tests, and the increased cost of manual methods due to their low reproducibility [3].
ABO and RhD blood typing concordance between DAYMATE M and the standard method among HSCT patients was 92.2%, which was higher than expected. As the blood typing of HSCT patients requires highly trained and experienced personnel to ensure high quality test performance and interpretation, an automated analyzer is required to substitute or support the test. Assessment of samples from the HSCT patients revealed that the isoagglutinin titers of the cell typing performed by the DAYMATE M were higher than those calculated using manual method (Fig. 1). The serum typing revealed higher titers from the manual method, which is in line with previous reports [316]. Additional studies are required to further our understanding of the underlying causes behind these differences.
In conclusion, the DAYMATE M could offer blood testing standardization, objective reading of hemagglutination endpoints, uniform interpretation of serologic reaction patterns, improved documentation of test procedures, and decreased hands-on time for operators. The DAYMATE M exhibited acceptable concordance with the standard method for ABO and RhD blood typing, as well as AST and on samples from patients treated with HSCT.
Figures and Tables
 | Fig. 1Comparison of isoagglutinin titer between Manual method and DAYMATE M among patients with HSCT. The x axis is the standard method titer of anti-A, anti-B, A cell, and B cell performed by manual method. The y axis is titer results by DAYMATE M. The number implies the frequency of tests repeatedly performed during hospital stay. A→O refers to type A donor with type O recipient. |
Table 1
Baseline characteristics and concordance rates between the standard method at Site A and Site B as compared to the automated immunohematology analyzer DAYMATE M

Table 2
AST results by frequency, performed with known identification
References
1. Roback JD, Barclay S, Hillyer CD. An automatable format for accurate immunohematology testing by flow cytometry. Transfusion. 2003; 43:918–927.

2. Bajpai M, Kaur R, Gupta E. Automation in Immunohematology. Asian J Transfus Sci. 2012; 6:140–144.

3. Shin SY, Kwon KC, Koo SH, Park JW, Ko CS, Song JH, et al. Evaluation of two automated instruments for pre-transfusion testing: AutoVue Innova and Techno TwinStation. Korean J Lab Med. 2008; 28:214–220.

4. Sturgeon P, Cedergren B, McQuiston D. Automation of routine bloodtyping procedures. Vox Sang. 1963; 8:438–451.
5. Lapierre Y, Rigal D, Adam J, Josef D, Meyer F, Greber S, et al. The gel test: a new way to detect red cell antigen-antibody reactions. Transfusion. 1990; 30:109–113.

6. Sinor LT. Advances in solid-phase red cell adherence methods and transfusion serology. Transfus Med Rev. 1992; 6:26–31.

7. Voak D. The status of new methods for the detection of red cell agglutination. Transfusion. 1999; 39:1037–1040.

8. Duguid JK, Bromilow IM. New technology in hospital blood banking. J Clin Pathol. 1993; 46:585–588.

9. Casina TS. In search of the Holy Grail: comparison of antibody screening methods. Immunohematology. 2006; 22:196–202.

10. Malomgré W, Neumeister B. Recent and future trends in blood group typing. Anal Bioanal Chem. 2009; 393:1443–1451.

11. Tanabe K. Interinstitutional variation in the measurement of anti-A/B antibodies: the Japanese ABO-Incompatible Transplantation Committee survey. Transplantation. 2007; 84:S13–S16.

12. Validation Task Force of the International Society of Blood Transfusion Working Party on Information Technology. ISBT Guidelines for validation of automated systems in blood establishments. Vox Sang. 2010; 98:1–19.
13. Clinical and Laboratory Standards Institute. Validation of automated systems for immunohematological testing before implementation; approved guidelines. I/LA33-A. Wayne, PA: Clinical and Laboratory Standards Institute;2010.
14. Fung MK, Grossman BJ, editors. Technical manual. 18th ed. Bethesda: American Association of Blood Banks;2014. p. 371–378.
15. Jang MA, Oh JW, Lee ST, Seo JY, Kim DW. Evaluation of the automated blood bank systems Galileo NEO and QWALYS-3 for ABO-RhD typing and antibody screening. Korean J Blood Transfus. 2014; 25:235–242.
16. Park Y, Lim J, Ko Y, Kwon K, Koo S, Kim J. Evaluation of IH-1000 for automated ABO-Rh typing and irregular antibody screening. Korean J Blood Transfus. 2012; 23:127–135.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download