Abstract
During the course of evaluation and management of neck masses, consideration for Immunoglobulin G4-related disease (IgG4-RD) should be given. IgG4-RD is relatively a new growing entity of immune-mediated origin, characterized by a mass-forming lesion, the infiltration of IgG4-positive plasma cells and occasionally elevated serum IgG4. The most common manifestations are parotid and lacrimal swelling, lymphadenopathy and autoimmune pancreatitis.
A previously healthy 72-year-old man was referred to our clinic with a 2-month history of left cervical lymph node enlargement without systemic manifestations . A cervical lymph node biopsy was planned because of elevated serum IgG4 levels. Pathological findings showed prominent infiltration of IgG4-postive plasma cells in the lymph node. After steroid therapy, a computed tomography scan revealed a decrease in the cervical lymph node size.
This case illustrates the importance of including IgG4-RD in the differential diagnosis of a cervical lymph node enlargement.
For the differential diagnosis of a patient with lymph node enlargement, the possibility of an infectious disease caused by viral or bacterial infection, lymphadenitis caused by an autoimmune disease, a neoplastic lesion such as Hodgkin's lymphoma and non-Hodgkin's lymphoma, and a rheumatoid disease such as systemic lupus erythematosus and rheumatoid arthritis may be considered.1 In addition, immunoglobulin G4 related disease with lymphadenopathy should be considered as a possible cause of lymph node enlargement.
IgG4-related disease, which is a disease causing fibrinous inflammatory histological changes as IgG4 positive plasma cells infiltrate into various target organs,2 has been studied since indurative pancreatitis accompanying serum IgG4 increase was first reported in 2001. The prevalence of IgG4-related diseases is high in middle-aged men, but is dependent on the organs that are the target of infiltration. It is known that there is no a significant difference between men and women in the prevalence of IgG4-related salivary gland inflammation.3 In addition to the pancreas, an IgG4-related disease may be found in kidneys, salivary glands, lymph nodes, and retroperitoneum, and IgG4-related disease infiltration is reported to have been found in multiple organs in 60 to 90% of the diagnosed patients.4
An IgG4-related disease with lymphadenopathy generally accompanies infiltration into organs such as pancreas, kidneys, and salivary glands. Of the 114 cases of IgG4-related disease patients in which there was infiltration of multiple organs, 41 of the patients also had lymphadenopathy.5 However, IgG4-related disease with lymphadenopathy found in some patients showed one only symptom or sign of lymphadenopathy without an accompanied organ infiltration.6 Thus, for the diagnosis of a patient with the chief complaint of lymphadenopathy and no other specific symptoms, the possibility of IgG4-related disease with lymphadenopathy may need to be considered in addition to the possibility of an infectious disease by viral or bacterial infection, lymphadenitis by an autoimmune disease, or a neoplastic lesion such as Hodgkin's lymphoma and non-Hodgkin's lymphoma. We herein report a case in which a lymph node enlargement patient was diagnosed with IgG4-related disease with lymphadenopathy.
Patient: 72-year-old man
Chief complaint: Complained of left lymph node enlargement since two months before the visit
History: Hypertension, chronic obstructive lung disease
Present disease history: The patient stated that there had been a lymph node enlargement at the left cervical part since two months before the visit to our institution. The patient did not have a history of being bitten by an animal, consuming uncooked food, or any special travel. The patient did not complain of any particular symptoms such as fever by which tuberculosis or a neoplastic disease is suspected, or any weight change, fatigue, and night sweat.
Family history and social history: None of the patient's family members were affected by an infectious disease within last three months. None of the patient's direct family members had a history of a neoplastic disease. The patient was a non-smoker and was not taking any medicine.
Physical examination: The vital signs were blood pressure 116/70 mmHg, heart rate 98 /min, body temperature 36.5 ℃, and respiration rate 12 /min, which were all normal. The patient's consciousness was normal, but the patient had the complexion of a chronic illness. A lump of about 2 cm was palpated at the left cervical lymph node, which was relatively hard and moving. There was no oppressive pain during the palpation. No lymph node was palpated in other parts of the body other than the cervical lymph node. The abdominal physical examination did not show any enlargement of liver or spleen. The chest examination did not show any abnormalities in the breath sound and heart sound.
