Abstract
Background
The use of the multiplex polymerase chain reaction (PCR) technique for respiratory viruses has become popular in Korea owing to its convenience and sensitivity. However, concerns remain with regard to possible interference due to multiplexing.
Methods
We compared the analytical sensitivity and virus interference of a commercially available, multiplex PCR kit (AdvanSure Respiratory virus real-time PCR kit, LG Life Sciences, Korea) with that of singleplex PCR to detect 11 viruses including coronavirus 229E and OC43; parainfluenza virus 1 (PIV 1), parainfluenza virus 2 (PIV 2), and parainfluenza virus 3 (PIV 3); influenza virus A (INF A) and influenza virus B (INF B); respiratory syncytial virus A (RSV A) and respiratory syncytial virus B (RSV B); adenovirus; and rhinovirus A, B, and C.
Results
The lowest detected viral concentrations of coronavirus 229E and OC43, INF A and B, RSV A and B, adenovirus, and rhinovirus A, B, and C were the same for both, multiplex and singleplex systems. However, the lowest detected viral concentrations of PIV1, 2, and 3 differed by 1 dilution factor between the two systems. Threshold cycle (Ct) values for mixed viruses within the same well were not significantly influenced by each other, where the difference between Ct values ranged from 0.24 to 1.99.
Acute respiratory tract infections are the second-most common cause of premature mortality worldwide [1], with approximately 200 million cases of viral community-acquired pneumonia, annually [2]. Respiratory infections can be caused by any of the 26 respiratory viruses currently known [23]. Several children with respiratory illnesses are diagnosed with viral co-infections with at least 5 concomitant respiratory virus species [3].
Conventional detection methods for respiratory virus infection include virus culture, antigen detection, and serology, which are time-consuming, labor-intensive, and with low sensitivity [4]. These methods yield an overall virus detection rate of <40% in children with lower respiratory illnesses (acute wheezing/asthma and pneumonia) [3].
Various nucleic acid-based amplification technologies have been used to detect respiratory viruses, such as polymerase chain reaction (PCR), nucleic acid sequence-based amplification, transcription-mediated amplification, strand displacement amplification, loop-mediated isothermal amplification, rolling circle amplification, helicase-dependent amplification, and multiplex ligation-dependent probe amplification [4]. Among these, PCR has emerged as the most convenient technology for multiplexing a large number of targets [4]. Molecular methods currently detect one or more respiratory viruses in up to 95% of children with bronchiolitis, acute wheezing, or asthma, and in up to 72% of children with pneumonia [3]. Molecular diagnostic tests have greatly increased our understanding of the role of viruses in pneumonia and findings indicate that the incidence of viral pneumonia has been underestimated [2].
The simultaneous detection of multiple viruses by PCR would be clinically beneficial, because clinical signs and symptoms of respiratory virus infections overlap and are seldom pathognomonic for any specific virus [3]. Recently, multiplexed molecular assays for respiratory viruses have been commercially developed and used largely for routine clinical diagnosis of respiratory tract infection [4]. However, primer dimer formation and competition between multiple targets would hamper the performance of PCR technology.
Recently, an increasing number of comparative studies have been reported, involving commercial versus laboratory-developed assays, or amongst various commercial assays [4]. However, very limited data is available to compare the performance of multiplex PCR with singleplex PCR for the detection of respiratory viruses. In this study, we aim to compare the analytical sensitivity and multiple virus interference of a commercially available, respiratory virus multiplex PCR kit with the singleplex technique.
Commercially available reference strains of 11 respiratory viruses were purchased from Korea Bank for Pathogenic Viruses. Detailed information regarding the 11 species of virus, such as control number and titer, are listed in Table 1. The viruses were 10-fold serially diluted in distilled water for the evaluation of assay sensitivity. Viral concentration was expressed as plaque forming units (PFU)/mL, based on the plaque assay, or converted from the value obtained using the tissue culture infective dose 50 (TCID50) assay which is the measure of infectious virus titer to quantify the amount of virus required to kill 50% of infected host or to produce a cytopathic effect in 50% of inoculated tissue culture cells.
Nucleic acid of each diluted reference virus strain was extracted using ExiPrep Viral DNA/RNA Kit (Bioneer, Daejeon, Korea) according to the manufacturer's instructions. Multiplex PCR was performed using AdvanSure™ RV real-time PCR kit (LG Life Science, Seoul, Korea) according to the manufacturer's instructions. For the same target viruses, singleplex PCR kits were developed using the same primer and probe sets obtained from the same manufacturer. All samples were tested in duplicate and were retested if the difference in threshold cycle (Ct) value between duplicates exceeded 1.0 to exclude random error. Positive and negative controls were tested as batch controls.
Each virus sample was 10-fold serially diluted with distilled water (1-10-8). Assay sensitivity was defined as the lowest virus concentration detected by each assay. A Ct difference of >2.0 between multiplex and singleplex PCR was regarded to be significant based on the imprecision of multiplex PCR reagents, per the manufacturer's instructions (data not shown).
The multiplex kit was designed to test three viruses within a single well (Table 2). For the evaluation of interference, the target virus sample was prepared at a concentration 10-fold higher than the limit of detection (LOD), mixed with serially diluted, possibly interfering virus within a single well, and multiplexed. Commercially available positive and negative controls included in the multiplex kit were tested as batch quality controls. If the control results exceeded the predefined limit, all samples of that batch were tested again. A Ct difference >2.0, per the concentration of interfering viruses, was regarded as significant.
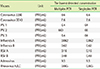
Multiplex and singleplex PCR results showed the same analytical sensitivity level for 8 viruses: coronavirus 229E and OC43, influenza virus (INF) A and B, respiratory syncytial virus (RSV) A and B, adenovirus, and rhinovirus A, B, and C (Table 3). However, multiplex PCR showed higher sensitivity for parainfluenza virus (PIV) 1 and 3 (the lowest detected viral concentration of both viruses was 6.4 PFU/mL using multiplex versus 6.4×10 PFU/mL using singleplex), and lower sensitivity for PIV2 (6.6×102 PFU/mL using multiplex versus 6.6×10 PFU/mL using singleplex), but the difference was within 1 dilution factor (Table 3).
