Abstract
Bacteria belonging to the genus Tsukamurella are aerobic, gram-positive rods that are weakly acid-fast with no apparent branching. Infections of the Tsukamurella spp. are generally caused by the use of infected medical devices such as central venous catheters. The underreporting of these infections might be attributable to the frequent misdiagnosis of Tsukamurella infections as Corynebacterium or atypical Mycobacterium spp. infections. Therefore, when gram-positive aerobic rods are observed in the blood culture of a patient with a central venous catheter, it is important to consider Tsukamurella as one of the causative organisms. Here, we report the first case of a catheter-related blood stream infection caused by Tsukamurella inchonensis in a 3-yr-old Korean girl with underlying biliary atresia who underwent hepatoportoenterostomy.
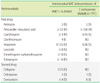
Figures and Tables
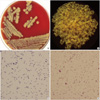 | Fig. 1Macroscopic and microscopic features of the isolated strain. (A) Growth of the strain after 72 hr on blood agar plates; (B) A colony of the strain after 72-hr growth (×10); (C) Gram stain of the strain after a 48-hr growth (×1,000); (D) Modified acid-fast bacilli (AFB) stain of the strain after a 48-hr growth (&1,000) |
 | Fig. 2A dendrogram illustrating the phylogenetic relationships between our clinical isolate (YMC11-5-B1957) and T. inchonensis, T. paurometabola, T. tyrosinosolvens, T. strandjordae, T. pulmonis, T. carboxydivorans, T. pseudospumae, T. spumae, T. sunchonensis, and T. spongiae strains based on the 16S rRNA gene sequencing. The scale indicates the similarity index. |
References
1. Conville PS, Witebsky FG. Murray PR, Baron EJ, editors. Nocardia, Rhodococcus, Gordonia, Actinomadura, Streptomyces, and Other Aerobic Actionmycetes. Manual of clinical microbiology. 2007. 9th ed. Washington DC: ASM Press;515–535.
2. Maalouf R, Mierau SB, Moore TA, Kaul A. First case report of community-acquired pneumonia due to Tsukamurella pulmonis. Ann Intern Med. 2009. 150:147–148.

3. Alcaide ML, Espinoza L, Abbo L. Cavitary pneumonia secondary to Tsukamurella in an AIDS patient. First case and a review of the literature. J Infect. 2004. 49:17–19.

4. Larkin JA, Lit L, Sinnott J, Wills T, Szentivanyi A. Infection of a knee prosthesis with Tsukamurella species. South Med J. 1999. 92:831–832.
5. Shaer AJ, Gadegbeku CA. Tsukamurella peritonitis associated with continuous ambulatory peritoneal dialysis. Clin Nephrol. 2001. 56:241–246.
6. Woo PC, Ngan AH, Lau SK, Yuen KY. Tsukamurella conjunctivitis: a novel clinical syndrome. J Clin Microbiol. 2003. 41:3368–3371.

7. Woo PC, Fong AH, Ngan AH, Tam DM, Teng JL, Lau SK, et al. First report of Tsukamurella keratitis: association between T. tyrosinosolvens and T. pulmonis and ophthalmologic infections. J Clin Microbiol. 2009. 47:1953–1956.

8. Shim HE, Sung H, Baek SM, Namgung S, Kim MN, Kim YG, et al. A case of catheter-related bacteremia of Tsukamurella pulmonis. Korean J Lab Med. 2009. 29:41–47.
9. Elshibly S, Doherty J, Xu J, McClurg RB, Rooney PJ, Millar BC, et al. Central line-related bacteraemia due to Tsukamurella tyrosinosolvens in a haematology patient. Ulster Med J. 2005. 74:43–46.
10. Bouza E, Pérez-Parra A, Rosal M, Martín-Rabadán P, Rodríguez-Créixems M, Marín M. Tsukamurella: a cause of catheter-related bloodstream infections. Eur J Clin Microbiol Infect Dis. 2009. 28:203–210.

11. Clinical and Laboratory Standards Institute. CLSI document MM18-A. Interpretive criteria for identification of bacteria and fungi by DNA target sequencing; approved guideline. 2008. Wayne, PA: Clinical and Laboratory Standards Institute.
12. Cho AR, Kim HR, Lee MK, Choi SH, Yun SW. A case report of Tsukamurella pulmonis infection misidentified as atypical mycobacteria. Korean J Clin Microbiol. 2010. 13:93–97.

13. Park JC, Hong J, Seo JG, Chung WK, Seo YH, Lee HH. A case of Tsukamurella tyrosinosolvens peritonitis associated with continuous ambulatory peritoneal dialysis. Korean J Med. 2009. 76:225–228.
14. Lo SF. Kliegman R, Nelson WE, editors. Reference intervals for laboratory tests and procedures. Nelson textbook of pediatrics. 2011. 19th ed. Philadelphia, PA: Elsevier/Saunders.

15. Chun J, Lee JH, Jung Y, Kim M, Kim S, Kim BK, et al. EzTaxon: a web-based tool for the identification of prokaryotes based on 16S ribosomal RNA gene sequences. Int J Syst Evol Microbiol. 2007. 57:2259–2261.

16. Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987. 4:406–425.
17. National Committee for Clinical Laboratory Standards. NCCLS document M24-A. Susceptibility testing of Mycobacteria, Nocardiae, and other aerobic actinomycetes; approved standard. 2003. Wayne, PA: National Committee for Clinical Laboratory Standards.
18. Guidelines and procedures for monitoring CLABSI (Central Line-Associated Bloodstream Infection). Centers for Disease Control and Prevention: National Healthcare Safety Network. Updated on Jun 2011. http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf.
19. Yassin AF, Rainey FA, Brzezinka H, Burghardt J, Lee HJ, Schaal KP. Tsukamurella inchonensis sp. nov. Int J Syst Bacteriol. 1995. 45:522–527.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download