Abstract
Eggerthella lenta is an anaerobic, non-spore-forming, non-motile, gram-positive bacillus that can be isolated from human feces and a few other clinical specimens. Bacteremia caused by the organism is rare but, when present, is always of clinical significance. E. lenta is an emerging pathogen that has been under-recognized because of difficulties with its laboratory identification. Few reports on E. lenta infections and the optimal treatment thereof are available. We describe a case of bacteremia caused by E. lenta in an elderly patient with an intra-abdominal abscess. We also review the current literature.
Eggerthella lenta is part of the normal human intestinal flora and has been most commonly associated with infections arising from the gastrointestinal tract [1]. Predisposing conditions include gastrointestinal tract disease, malignancies, hepatobiliary disease, immobilization, bedsores, diabetes mellitus, and stroke [234]. E. lenta is an emerging pathogen that has been under-recognized because of difficulties with its laboratory identification [3]. Few reports have addressed E. lenta infections or optimal treatments thereof. Here, we describe one case that we treated and briefly summarize the available data on E. lenta bacteremia.
A 73-yr-old male presented with fever, vomiting, and dyspnea. His medical history included a prior cerebrovascular attack and multiple complications caused by hemiplegia, including recurrent urinary tract infections and pressure sores requiring continuous medical care.
On the day of admission, his body temperature, pulse rate, respiratory rate, and blood pressure were 40.4℃, 108/min, 39/min, and 170/90 mmHg, respectively. Abdominal examina-tion revealed diffuse tenderness and guarding with absence of bowel sounds. The initial laboratory test data were as follows: Hb, 14.9 g/dL; white blood cell count, 7,250/µL (neutrophils, 78.0%); and platelets, 110,000/µL. His procalcitonin level was elevated to 28.46 ng/mL. Sputum and urine cultures were negative. PCR to detect Mycobacterium tuberculosis was negative. Abdominal and pelvic contrast computed tomography scans were suggestive of an abdominal abscess; air appeared to be present at the junction of the distal ileum and cecum. On admission, we ordered blood cultures to evaluate the fever. Escherichia coli was isolated, so we prescribed empirical intravenous levofloxacin. Despite 4 days of such treatment, the patient experienced fluctuating high-level fever, tachycardia, and hypotension and required intensive care. Blood was re-cultured and we additionally prescribed metronidazole. On hospital day 6, gram-positive rods were evident in an anaerobic blood culture bottle and were identified using several techniques, including Gram staining, examination of colony morphology, and VITEK 2 analysis (bioMérieux, Marcy, l'Etoile, France). The smooth gray colonies of rod-shaped non-sporulating bacteria were gram-positive, and the bacterial cells occurred either singly or in short chains. The isolate was catalase-positive and urease-negative. Glucose, galactose, maltose, sucrose, and saccharose were not fermented. VITEK MS (bioMérieux)-associated matrix-assisted laser desorption-ionization time-of-flight mass spectrometry identified E. lenta at a confidence level of 99.9%. For 16S rRNA sequencing, bacterial DNA was extracted, amplified, and sequenced with the aid of a 3,730 xL DNA Analyzer (sequencing service from Macrogen, Seoul, Korea). Comparison of the amplicon with database sequences (NCBI BLAST, Ez-Taxon database) revealed that the sequence was 99.9% (702/703 base pairs) identical to that of an authentic E. lenta strain (ATCC 25559). The minimum inhibitory concentrations of four antimicrobial agents were estimated using the Etest (bioMérieux), following the 2012 Clinical and Laboratory Standards Institute (CLSI) guideline M100-S22 [5]. The bacteria were grown on brucella agar supplemented with 5 µg/mL hemin, 1 µg/mL vitamin K1, and 5% (w/v) lysed sheep blood cells. The 2012 CLSI breakpoints [5] indicated that the isolate was susceptible to clindamycin, metronidazole, and meropenem, but resistant to ceftriaxone.
The fever and leukocytosis resolved slowly, and the patient was discharged after symptom relief. A nursing home stay was planned and follow-up outpatient visits were scheduled (Fig. 1).