Except for coronavirus OC43, RSV A and rhinovirus A, B, and C, the difference in Ct value between multiplex and singleplex assays was < 2.0 for all dilutions of each virus (mean±standard deviation [SD], -0.40±1.28). Ct values for coronavirus OC43 and RSV A using multiplex PCR were lower than those using singleplex PCR at certain low concentrations, while Ct values for rhinovirus A, B, and C using multiplex PCR were higher than those using singleplex PCR (Fig. 1).
Ct values for viruses mixed in a single well were not significantly influenced by each other, where the difference between Ct values ranged from 0.24 to 1.99 (Fig. 2).
As a DNA amplification technique, PCR drives modern genomics, forensics, and medical diagnostics. However, the PCR technique is still not necessarily easy to perform or without complications [5]. Due to its high sensitivity, PCR is highly prone to contamination and off-target effects.
In multiplex PCR, two or more loci are simultaneously amplified in the same reaction [6]. By reducing the number of PCR reactions in an experiment, it can conserve expensive reagents and DNA samples [67]. However, multiplex PCR is more prone to contamination, because multiple targets (usually between two and five) are detected simultaneously in the same tube [5]. If one target requires three primers, none of which should be able to bind elsewhere in the template DNA or to each other, then two targets require six, three require nine, and so on. Each amplicon must either be a different size (for gels) or be labeled with a spectrally distinct fluorescent dye. Complicating matters is that different targets in the reaction can compete with each other for resources. If highly abundant templates are detected, the less abundant ones fade into the background [5]. Therefore, considerable time and effort is required for optimization and validation of multiplex PCR.
Our study results show that multiplex real-time PCR assays developed recently exhibited high performance compared with singleplex PCR and there was no interference between targets in multiplex PCR. Very few reports are available that compare singleplex and multiplex PCR. A study conducted in 2000, regarding fragment size differences between multiplex and singleplex PCR products, reported that for one marker, the fragment sizes of the products obtained from multiplex PCR were all approximately 2 bp larger than those obtained from singleplex PCR [6]. The authors concluded that primer-primer interaction within the multiplex PCR system may have resulted in this genotyping error [6]. On the contrary, Wang et al. [8] reported the clinical validation of multiplex real-time PCR assays for detection of bacterial meningitis pathogens in 2011 and showed that differences between Ct values and respective SD were similar between the multiplex and singleplex systems, indicating similar extent of measurement error. Additionally, there was no significant difference in sensitivity and specificity between the multiplex and singleplex real-time PCR assays [8]. Another previous study comparing the Luminex xTAG respiratory virus panel with real-time reverse-transcriptase PCR developed by the Centre for Disease Control, USA, for INF A showed that although 0.7% clinical samples showed discordant results, this was due not to multiplexing but to the different formats of the two assays [9].
To the best of our knowledge, no standard cutoff has been established to designate a difference in Ct value between 2 qualitative methods as significant. Therefore, a difference of >2.0 between Ct values using multiplex and singleplex PCR was regarded as significant in this study, based on the imprecision of multiplex PCR reagents, per the manufacturer's instructions (data not shown). The mean SD of Ct for all respiratory viruses across all concentrations studied was 0.8±0.4. Therefore, the value of 2.0 (2×SD) was used as a decisional cutoff. If the primer is 100% efficient, theoretically, a Ct difference of 1 indicates that one sample contains twice as much of the template as the other. Using qualitative PCR for virus detection, <2 times the quantity has little effect on the results. We used the same cutoff for difference in Ct value, to designate significant interference as that used for sensitivity. All results in this study showed Ct difference of <2, suggesting that there was no interference of counterpart viruses.
The tests analyzed in this study are qualitative; therefore, we could not evaluate the LOD using the method employed for quantitative tests. Rather, we used the 10-fold dilution method to presume the approximate lowest concentration detectable. Even though the assay sensitivity for PIV between multiplex and singleplex assays seemed to differ, this difference was within 1 dilution factor. This difference could be due either to an error during dilution or to the difference between the multiplex and singleplex procedures.
There were some limitations in our study. First, we could evaluate only real-time multiplexing PCR format for respiratory tract infections, although there are many other multi-parametric, molecular diagnostic platforms such as microassay, PCR-mass spectrometry, PCR-electrochemical detection, and Luminex platforms [10]. Second, the singleplex PCR assay kit used in this study was obtained from the same manufacturer as a reagent for research use (not an approved in vitro diagnostics), although the singleplex kit was made using the same manufacturing process and the same primer sets were used, as in the multiplex PCR kit. Third, we used standard virus strains rather than clinical samples. Components of clinical specimens can interfere with PCR, so further study is required using clinical specimens. Lastly, we did not evaluate coronavirus NL63, metapneumovirus, and bocavirus, which were included in the multiplex kit, because of lack of standardized viral materials.
In conclusion, analytical sensitivity of multiplex PCR for respiratory viruses was comparable to singleplex PCR. Interference by other viruses present in the same reaction well, which is a concern while performing multiplex PCR, was not observed in this study. However, it is crucial to validate and verify the performance of multiplex PCR reagents by manufacturer during producing the reagents.
Figures and Tables
Fig. 1
Threshold cycle (Ct) values of multiplex PCR and singleplex PCR for each respiratory virus. *Ct difference between multiplex PCR and singleplex PCR > 2.

