Abstract
Background
Dual antiplatelet therapy (aspirin and clopidogrel) is used to prevent adverse cardiac events in patients undergoing percutaneous coronary intervention (PCI). Some patients do not respond adequately to clopidogrel. Beta-thromboglobulin (β-TG) and platelet factor 4 (PF-4) can act as markers to detect platelet activation. We investigated the relationship between clopidogrel response and the dynamics of β-TG and PF4 concentrations.
Methods
This study included 36 myocardial infarction (MI) patients, who underwent PCI and was indicated for dual antiplatelet therapy. Platelet reactivity, using the VerifyNow P2Y12 assay, was measured on the 3rd day of PCI. At the time of admission, and on the 3rd and 10th day of PCI, the plasma β-TG and PF4 concentrations were quantified.
Results
Ten patients (27.8%) were clopidogrel non-responders displaying >208 P2Y12 reaction units. At the time of admission, levels of β-TG in patients were elevated than that in the healthy controls (P<0.001). A similar trend was observed on the 3rd and 10th day of PCI (P<0.001). The β-TG levels on the 10th day were reduced than those at the time of admission and on the 3rd day of PCI. PF4 levels were not different between patients and controls, and were not significantly reduced after PCI. Higher β-TG levels were observed in clopidogrel non-responders on the 10th day, but not significant.
Figures and Tables
Fig. 1
Comparison of β-thromboglobulin and platelet factor 4 at each time point of measurement in 36 patients with myocardial infarction. The central box and middle line represent 25 to 75 percentile and the median. A line extends from the minimum to the maximum value.

Table 1
Baseline characteristics of the patients in the study group at the time of hospital admission
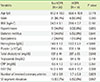
Table 2
Markers of platelet activation measured in the study group

References
1. Persantine and aspirin in coronary heart disease. Persantine-Aspirin Reinfarction Study Research Group. Circulation. 1980; 62:449–461.
2. Caro JJ, Migliaccio-Walle K. Generalizing the results of clinical trials to actual practice: the example of clopidogrel therapy for the prevention of vascular events. CAPRA (CAPRIE Actual Practice Rate Analysis) Study Group. Clopidogrel versus Aspirin in Patients at Risk of Ischaemic Events. Am J Med. 1999; 107:568–572.

3. Mehta SR, Yusuf S, Peters RJ, Bertrand ME, Lewis BS, Natarajan MK, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001; 358:527–533.

4. Angiolillo DJ. Variability in responsiveness to oral antiplatelet therapy. Am J Cardiol. 2009; 103:3 suppl. 27A–34A.

5. Breet NJ, van Werkum JW, Bouman HJ, Kelder JC, Ruven HJ, Bal ET, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010; 303:754–762.

6. Godino C, Mendolicchio L, Figini F, Latib A, Sharp ASP, Cosgrave J, et al. Comparison of VerifyNow-P2Y12 test and Flow Cytometry for monitoring individual platelet response to clopidogrel. What is the cut-off value for identifying patients who are low responders to clopidogrel therapy? Thromb J. 2009; 7:4.

7. Kaplan KL, Owen J. Plasma levels of beta-thromboglobulin and platelet factor 4 as indices of platelet activation in vivo. Blood. 1981; 57:199–202.

8. Levine SP, Lindenfeld J, Ellis JB, Raymond NM, Krentz LS. Increased plasma concentrations of platelet factor 4 in coronary artery disease: a measure of in vivo platelet activation and secretion. Circulation. 1981; 64:626–632.

9. Smitherman TC, Milam M, Woo J, Willerson JT, Frenkel EP. Elevated beta-thromboglobulin in peripheral venous blood of patients with acute myocardial ischemia: direct evidence for enhanced platelet reactivity in vivo. Am J Cardiol. 1981; 48:395–402.

10. Gavaghan TP, Hickie JB, Krilis SA, Baron DW, Gebski V, Low J, et al. Increased plasma beta-thromboglobulin in patients with coronary artery vein graft occlusion: response to low dose aspirin. J Am Coll Cardiol. 1990; 15:1250–1258.

