Abstract
We report a case of a 65-year-old man with Behcet's disease who presented with massive hemoptysis caused by bronchial varices. A computed tomography (CT) scan and bronchoscopy were performed to identify the bleeding site. The CT scan revealed pneumonia and a combined hemorrhage in the right-middle and lower lobes. Massive bleeding was detected during the bronchoscopy and emergency embolization was attempted but angiographic findings were normal. An anteriojugulo-right femoral bypass operation was performed to relieve the tortuous and hypertrophied jugular venous obstruction. However, thrombectomy and thrombolysis followed because of graft thrombosis six days post-surgery. The patient was treated with steroid and high-dose cyclophosphamide therapy for his Behçet's disease, which caused the venous obstructions; the saccular bronchial varices in the right-middle and right lower lobes on bronchoscopy regressed slightly after four cycles of cyclophosphamide therapy
Behçet's disease, characterized by oral ulcers, recurrent genital ulcers, and uveitis or iritis, is widely known as a chronic recurrent systemic inflammatory disease affecting the gastrointestinal tract, nervous system, blood vessels, and multiple mediastinal structures.1 Vascular involvement is reported in 25–50% of cases. The veins are the most commonly affected vessels, particularly the superior vena cava (SVC) and inferior vena cava.2 A bronchial varix usually develops primarily but can be secondary if bronchial venous pressure is elevated by another cause.4 Bleeding from a bronchial varix is a rare cause of hemoptysis. However, a few case reports have described bronchial varices associated with Behçet's disease. We report a case of bronchial varices diagnosed via bronchoscopy that formed as collateral venous circulation secondary to a SVC obstruction in a patient with Behçet's disease.
64-year-old man presented to our emergency room with a 100 mL episode of hemoptysis in May 2011. He had been diagnosed with Behçet's disease in 1989 and admitted to a hospital in 2004 for dilatation of anterior chest and abdominal superficial veins. During that time, an SVC obstruction was found on a chest computed tomography (CT) scan and esophageal varices were detected on an upper endoscopic exam. Since then, he had been taking prednisone (20 mg/d) and colchine (1.2 mg/d) but no antiplatelet or anticoagulation agent. He stopped taking these medications on his own and had not visited our clinic for a long time. He also had a history of schizophrenia reported in 2000. He was an ex-smoker with a 25 pack-year smoking history. The family history was non-contributory. Blood pressure was 110/63 mmHg, pulse rate was 60/min, respiration rate was 20/min, and body temperature was 37℃. Crackles were heard in the right lower lung field on auscultation, but no cardiac murmur was detected. Although there was no definite facial or neck edema, the jugular and superficial veins in the anterior chest and abdomen were distended (Fig. 1). Whitish ulcers surrounded by circular erythema and ulcerous scars were found in the oral cavity and genital area. No hepatosplenomegaly or lower-extremity edema was observed. No focal neurological signs were detected. On admission, the white blood cell count was 3,940/mm3 (4,000–10,000/mm3) with 67.6% (42–75%) segmented neutrophils. Hemoglobin was 13.3 g/dL (12–16 g/dL), and the platelet count was 137,000/mm3 (150,000–450,000/mm3). Blood urea nitrogen was 13.1 mg/dL (6–20 mg/dL), creatinine was 0.7 mg/dL (0.5–1.2 mg/dL), total protein was 6.2 g/dL (6.4–8.3 g/dL), albumin was 3.8 mg/dL (3.5–5.2 mg/dL), aspartate aminotransferase/alanine aminotransferase was 26/26 IU/L (8–32 IU/L), total bilirubin was 1.7 mg/dL (0.2–1.2 mg/dL), sodium was 136 mEq/L (136–145 mEq/L), potassium was 3.6 mEq/L (3.5–5.1 mEq/L), C-reactive protein was 0.97 mg/L (0–3 mg/L), and erythrocyte sedimentation rate was 8 mm/h (0–20 mm/h). Arterial blood gas analysis revealed a pH of 7.44 (7.35–7.45), PaCO2 of 36 mmHg (35–45 mmHg), PaO2 of 68 mmHg (75–100 mmHg), and HCO3 of 24 mEq/L (23–30 mEq/L). Simple radiography showed inhomogenous consolidation in the right lower lung field and no specific findings in the abdomen. An enhanced chest CT revealed consolidated lesions in the right-lower and middle lung fields but no ground glass opacity, suggestive of pneumonia and hemorrhage. Obstructions were found in the SVC and brachiocephalic and subclavian veins, which likely caused the formation of many collateral veins in the mediastinum, retroperitoneum, and chest and abdominal walls (Fig. 2). A bronchoscopy showed linear hypertrophied bronchial varices (Fig. 3). Massive bleeding occurred during the bronchoscopy, and epinephrine was injected. Then, emergency embolization was attempted but the angiographic findings were normal. The patient was transferred to the intensive care unit for close observation. His vital signs were stable despite bleeding. Echocardiography was performed to rule out bronchial varices induced by a cardiac problem; a normal ejection fraction was detected, and he had no pulmonary arterial hypertension or valve disease. An anteriojugulo-right femoral bypass operation was performed to relieve the tortuous and hypertrophied obstruction in the jugular vein. No additional hemoptysis occurred postoperatively. Furthermore, the superficial anterior chest and abdominal venous distension were markedly relieved. However, thrombectomy and thrombolysis followed because a graft thrombosis occurred six days after surgery. The patient's Behçet's disease, which caused the venous obstructions, was treated with intravenous systemic methylprednisolone (125 mg) for two days, followed by prednisone (10 mg/day) and six cycles of monthly high dose cyclophosphamide therapy. In addition, warfarin was started for the graft thrombosis and SVC obstruction. Since then, no hemoptysis has been observed, and a follow-up bronchoscopy after four cycles of cyclophosphamide therapy demonstrated regressed saccular bronchial varices in the right-medial and right-lower lobes (Fig. 4).
Bronchial varices form primarily in patients with severe bronchiectasis, obstructive lung disease, and pulmonary fibrosis, as well as secondary to elevated bronchial venous pressure caused by mitral-valve stenosis or a pulmonary venous obstruction.3 Bleeding from the veins is rarely found on bronchoscopy and only incidentally in patients with hemoptysis.4 The longer the SVC obstruction remains, the more collateral veins without SVC drainage form due to flow from the head/neck area and upper extremities.5 This collateral circulation produces varices at the lower esophagus between the left gastric vein and the left azygous vein or anastomosis of the left gastric vein with the adjacent bronchial vein. Venous flow bypassing the SVC can rapidly produce bronchial and esophageal varices without portal hypertension. Many cases of bronchial varix have been reported, but none in patients with Behçet's disease.3456789 Although the exact mechanism of vessel obstruction associated with Behçet's disease is unknown, a complex mechanism involving interactions among T lymphocytes, neutrophils, and antigen-presenting cells has been proposed.510 In addition, a genetic mutation may contribute;6 no thrombophilic factor is known to be involved. Gul et al. reported that the factor V gene G1691A mutation is associated with formation of a thrombus, but some reports have indicated that thrombosis in patients with Behçet's disease is not caused by a coagulation disorder.7 Thus, more studies are needed to find the mechanism.
The focus of a hemoptysis is usually identified by contrast-enhanced CT and bronchoscopy. Emergency angiography and embolization are the first choice in cases of massive hemoptysis. In our case, we found an SVC obstruction and collateral vessel formation on CT and bronchial varices on bronchoscopy. However, because of the massive bleeding, we performed emergency angiography that found no abnormality. One case report describes a patient with portal hypertension presenting with massive hemoptysis due to bronchial varices found by venous phase mesenteric arteriography and direct portography, successfully treated with a transjugular intrahepatic portosystemic shunt.9 Clinical suspicion, finding the bleeding focus, and prompt treatment are fundamental in these cases. Moreover, the underlying disease causing the bronchial varices should be corrected. In general, steroids, immunosuppressants, and anticoagulants are useful to treat systemic vasculitis and vascular thrombosis, respectively.11 In our case, we performed an anterojugulo-right femoral bypass to treat venous thrombosis, but it provided only temporary relief, failing due to a graft thrombosis. Fortunately, the bronchial varices regressed after systemic steroid and cyclophosphamide treatment. Bronchial varices can form for many reasons, and a few reports have described bronchial varices associated with Behcet's disease. Although the exact mechanism for an obstructed vessel due to Behcet's disease is unknown, a complex mechanism involving interactions among T lymphocytes, neutrophils, and antigen-presenting cells has been proposed. Bronchial varices should be considered a cause of bleeding in patients presenting with hemoptysis and comorbidities that increase bronchial venous pressure, such as portal hypertension, heart disease, or an uncontrolled autoimmune disease. Although formation of venous collaterals is very rare, early exploration and management of these high-risk patients may be lifesaving. In conclusion, bronchoscopy should be considered to detect bronchial varices early, particularly in high-risk patients with signs of venous collateral formation. Early efforts to control the underlying etiology and active exploration will improve survival and patient quality of life.
Figures and Tables
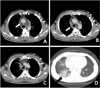 | Fig. 2Contrast-enhanced thoracic computed tomography reveals an obstruction of the superior vena cava (SVC) (A, white arrow) and a narrowed right azygous vein (B, white arrow), resulting in numerous collateral vessels, including bilateral brachiocephalic and subclavian veins with numerous collaterals (C, multiple thin white arrows). Pneumonia in the right-middle and lower lobes and a combined hemorrhage underlying early interstitial fibrosis are visible at the base of both lungs (D, black arrow). |
References
1. Chajek T, Fainaru M. Behçet's disease. Report of 41 cases and a review of the literature. Medicine (Baltimore). 1975; 54:179–196.

