Abstract
Background
The two common serological test methods used for initial diagnosis of acute Mycoplasma pneumoniae (MP) pneumonia are particle agglutination assay (PA) and enzyme immunoassay (EIA). We compared the differences between the two methods and suggest a test method more suitable for clinical laboratories.
Methods
A total of 35 patients (18 adult and 17 pediatric) performed MP specific antibody test using PA (Serodia-Myco II, Fujirebio, Japan) and EIA (Ani Labsystems, Finland) methods. IgM and IgG antibodies were measured separately by EIA method. PA and both IgM and IgG EIA were tested in 26 patients and PA and IgG-EIA were tested in 9 patients.
Results
The concordance rates between PA and EIA were 57.7% for IgM and 65.7% for IgG antibodies. Positive PA results showed better agreement with IgG (77.8%) than IgM (38.9%), while negative PA results showed better agreement with IgM (100%) than IgG EIA results (25%). In adult patients, the correlation between PA titers and IgM (r=0.852, P <0.01) and IgG values (r=0.517, P <0.05) were statistically significant. In pediatric patients, the correlation between PA titers and IgG values (r=0.842, P <0.01) was statistically significant.
Conclusions
In this study, we observed that PA and EIA may not be used alternatively. Therefore, we suggest that use of both PA and IgM-EIA will be the optimal choice for laboratories. However, when laboratories are required to select one from PA or EIA, PA may be more useful to diagnose MP infection.
Figures and Tables
 | Fig. 1Correlation between PA titer and EIA measured value in the detection of Mycoplasma pneumoniae specific antibodies. (A) between PA titer and IgM-EIA (P<0.01). (B) between PA titer and IgG-EIA (P=0.07). (C) between PA titer and IgM-EIA in adults (P<0.01). (D) between PA titer and IgG-EIA in adults (P<0.05). (E) between PA titer and IgM-EIA in children (P=0.059). (F) between PA titer and IgG-EIA in children (P<0.01).
Abbreviations: PA, particle agglutination assay; EIA, enzyme immunoassay.
|
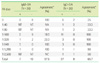
Table 1
Comparison between PA and EIA methods in the detection of
MP specific antibodies
*Measurement of agreement (k) between PA and IgM was 0.281 (P=0.039). †Measurement of agreement (k) between PA and IgG was 0.028 (P=0.869). ‡Agreement of positive and negative PA results with EIA results.
Abbreviations: PA, particle agglutination assay; EIA, enzyme immunoassay; MP, Mycoplasma pneumoniae.
Table 2
Comparison between PA and IgM-EIA methods in the detection of MP specific antibodies stratified for PA antibody titers
References
1. Kim JW, Seo SK, Yoo EG, Park SJ, Yoon SH, Jung HY, et al. Mycoplasma pneumoniae pneumonia in Korean children, from 1979 to 2006-a meta-analysis. Korean J Pediatr. 2009. 52:315–323.

2. Csabi G, Komaromy H, Hollody K. Transverse myelitis as a rare, serious complication of Mycoplasma pneumoniae infection. Pediatr Neurol. 2009. 41:312–313.
3. Smith R, Eviatar L. Neurologic manifestations of Mycoplasma pneumoniae infections: diverse spectrum of diseases. A report of six cases and review of the literature. Clin Pediatr (Phila). 2000. 39:195–201.

4. Myers PO, Khabiri E, Greub G, Kalangos A. Mycoplasma hominis mediastinitis after acute aortic dissection repair. Interact Cardiovasc Thorac Surg. 2010. 11:857–858.

5. Nagashima M, Higaki T, Satoh H, Nakano T. Cardiac thrombus associated with Mycoplasma pneumoniae infection. Interact Cardiovasc Thorac Surg. 2010. 11:849–851.
6. Shin YH, Lee BC, Song TW, Kim KW, Lee KE, Kim ES, et al. Diagnostic availability of PCR and ELISA in Mycoplasma pneumoniae Pneumonia. Pediatr Allergy Respir Dis. 2006. 16:47–56.
7. Yoo SJ, Oh HJ, Shin BM. Evaluation of Four Commercial IgG- and IgMspecific Enzyme Immunoassays for Detecting Mycoplasma pneumoniae Antibody: Comparison with Particle Agglutination Assay. J Korean Med Sci. 2007. 22:795–801.

8. Block S, Hedrick J, Hammerschlag MR, Cassell GH, Craft JC. Mycoplasma pneumoniae and Chlamydia pneumoniae in pediatric community-acquired pneumonia: comparative efficacy and safety of clarithromycin vs. erythromycin ethylsuccinate. Pediatr Infect Dis J. 1995. 14:471–477.

9. Waites KB, Talkington DF. Mycoplasma pneumoniae and Its Role as a Human Pathogen. Clinical Microbiology Reviews. 2004. 17:697–728.
10. Kim HJ, Nam SY, Yoon HS, Kim WK. Correlation between the diagnostic validity of enzymeimmunoassay and the hyperreactivity of the respiratory tract for the diagnosis of Mycoplasma pneumoniae. Pediatr Allergy Respir Dis. 2007. 17:394–403.
11. Barker CE, Sillis M, Wreghitt TG. Evaluation of Serodia Myco II particle agglutination test for detecting Mycoplasma pneumoniae antibody: comparison with mu-capture ELISA and indirect immunofluorescence. J Clin Pathol. 1990. 43:163–165.

12. Lee EY, Lee DJ, Lee JA, Kim SW, Chang MW. Comparison of PCR, Culture and Serologic Tests for Diagnosis of Mycoplasma pneumoniae Infection. Pediatr Allergy Respir Dis. 2005. 15:359–367.
13. McCormick DP, Wenzel RP, Senterfit LB, Beam WE Jr. Relationship of pre-existing antibody to subsequent infection by Mycoplasma pneumoniae in adults. Infect Immun. 1974. 1:53–59.
14. Theile A, Karg O, Wex P, Muller KM. Bronchiolitis obliterans after Mycoplasma pneumonia. Pneumologie. 1994. 48:491–494.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download