11. Minar E, Ehringer H. Influence of acetylsalicylic acid (1.0 g/day) on platelet survival time, beta-thromboglobulin and platelet factor 4 in patients with peripheral arterial occlusive disease. Thromb Res. 1987; 45:791–802.

12. Klovaite J, Benn M, Yazdanyar S, Nordestgaard BG. High platelet volume and increased risk of myocardial infarction: 39,531 participants from the general population. J Thromb Haemost. 2011; 9:49–56.

13. Asher E, Fefer P, Shechter M, Beigel R, Varon D, Shenkman B, et al. Increased mean platelet volume is associated with non-responsiveness to clopidogrel. Thromb Haemost. 2014; 112:137–141.

14. Trenk D, Stone GW, Gawaz M, Kastrati A, Angiolillo DJ, Müller U, et al. A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (Testing Platelet Reactivity In Patients Undergoing Elective Stent Placement on Clopidogrel to Guide Alternative Therapy With Prasugrel) study. J Am Coll Cardiol. 2012; 59:2159–2164.

15. Maruyama H, Takeda H, Dembo T, Nagoya H, Kato T, Fukuoka T, et al. Clopidogrel resistance and the effect of combination cilostazol in patients with ischemic stroke or carotid artery stenting using the VerifyNow P2Y12 Assay. Intern Med. 2011; 50:695–698.

16. Kim MH, Huo SH, Kim KS, Kim MS, Song JS. Study on the platelet factor and beta-thromboglobulin in the patients with ischemic heart disease. Korean J Intern Med. 1986; 1:1–6.

17. Diop S, Ka-Cisse M, Toure-Fall AO, Diagne Fall-Sarr F, Diop SN, Thiam D, et al. Evaluation of thrombotic risk in type 2 diabetes: determination of platelet factor 4 and beta thromboglobulin. Dakar Med. 2002; 47:247–251.
18. Buyukasýk NS, Ileri M, Alper A, Senen K, Atak R, Hisar I, et al. Increased blood coagulation and platelet activation in patients with infective endocarditis and embolic events. Clin Cardiol. 2004; 27:154–158.

19. Jaffe AS, Lee RG, Perez JE, Geltman EM, Wilner GD, Sobel BE. Lack of elevation of platelet factor IV in plasma from patients with myocardial infarction. J Am Coll Cardiol. 1984; 4:653–659.

20. Minar E, Ehringer H, Jung M, Koppensteiner R, Stümpflen A. Lack of influence of low-dose acetylsalicylic acid (100 mg daily) on platelet survival time, beta-thromboglobulin and platelet factor 4 in patients with peripheral arterial occlusive disease. Thromb Res. 1988; 52:219–226.

21. Weltermann A, Fritsch P, Kyrle PA, Schoenauer V, Heinze G, Wojta J, et al. Effects of pretreatment with clopidogrel on platelet and coagulation activation in patients undergoing elective coronary stenting. Thromb Res. 2003; 112:19–24.

22. Kamath S, Blann AD, Chin BS, Lip GY. A prospective randomized trial of aspirin-clopidogrel combination therapy and dose-adjusted warfarin on indices of thrombogenesis and platelet activation in atrial fibrillation. J Am Coll Cardiol. 2002; 40:484–490.

23. Garcia AE, Mada SR, Rico MC, Dela Cadena RA, Kunapuli SP. Clopidogrel, a P2Y12 receptor antagonist, potentiates the inflammatory response in a rat model of peptidoglycan polysaccharide-induced arthritis. PLoS One. 2011; 6:e26035.

24. Krajewski S, Kurz J, Neumann B, Greiner TO, Stolz A, Balkau B, et al. Short-acting P2Y12 blockade to reduce platelet dysfunction and coagulopathy during experimental extracorporeal circulation and hypothermia. Br J Anaesth. 2012; 108:912–921.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download