Fig. 2
Ct values for 11 respiratory viruses mixed in the same reaction well with other respiratory virus of decreasing concentration.

Table 1
Information for 11 reference strains of respiratory viruses

When titer as PFU/mL based on the TCID50 assay was available, these titers were used as base concentrations. The concentrations of all viruses except two (RSV A and RSV B) were converted from the values based on TCID50 assay. The concentrations of RSV A and RSV B were based on the plaque assay.
Abbreviations: NA, not available; PIV, parainfluenza virus; RSV, respiratory syncytial virus.
Table 2
Target compositions of wells in the AdvanSure multiplex PCR kit
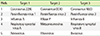
Table 3
Lowest detected concentration for each virus in multiplex and singleplex PCR
Notes
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST No potential conflicts of interest relevant to this article were reported.
This article is available from http://www.labmedonline.org
References
1. World Health Organization. World Health Statistics 2014. Geneva: World Health Organization;2014.
3. Jartti T, Soderlund-Venermo M, Hedman K, Ruuskanen O, Makela MJ. New molecular virus detection methods and their clinical value in lower respiratory tract infections in children. Paediatr Respir Rev. 2013; 14:38–45.

4. Vallieres E. Clinical and economical impact of multiplex respiratory virus assays. Diagn Microbiol Infect Dis. 2013; 76:255–261.

5. Perkel J. Overcoming the Challenges of Multiplex PCR. http://www.biocompare.com/Editorial-Articles/117895-Multiplex-PCR/.
6. Deng HW, Zhou Y, Recker RR, Johnson ML, Li J. Fragment size difference between multiplex and singleplex PCR products and their practical implications. Biotechniques. 2000; 29:298–304.

7. Burgart LJ, Robinson RA, Heller MJ, Wilke WW, Iakoubova OK, Cheville JC. Multiplex polymerase chain reaction. Mod Pathol. 1992; 5:320–323.
8. Wang X, Theodore MJ, Mair R, Trujillo-Lopez E, du Plessis M, Wolter N, et al. Clinical validation of multiplex real-time PCR assays for detection of bacterial meningitis pathogens. J Clin Microbiol. 2012; 50:702–708.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download