Abstract
Carbapenem resistance in Acinetobacter baumannii has increased rapidly worldwide. It is generally assumed that carbapenem prescription in a hospital has a significant impact on imipenem resistance in A. baumannii. However, there are few studies validating these assumptions with statistical data. We performed a surveillance study to investigate the relationship between carbapenem prescription trends and the imipenem resistance rate of A. baumannii in an ICU. Carbapenem prescription data in the WHO anatomical therapeutic chemical (ATC)/defined daily dose (DDD) format for the period from 2006 to 2010 were obtained from the hospital electronic pharmacy records. In the same period, microbiologic data for the ICU were extracted from the laboratory information system. Imipenem resistance rates of A. baumannii increased from 4.3% in 2006 to 83.8% in 2010 (P <0.05; r2=0.85). Carbapenem prescription had increased from 19.71 DDD per 1,000 inpatient-days in 2006 to 36.99 DDD per 1,000 inpatient-days in 2010 (P <0.05; r2=0.95). Carbapenem prescription rate correlated with the imipenem resistance rate in A. baumannii (P <0.05; R=0.9). The results of our study demonstrated a correlation between carbapenem prescription trends and imipenem resistance in A. baumannii.
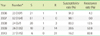
Figures and Tables
References
1. Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008. 21:538–582.

2. Fournier PE, Richet H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin Infect Dis. 2006. 42:692–699.

3. Cisneros JM, Reyes MJ, Pachón J, Becerril B, Caballero FJ, García-Garmendía JL, et al. Bacteremia due to Acinetobacter baumannii: epidemiology, clinical findings, and prognostic features. Clin Infect Dis. 1996. 22:1026–1032.

4. Mera RM, Miller LA, Amrine-Madsen H, Sahm DF. Acinetobacter baumannii 2002-2008: increase of carbapenem-associated multiclass resistance in the United States. Microb Drug Resist. 2010. 16:209–215.

5. Goossens H, Ferech M, Vander Stichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005. 365:579–587.

6. Hsu LY, Tan TY, Tam VH, Kwa A, Fisher DA, Koh TH. Surveillance and correlation of antibiotic prescription and resistance of Gram-negative bacteria in Singaporean hospitals. Antimicrob Agents Chemother. 2010. 54:1173–1178.

7. van de Sande-Bruinsma N, Grundmann H, Verloo D, Tiemersma E, Monen J, Goossens H, et al. Antimicrobial drug use and resistance in Europe. Emerg Infect Dis. 2008. 14:1722–1730.

8. Sandiumenge A, Diaz E, Rodriguez A, Vidaur L, Canadell L, Olona M, et al. Impact of diversity of antibiotic use on the development of antimicrobial resistance. J Antimicrob Chemother. 2006. 57:1197–1204.

9. Goel N, Wattal C, Oberoi JK, Raveendran R, Datta S, Prasad KJ. Trend analysis of antimicrobial consumption and development of resistance in non-fermenters in a tertiary care hospital in Delhi, India. J Antimicrob Chemother. 2011. 66:1625–1630.

10. Lai CC, Wang CY, Chu CC, Tan CK, Lu CL, Lee YL, et al. Correlation between antimicrobial consumption and resistance among Staphylococcus aureus and enterococci causing healthcare-associated infections at a university hospital in Taiwan from 2000 to 2009. Eur J Clin Microbiol Infect Dis. 2011. 30:265–271.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download