Abstract
Background
The Multiplate analyzer (Dynabyte GmbH) has been recently introduced as a platelet function test for patients taking antiplatelet drugs. The study aimed at providing basic data for determining the reference interval of parameters produced by Multiplate in Koreans and to study the factors that influence those parameters.
Methods
Blood was collected from 35 healthy volunteers (female 18, male 17) into tubes containing hirudin or 3.2% sodium citrate. Whole blood platelet aggregations triggered by adenosine-5'-diphosphate (ADP), ADP-high sensitive (ADP+PGE1 only in hirudin samples), arachidonic acid (AA), collagen or thrombin receptor activator peptide (TRAP) were investigated using Multiplate according to the manufacturer's instructions. Data from healthy volunteers for the area under the curve (AUC) were determined from the central 95th percentile of the results.
Results
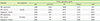
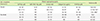
The values of AUC in hirudin samples for all agonists were significantly higher than those in sodium citrate samples. The AUC values in hirudin (sodium citrate) samples were as follows: ADP 38-107 (18-119) U; ADP+PGE1 16-91 U; AA 64-156 (32-117) U; collagen 53-112 (26-108) U; and TRAP 81-163 (49-149) U. The parameters from Multiplate were significantly correlated with leukocyte counts, but not with hematocrit levels.
Figures and Tables
Table 1
Comparison and Pearson's correlations (R value) for parameters from the Multiplate analyzer according to the anticoagulants and platelet-aggregating agents

Table 2
Reference range (central 95th percentile) for parameters from the Multiplate analyzer according to the anticoagulants and aggregating agents
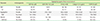
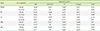
Table 3
Pearson's correlations between parameters from the Multiplate analyzer according to the anticoagulants and platelet-aggregating agents
All correlation coefficiencts were significant (P<0.001).
For abbreviations and final concentration of aggregating agents, see Table 2.
Table 4
Pearson's correlations between hematologic parameters, age and AUC (U) according to the anticoagulants and aggregating agents
*P<0.001; †P<0.01; ‡P<0.05.
For abbreviation and final concentration of aggregating agents, see Table 2.
Table 5
Comparison of reference intervals of AUC (U) according to data from references
For abbreviations, see Table 2.
*The number of individuals for the reference intervals of AUC differs according to agonist.
References
1. Woo KS, Kim BR, Kim JE, Goh RY, Yu LH, Kim MH, et al. Determination of the prevalence of aspirin and clopidogrel resistances in patients with coronary artery disease by using various platelet-function tests. Korean J Lab Med. 2010; 30:460–468.

2. Yoo NT, Bae HJ, Kim JE, Goh RY, Han JY, Kim MH, et al. Aspirin resistance may not be associated with clinical outcome after acute ischemic stroke: comparison with three different platelet function assays. Korean J Stroke. 2012; 14:35–42.

3. Tóth O, Calatzis A, Penz S, Losonczy H, Siess W. Multiple electrode aggregometry: a new device to measure platelet aggregation in whole blood. Thromb Haemost. 2006; 96:781–788.

4. Packham MA, Bryant NL, Guccione MA, Kinlough-Rathbone RL, Mustard JF. Effect of the concentration of Ca2+ in the suspending medium on the responses of human and rabbit platelets to aggregating agents. Thromb Haemost. 1989; 62:968–976.

5. Rubak P, Villadsen K, Hvas AM. Reference intervals for platelet aggregation assessed by multiple electrode platelet aggregometry. Thromb Res. 2012; 130:420–423.

6. Seyfert UT, Haubelt H, Vogt A, Hellstern P. Variables influencing Multiplate(TM) whole blood impedance platelet aggregometry and turbidimetric platelet aggregation in healthy individuals. Platelets. 2007; 18:199–206.

7. Görlinger K, Jambor C, Hanke AA, Dirkmann D, Adamzik M, Hartmann M, et al. Perioperative coagulation management and control of platelet transfusion by point-of-care platelet function analysis. Transfus Med Hemother. 2007; 34:396–411.

8. Park SJ, Chi HS, Min SK, Choi MO, Jang S, Park CJ. Predicting response to antiplatelet drugs with the Multiplate analyzer. Korean J Lab Med. 2008; 28(S2):S476.
9. Kalb ML, Potura L, Scharbert G, Kozek-Langenecker SA. The effect of ex vivo anticoagulants on whole blood platelet aggregation. Platelets. 2009; 20:7–11.

10. Heptinstall S, Taylor PM. The effects of citrate and extracellular calcium ions on the platelet release reaction induced by adenosine diphosphate and collagen. Thromb Haemost. 1979; 42:778–793.

11. Sibbing D, Braun S, Jawansky S, Vogt W, Mehilli J, Schömig A, et al. Assessment of ADP-induced platelet aggregation with light transmission aggregometry and multiple electrode platelet aggregometry before and after clopidogrel treatment. Thromb Haemost. 2008; 99:121–126.

12. Beyan C, Kaptan K, Ifran A, Savasci S, Oztürk Y, Okmen B. Effect of sex difference on platelet aggregation using an optical method in healthy subjects. Clin Lab Haematol. 2006; 28:14–16.

13. Kasjanovová D, Adamecková D, Gratzlová J, Hegyi L. Sex-related and age-related differences in platelet function in vitro: influence of hematocrit. Mech Ageing Dev. 1993; 71:103–109.

14. Melamed N, Yogev Y, Bouganim T, Altman E, Calatzis A, Glezerman M. The effect of menstrual cycle on platelet aggregation in reproductive-age women. Platelets. 2010; 21:343–347.

15. Otahbachi M, Simoni J, Simoni G, Moeller JF, Cevik C, Meyerrose GE, et al. Gender differences in platelet aggregation in healthy individuals. J Thromb Thrombolysis. 2010; 30:184–191.

16. Knol HM, Kemperman RF, Kluin-Nelemans HC, Mulder AB, Meijer K. Haemostatic variables during normal menstrual cycle. A systematic review. Thromb Haemost. 2012; 107:22–29.
17. Renesto P, Chignard M. Enhancement of cathepsin G-induced platelet activation by leukocyte elastase: consequence for the neutrophil-mediated platelet activation. Blood. 1993; 82:139–144.

18. Glenn JR, White AE, Johnson A, Fox SC, Behan MW, Dolan G, et al. Leukocyte count and leukocyte ecto-nucleotidase are major determinants of the effects of adenosine triphosphate and adenosine diphosphate on platelet aggregation in human blood. Platelets. 2005; 16:159–170.

19. Würtz M, Hvas AM, Kristensen SD, Grove EL. Platelet aggregation is dependent on platelet count in patients with coronary artery disease. Thromb Res. 2012; 129:56–61.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download