E. lenta is an anaerobic, non-spore-forming, gram-positive bacillus of the Coriobacteriaceae first described in 1935 by Eggerth [6]. The bacterium was previously named Eubacterium lentum, but genetic analysis performed in 1999 showed that the bacterium merited its own genus [7]. Eggerthella and Eubacterium can be differentiated from closely related genera, including Propionibacterium, Bifidobacterium, Lactobacillus, and Actinomyces, on the basis of acid-production patterns upon growth in peptone/yeast extract/glucose broth. However, the bacteria are fastidious and slow-growing, and correct identification of E. lenta at the species level is difficult using conventional methods. Not even biochemical or fermentative reactions can reliably identify Eubacterium to the subspecies level [8].
Over the last decades, various commercial enzyme-based kits identifying clinically relevant anaerobes have been developed. These include the RapID-ANA II panel (Thermo Fisher Scientific Inc., Lenexa, KS, USA), the Minitek systems (BBL Microbiology Systems, Cockeysville, MD, USA), the Vitek Anaerobe Identification (ANI) card (bioMérieux), the BBL Crystal ANR ID kit (BD Diagnostics, Sparks Glencoe, MD, USA), and the API rapid ID 32A and API 20A systems (bioMérieux) [91011]. 16S rRNA sequencing is useful for confirming an E. lenta infection and is considered to be the gold standard [12]. Although we used the VITEK 2 ANI card, VITEK MS, and 16S rRNA sequencing, we suggest that the VITEK 2 system alone is adequate; the system is in use by many hospitals.
We reviewed 10 reports of laboratory-documented E. lenta bacteremia occurring from 2008 to 2015 (Table 1). Initially, traditional methods of bacterial identification (Gram staining, culture, and biochemical techniques) were used. Molecular techniques, including real-time PCR or microarray analysis, were secondarily employed to identify the causative organisms (71.4%). Many patients (81.0%) exhibited symptoms of gastroenteritis associated with diarrhea and/or vomiting. Abdominal pain was also often present. Those infected by E. lenta were already ill, and included patients hospitalized in intensive care units, the elderly, and patients with diabetes and/or chronic kidney failure (86.0%). Catheters (tubes inserted into blood vessels or the gallbladder) and other bodily tubes (e.g., running from the nose to the stomach) were common causes of bacteremia (19.0%). Several antimicrobial susceptibility testing methods (broth and agar dilution methods, disk-diffusion tests, the Etest, and automated testing systems) were used. The isolates were commonly susceptible to both clindamycin and metronidazole (Table 2).
In our case, E. coli was cultured from blood taken on the first day of hospitalization. Although we (empirically) prescribed levofloxacin, an intermittent fever (over 38.9℃) persisted for 4 days. On day 5, E. lenta was detected in the blood. After commencement of metronidazole, the fever slowly resolved. Because the isolate was resistant to levofloxacin but susceptible to metronidazole, we considered that the bacteremia was caused by a mixed infection of E. coli and E. lenta (the latter is not a normal component of skin flora). At the time of admission, the intra-abdominal abscess was the only obvious source of infection.
Recent reports have shown that several E. lenta infections were associated with the use of intrauterine devices, spondylodiscitis, female genital tract infections, cutaneous abscesses, and bacteremia (in Crohn's disease patients) [123412]. These data emphasize the importance of further investigation for bacterial virulence factors. It is suspected that transfer of E. lenta from an intra-abdominal abscess to the bloodstream may reflect a defect in the gastrointestinal tract; E. lenta is normally a gut commensal bacterium [1314]. Some reports found that E. lenta infection caused morbidity and mortality associated with septic shock and multiple organ failure. Although the pathogenesis of E. lenta bacteremia has not been well described [15], 10 recent reports indicate that the prognosis is rather favorable [12312151617181920]. Our patient required intensive care for several days but eventually recovered. Few data on E. lenta infections or the optimal treatment thereof are available.
In summary, we have reported a case of bacteremia caused by E. lenta in an elderly patient with an intra-abdominal abscess. We also reviewed the current literature.
Figures and Tables
 | Fig. 1Schematic diagram of the patient's clinical course.Abbreviations: Hb, hemoglobin; PLT, platelet; PCT, procalcitonin.
|
Table 1
Reported cases of Eggerthella lenta infection

