Abstract
Background
Lung cancer is one of the leading causes of cancer-related deaths throughout the world. The gene tumor protein 53 (TP53) is frequently mutated in cases of lung cancer. This study was performed to investigate the frequencies and types of mutations in the TP53 gene in Korean patients with lung cancer.
Methods
We obtained tissue samples from 80 lung cancer patients and synthesized TP53 cDNA by using RNA isolated from these tissues by performing reverse transcriptase polymerase chain reaction. Hybridization and denaturing high-performance liquid chromatography were performed to identify the TP53 gene mutations, and then, the mutations were validated by direct sequencing.
Results
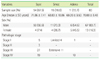
Forty mutations out of the 80 patients (50.0%) were noted in the TP53 gene. The frequencies of TP53 gene mutation for different cancer types, namely, squamous cell carcinoma, adenocarcinoma, and small cell carcinoma were 61.1%, 27.3%, and 26.7%, respectively. The mutation frequencies in the different regions of the gene were 10.0% for exon 4, 35.0% for exon 5, 12.5% for exon 6, 22.5% for exon 7, 17.5% for exon 8, and 2.5% for exon 9. The frequently mutated positions were codon 179 in exon 5, codons 202 and 220 in exon 6, and codons 266 and 273 in exon 8.
Figures and Tables
 | Fig. 1Denaturing high-performance liquid chromatography (DHPLC) analysis of exons 4-5 and 6-9.
Chromatograms obtained by performing DHPLC for exons 4-5 (A) and 6-9 (B) of wild type (a) and mutated (b) TP53 gene. The chromatograms for both the regions of the wild type gene were similar to those for the corresponding regions of the controls, while those for both the regions of the mutant genes were different from those for the corresponding regions of the controls.
|
References
1. Minna JD. Pass HI, Mitchell JB, Johnson DH, Turrisi AT, editors. Molecular biology overview. Lung cancer: principles and practice. 1996. 1st ed. Philadelphia: Lippincott-Raven;143–148.
2. Mendelsohn J. Targeting the epidermal growth factor receptor for cancer therapy. J Clin Oncol. 2002. 20:18 Suppl. 1S–13S.
3. Sozzi G, Pastorino U, Moiraghi L, Tagliabue E, Pezzella F, Ghirelli C, et al. Loss of FHIT function in lung cancer and preinvasive bronchial lesions. Cancer Res. 1998. 58:5032–5037.
5. Olivier M, Hollstein M, Hainaut P. TP53 mutations in human cancers: origins, consequences, and clinical use. Cold Spring Harb Perspect Biol. 2010. 2:a001008.

6. Hainaut P, Hollstein M. p53 and human cancer: the first ten thousand mutations. Adv Cancer Res. 2000. 77:81–137.

9. Jassem E, Nikliński J, Rosell R, Niklińska W, Jakóbkiewicz J, Monzo M, et al. Types and localisation of p53 gene mutations: a report on 332 non-small cell lung cancer patients. Lung Cancer. 2001. 34:Suppl 2. S47–S51.
10. Feng Z, Hu W, Rom WN, Costa M, Tang MS. Chromium(VI) exposure enhances polycyclic aromatic hydrocarbon-DNA binding at the p53 gene in human lung cells. Carcinogenesis. 2003. 24:771–778.

11. Pfeifer GP, Denissenko MF, Oliver M, Tretyakova N, Hecht SS, Hainaut P. Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene. 2002. 21:7435–7451.

12. Hussain SP, Amstad P, Raja K, Sawyer M, Hofseth L, Shields PG, et al. Mutability of p53 hotspot codons to benzo(a)pyrene diol epoxide (BPDE) and the frequency of p53 mutations in nontumorous human lung. Cancer Res. 2001. 61:6350–6355.
13. Lee EB, Jin G, Lee SY, Park JY, Kim MJ, Choi JE, et al. TP53 mutations in Korean patients with non-small cell lung cancer. J Korean Med Sci. 2010. 25:698–705.

14. Walker DR, Bond JP, Tarone RE, Harris CC, Makalowski W, Boguski MS, et al. Evolutionary conservation and somatic mutation hotspot maps of p53: correlation with p53 protein structural and functional features. Oncogene. 1999. 18:211–218.

15. Kato S, Han SY, Liu W, Otsuka K, Shibata H, Kanamaru R, et al. Understanding the function-structure and function-mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc Natl Acad Sci USA. 2003. 100:8424–8429.

16. Takahashi T, Nau MM, Chiba I, Birrer MJ, Rosenberg RK, Vinocour M, et al. p53: a frequent target for genetic abnormalities in lung cancer. Science. 1989. 246:491–494.

17. Hu Y, McDermott MP, Ahrendt SA. The p53 codon 72 proline allele is associated with p53 gene mutations in non-small cell lung cancer. Clin Cancer Res. 2005. 11:2502–2509.

18. Sidransky D, Hollstein M. Clinical implications of the p53 gene. Annu Rev Med. 1996. 47:285–301.

19. Horio Y, Takahashi T, Kuroshi T, Hibi K, Suyama M, Niimi T, et al. Prognostic significance of p53 mutations and 3p deletions in primary resected non-small cell lung cancer. Cancer Res. 1993. 53:1–4.
20. Hashimoto T, Tokuchi Y, Hayashi M, Kobayashi Y, Nishida K, Hayashi S, et al. Different subtypes of human lung adenocarcinoma caused by different etiological factors. Evidence from p53 mutational spectra. Am J Pathol. 2000. 157:2133–2141.

21. International Agency for Research on Cancer. IARC tp53 database, R15. World Health Organization. Updated on Nov 2010. http://www-p53.iarc.fr/index.html.
22. Hernandez-Boussard TM, Hainaut P. A specific spectrum of p53 mutations in lung cancer from smokers: review of mutations compiled in the IARC p53 database. Environ Health Perspect. 1998. 106:385–391.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download