2. Düzgün N, Ateş A, Aydintuğ OT, Demir O, Olmez U. Characteristics of vascular involvement in Behcet's disease. Scand J Rheumatol. 2006; 35:65–68.
3. Moon SY, Kim SY, Cheon WS, Eom KS, Jang SH, Bahn JW, et al. A Case of Bronchial Varices in a Patient with Severe Mitral Stenosis. Tuberc Respir Dis. 2005; 58:174–178.

4. Wiebe S, Masclusky I, Manson D, Holowka S, Yoo SJ. Hemoptysis: a rare cause can be related to a bronchial varix due to pulmonary venous obstruction. Pediatr Radiol. 2003; 33:884–886.

5. Tavakkoli H, Asadi M, Haghigh M, Esmaeili A. Therapeutic approach to “downhill” esophageal varices bleeding due to superior vena cava syndrome in Behcet's disease: a case report. BMC Gastroenterol. 2006; 6:43.

6. Yu M, Shi A, Jin B, Jiang X, Liang H, Ouyang C. Superior vena cava occlusion caused by Behçet disease. J Vasc Surg. 2012; 55:1488–1491.

7. Nagahiro I, Toda D, Andou A, Shimizu N. A Case of bronchial varices due to extrahepatic portal hypertension. Respiration. 2007; 74:460–461.

8. Seyahi E, Yurdakul S. Behçet's Syndrome and Thrombosis. Mediterr J Hematol Infect Dis. 2011; 3:e2011026.

9. Mansilla AV, Ball D, Putman SG, Cohen GS, Krachman S, Black M. Massive hemoptysis secondary to bronchial collaterals: treatment with use of TIPS and embolization. J Vasc Interv Radiol. 1999; 10:372–374.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download