| References | Year | Gender/Age | Clinical presentation | Clinical specimen | Underlying heath status | Method/Isolates | Identification by 16S rRNA sequencing | Antibiotic susceptibility test | Initial antibiotic treatment | Polymicrobial infection | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| [1] | 2015 | M (52.0%)/68 (mean) | Abdominal pain (63.6%) | Blood | Gastrointestinal pathology (57.6%) | Culture, commercial enzyme kits, MALDI-TOF MS/E. lenta | E. lenta (78.8%) | Disk-diffusion method, Etest | Metronidazole, Ceftriaxone, Piperacillin-tazobactam, Meropenem | Positive (39.4%) | Cured (48.5%) |
| [2] | 2014 | M/86 | Diarrhea, fever, chills, rigor, dyspnea | Blood | Type 2 DM, ESRD, gout, gastrointestinal malignancy | Culture, commercial enzyme kits/E. lenta | NT | Etest | Vancomycin, Piperacillin-tazobactam | Negative | Cured |
| [3] | 2014 | M/53 | Abdominal pain, fever, chills | Blood | Rectal cancer (anterior resection with ileostomy/Hartmann's OP/chemotherapy) | Culture, commercial enzyme kits, MALDI-TOF MS/E. lenta | E. lenta | NT | Cefotaxime, Amikacin | Negative | Cured |
| [12] | 2011 | F/21 | Abdominal pain, nausea, vomiting, diarrhea | Blood | Crohn's disease, small bowel obstruction | Culture, commercial enzyme kits/E. lenta | NT | NT | Vancomycin, Piperacillin-tazobactam | Negative | Cured |
| [15] | 2010 | F/86 | Fever, dyspnea, diarrhea | Blood | Nursing home resident | Culture, commercial enzyme kits/E. lenta | E. lenta | Disk-diffusion method, Etest | Cefuroxime, Amoxicillin | Desulfovibrio desulfuricans | Cured |
| [16] | 2014 | M/69 | Abdominal pain | Blood | ESRD, liver cirrhosis | Culture, commercial enzyme kits/E. lenta | E. lenta | Etest | Metronidazole, Flumoxef | Pseudomonas putida, Bacteroides vulgatus | Cured |
| [17] | 2008 | M/70 | Erythema, increase in local temperature, pain on palpation | Synovial fluid | Stroke, hypertension, rheumatoid arthritis | Culture, commercial enzyme kits/E. lenta | NT | Etest | Amoxicillin-clavulanic acid | Negative | Cured |
| [18] | 2012 | M/19 | Fever, fatigue, poor appetite, nonproductive cough, nausea, vomiting, weight loss | Blood | Asthma, cholecystitis | Culture/E. lenta | NT | NT | Metronidazole, Ceftriaxone | Negative | Cured |
| [19] | 2012 | M/78 | Poor appetite, abdominal discomfort | Liver aspirate through drainage catheters | Multiple hepatic abscesses | Culture/E. lenta | E. lenta | NT | Meropenem, Vancomycin | Negative | Cured |
| [20] | 2009 | F/82 | Back pain, localized tenderness | Bone biopsy, aspiration of the disc space | Bed bound, vertebral compression fractures secondary to osteoporosis | Culture/E. lenta | NT | NT | Ceftriaxone, Cloxacillin | Negative | Cured |
| This report | - | M/73 | Abdominal pain, fever, nausea, vomiting, diarrhea | Blood | Stroke, hemiplegia, intra-abdominal abscess | Culture, commercial enzyme kits, MALDI-TOF MS/E. lenta | E. lenta | Etest | Levofloxacin | Escherichia coli | Cured |
Table 2
Antimicrobial susceptibility testing results of previously reported Eggerthella lenta infections
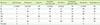
| References | Metronidazole | Clindamycin | Imipenem | Amoxicillin- clavulanic acid | Penicillin G | Trimethoprim- sulfamethoxazole | Meropenem | Chloramphenicol |
|---|---|---|---|---|---|---|---|---|
| [1] | S (100%)* | S (91.0%)* | NR | S (100%)* | S (39.0%)* | NR | S (100%)* | NR |
| [2] | S | S | NR | NR | R | NR | NR | NR |
| [3] | S | NR | S | NR | NR | NR | NR | NR |
| [15] | S | S | S | S | R | NR | NR | R |
| [16] | S | NR | NR | NR | R | NR | S | S |
| [17] | S | S | S | S | S | NR | NR | NR |
| [18] | S | NR | S | NR | NR | NR | S | NR |
| This report | S | S | S |
References
1. Gardiner BJ, Tai AY, Kotsanas D, Francis MJ, Roberts SA, Ballard SA, et al. Clinical and microbiological characteristics of Eggerthella lenta bacteremia. J Clin Microbiol. 2015; 53:626–635.

