Abstract
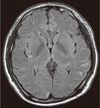
The HACEK group of microorganisms is responsible for approximately 3-6% of endocarditis cases and is a major cause of culture-negative endocarditis. Here, we report a case of Haemophilus parainfluenzae infective endocarditis that was diagnosed by direct PCR sequencing of 16S rRNA from resected vegetation. A healthy 26-yr-old man was admitted to the emergency room (ER) on March 27, 2011 because of intermittent high fever. The patient was prescribed cefpodoxime for 5 days at the ER. Six and 11 sets of blood cultures were performed at the ER and in a general ward, respectively, using BACTEC Plus Aerobic/F (Becton-Dickinson, USA) and Lytic Anaerobic/F Plus (BD) together. Echocardiography revealed a large vegetation at the posterior mitral valve leaflet. After performing mitral valvoplasty on hospital day (HD) 11, the vegetation tissue was cultured in thioglycolate broth, blood agar, Brucella agar, and MacConkey agar for 7 days, but no organism was grown. Direct PCR sequencing of 16S rRNA of the tissue revealed the presence of H. parainfluenzae. In the 17 sets of blood cultures, bacterial growth was detected in only 2 aerobic bottles of 5 sets taken at HD 9 after 10-day and 14-day incubation. The organism was identified as H. parainfluenzae by using the VITEK NHI card (bioMerieux, France). Direct PCR sequencing of vegetation could be useful in diagnosing bacterial pathogens in infective endocarditis patients, especially in culture-negative cases.
Figures and Tables
References
1. Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000. 30:633–638.

2. Lamas CC, Eykyn SJ. Blood culture negative endocarditis: analysis of 63 cases presenting over 25 years. Heart. 2003. 89:258–262.

3. Mandell GL, Bennett JE, editors. Principles and practice of infectious diseases. 2010. 7th ed. Philadelphia, PA: Churchill Livingstone;1067–1112.
4. Versalovic J, Carroll KC, editors. Manual of clinical microbiology. 2011. 10th ed. Washington, DC: American Society for Microbiology;588–598.
5. Steckelberg JM, Melton LJ 3rd, Ilstrup DM, Rouse MS, Wilson WR. Influence of referral bias on the apparent clinical spectrum of infective endocarditis. Am J Med. 1990. 88:582–588.

6. Darras-Joly C, Lortholary O, Mainardi JL, Etienne J, Guillevin L, Acar J. Haemophilus Endocarditis Study Group. Haemophilus endocarditis: report of 42 cases in adults and review. Clin Infect Dis. 1997. 24:1087–1094.

7. Rohner P, Pepey B, Auckenthaler R. Comparative evaluation of BACTEC aerobic Plus/F and Septi-Chek Release blood culture media. J Clin Microbiol. 1996. 34:126–129.

8. Clinical and Laboratory Standards Institute. Principles and procedures for blood cultures; Approved guideline. CLSI document M47-A. 2007. Wayne, PA: Clinical and Laboratory Standard Institute.
9. Washington JA 2nd. Blood cultures: principles and techniques. Mayo Clin Proc. 1975. 50:91–98.
10. Baron EJ, Scott JD, Tompkins LS. Prolonged incubation and extensive subculturing do not increase recovery of clinically significant microorganisms from standard automated blood cultures. Clin Infect Dis. 2005. 41:1677–1680.

11. Doern GV, Davaro R, George M, Campognone P. Lack of requirement for prolonged incubation of Septi-Chek blood culture bottles in patients with bacteremia due to fastidious bacteria. Diagn Microbiol Infect Dis. 1996. 24:141–143.

12. Forward KR. An evaluation of extended incubation time with blind subculture of blood cultures in patients with suspected endocarditis. Can J Infect Dis Med Microbiol. 2006. 17:186–188.

13. Huh JH, Bae SY, Kim JS, Lee KN, Lee CK. A case of Haemophilus parainfluenzae endocarditis. Korean J Clin Microbiol. 2009. 12:78–81.
14. Hong KW, Lee JA, Park HW, Kwon HL, Cho SJ, Kim JS, et al. A case of infective endocarditis caused by Aspergillus fumigatus in a liver transplant recipient. Korean J Med. 2008. 75:115–118.
15. Ryu KH, Choi HJ, Park SH, Park SH, Lee MA. Two cases of Haemophilus parainfluenzae endocarditis. Infect Chemother. 2003. 35:345–349.
16. Pazin GJ, Saul S, Thompson ME. Blood culture positivity: suppression by outpatient antibiotic therapy in patients with bacterial endocarditis. Arch Intern Med. 1982. 142:263–268.

17. Graig WA, Gudmundsson S. Lorian V, editor. Postantibiotic effects. Antibiotics in laboratory medicine. 1996. 4th ed. Baltimore, Maryland: Williams & Wikins;296–329.
18. Horstkotte D, Follath F, Gutschik E, Lengyel M, Oto A, Pavie A, et al. Guidelines on prevention, diagnosis and treatment of infective endocarditis executive summary; the task force on infective endocarditis of the European society of cardiology. Eur Heart J. 2004. 25:267–276.

19. Kelesidis T, Kelesidis I, Lewinski MA, Humphries R. Establishing diagnosis of Haemophilus parainfluenzae as etiology of culture-negative endocarditis using DNA sequence analysis on tissue specimen. Am J Med. 2011. 124:e9–e10.

20. Westling K, Vondracek M. Actinobacillus (Aggregatibacter) actinomycetemcomitans (HACEK) identified by PCR/16S rRNA sequence analysis from the heart valve in a patient with blood culture negative endocarditis. Scand J Infect Dis. 2008. 40:981–983.

21. Marín M, Muñoz P, Sánchez M, del Rosal M, Alcalá L, Rodríguez-Créixems M, et al. Molecular diagnosis of infective endocarditis by real-time broad-range polymerase chain reaction (PCR) and sequencing directly from heart valve tissue. Medicine (Baltimore). 2007. 86:195–202.

22. Fernández AL, Varela E, Martínez L, Martínez A, Sierra J, González-Juanatey JR, et al. Evaluation of a multiplex real-time PCR assay for detecting pathogens in cardiac valve tissue in patients with endocarditis. Rev Esp Cardiol. 2010. 63:1205–1208.

23. Voldstedlund M, Nørum Pedersen L, Baandrup U, Klaaborg KE, Fuurst-ed K. Broad-range PCR and sequencing in routine diagnosis of infective endocarditis. APMIS. 2008. 116:190–198.

24. Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009. 169:463–473.

25. Winn WC, Allen SD, editors. Koneman's color atlas and textbook of diagnostic microbiology. 1997. 6th ed. Baltimore, MD: Lippincott Williams & Wilkins;429–452.
26. Kang MH, Lim KR, Kim TS, Kim SH, Kim GH, Oh WS, et al. A case of early valve replacement for Haemophilus parainfluenzae endocarditis complicated with acute cerebral infarctions. Infect Chemother. 2011. 43:270–274.

27. Yang DJ, Ryu YS, Chung MY, Park EK, Park JY, Cho YB, et al. A case of Haemophilus parainfluenzae-related tricuspid valve endocarditis in an unhygenically insulin-injected patient. Korean J Med. 2009. 77:Suppl 5. S1170–S1173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download