2. Wong D, Aoki F, Rubinstein E. Bacteremia caused by Eggerthella lenta in an elderly man with a gastrointestinal malignancy: a case report. Can J Infect Dis Med Microbiol. 2014; 25:e85–e86.
3. Lee HJ, Hong SK, Choi WS, Kim EC. The first case of Eggerthella lenta bacteremia in Korea. Ann Lab Med. 2014; 34:177–179.

4. Goupil R, Nadeau-Fredette AC, Tennankore KK, Bargman JM. Peritonitis caused by Veillonella species and Eggerthella lenta in peritoneal dialysis. Perit Dial Int. 2014; 34:245–247.

5. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement, M100-S22. Wayne, PA: Clinical and laboratory Standards Institute;2012.
6. Eggerth AH. The gram-positive non spore bearing anaerobic bacilli of human feces. J Bacteriol. 1935; 30:277–299.

7. Wade WG, Downes J, Dymock D, Hiom SJ, Weightman AJ, Dewhirst FE, et al. The family Coriobacteriaceae: reclassification of Eubacterium exiguum (Poco et al. 1996) and Peptostreptococcus heliotrinreducens (Lanigan 1976) as Slackia exigua gen. nov., comb. nov. and Slackia heliotrinireducens gen. nov., comb. nov., and Eubacterium lentum (Prevot 1938) as Eggerthella lenta gen. nov., comb. nov. Int J Syst Bacteriol. 1999; 49:595–600.

8. Kageyama A, Benno Y, Nakase T. Phylogenetic evidence for the transfer of Eubacterium lentum to the genus Eggerthella as Eggerthella lenta gen. nov., comb. nov. Int J Syst Bacteriol. 1999; 49:1725–1732.

9. Hansen SL, Stewart BJ. Comparison of API and minitek to Center for Disease Control methods for the biochemical characterization of anaerobes. J Clin Microbiol. 1976; 4:227–231.

10. Lee EH, Degener JE, Welling GW, Veloo AC. Evaluation of the Vitek 2 ANC card for identification of clinical isolates of anaerobic bacteria. J Clin Microbiol. 2011; 49:1745–1749.

11. Marler LM, Siders JA, Wolters LC, Pettigrew Y, Skitt BL, Allen SD. Evaluation of the new RapID-ANA II system for the identification of clinical anaerobic isolates. J Clin Microbiol. 1991; 29:874–878.

12. Thota VR, Dacha S, Natarajan A, Nerad J. Eggerthella lenta bacteremia in a Crohn’s disease patient after ileocecal resection. Future Microbiol. 2011; 6:595–597.

13. Lee MR, Huang YT, Liao CH, Chuang TY, Wang WJ, Lee SW. Clinical and microbiological characteristics of bacteremia caused by Eggerthella, Paraeggerthella, and Eubacterium species at a university hospital in Taiwan from 2001 to 2010. J Clin Microbiol. 2012; 50:2053–2055.

14. Venugopal AA, Szpunar S, Johnson LB. Risk and prognostic factors among patients with bacteremia due to Eggerthella lenta. Anaerobe. 2012; 18:475–478.

15. Liderot K, Larsson M, Boräng S, Özenci V. Polymicrobial bloodstream infection with Eggerthella lenta and Desulfovibrio desulfuricans. J Clin Microbiol. 2010; 48:3810–3812.

16. Lee J, Cho YG, Kim DS, Lee HS. Eggerthella lenta bacteremia after endoscopic retrograde cholangiopancreatography in an end-stage renal disease patient. Ann Clin Microbiol. 2014; 17:128–131.

17. Sánchez FP, Jung PAR, Lamas LM, Barca BA. Septic bursitis due to Eggerthella lenta. Reumatol Clin. 2008; 4:80–84.
18. Salameh A, Klotz SA, Zangeneh TT. Disseminated infection caused by Eggerthella lenta in a previously healthy young man: a case report. Case Rep Infect Dis. 2012; 517637.
19. Elias RM, Khoo SY, Pupaibool J, Nienaber JH, Cummins NW. Multiple pyogenic liver abscesses caused by Eggerthella lenta treated with ertapenem: a case report. Case Rep Med. 2012; e718130.
20. Bok CW, Ng YS. Eggerthella lenta as a cause of anaerobic spondylodiscitis. Singapore Med J. 2009; 50:e393–e396.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download