Laboratory findings: The peripheral blood test results were leukocyte level 4,800 /mm3 (normal, 4,000 to 10,800 /mm3), segmented neutrophil 55.8%, lymphocyte 24.4%, eosinocyte 10.1%, hemoglobin 9.7 g/dL (normal, 13 to 17 g/dL), platelet 84,000 /mm3 (normal, 130,000 to 400,000 /mm3), erythrocyte sedimentation rate 46 mm/hr (normal, 0 to 9 mm/hr), and C-reactive protein < 0.1 mg/dl (normal, < 0.5 mg/dl).
The general chemistry test results were Na 129 mEql/L (normal, 137 to 145 mEql/L), K 4.36 mEql/L (normal, 3.7 to 5.0 mEql/L), Cl 104.5 mEql/L (normal, 99 to 109 mEql/L), total protein 10.47 g/dL (normal, 6.5 to 8.0 g/dL), albumin 2.13 g/dL (normal, 3.8 to 5.2 g/dL), AST 25 IU/L (normal, 10 to 36 IU/L), ALT 5 IU/L (normal, 7 to 38 IU/L), total bilirubin 0.44 mg/dL (normal, 0.2 to 1.3 mg/dL), blood urea nitrogen 18.5 md/dl (normal, 8 to 20 md/dl), creatinine 1.52 mg/dl (normal, 0.51 – 1.17 md/dl), LDH 213 IU/L (normal, 200 – 450 IU/L), CPK 21 U/L (normal, 0 to 170 U/L), and uric acid 5.59 mg/dl (normal, 2.6 – 7.2 mg/dl).
Special blood test findings: The autoimmune antibody test showed a positive antinuclear antibody reaction (> 1:320), a negative anti-double stranded deoxyribonucleic acid antibody reaction (< 1:5), a negative anti-myeloperoxidase antibody reaction (7.4), a negative anti-proteinase3 antibody reaction (53.8), and a negative anti-GBM antibody reaction (< 0.2). Other findings were serum C3 27 mg/dl (normal, 90 – 180 mg/dl), C4 12 mg/dl (normal, 10 to 40 mg/dl), IgG level 4310 mg/dl (normal, 700 to 1600 mg/dl), and serum IgG4 level 340 mg/dl or higher (normal, 3.92 to 86.40 mg/dl).
The protein electrophoresis test performed with the serum and the urine showed polyclonal gammopathy with B2-microglobulin level of 17.6 mg/L (normal, 0.7 to 1.8 mg/L).
Imaging test findings: The cervical CT showed that multiple bilateral lymph node enlargements (1 to 2 cm) were found at both cervical lymph nodes (level I – V) (Fig. 1A). The chest CT showed multiple enlargements of bilateral supraclavicular lymph nodes, bilateral axillary lymph nodes, and mediastinal lymph nodes. The abdominal CT showed multiple enlargements of bilateral inguinal lymph nodes and bilateral iliac lymph nodes. Enlargement of the liver and the spleen was not verified.
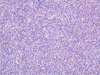
Biopsy: An incision biopsy was performed at the left cervical lymph node (1.3 cm). The biopsy showed lymphoplasmacytic infiltration. The IgG4 immunohistochemistry showed an IgG4 positive plasma cell level of 100 / High-power field (HPF) or higher (Fig. 2, Fig. 3).
Treatment and catamnesis: The patient was administered with prednisolone 25 mg/day for one week after being diagnosed with an IgG4-related disease. Then, the patient was administered with prednisolone 20 mg/day for the following eight weeks, prednisolone 15 mg/day for the following eight weeks, and prednisolone 10 mg/day for the following eight weeks, as the steroid dosage was gradually reduced. The chest CT performed after the administration showed no change in the lymph node enlargement. The prednisolone administration was increased again to 20 mg/day for five weeks, and then the chest and cervical CT were performed to evaluate the reaction (Fig. 1B). In comparison with the previous CT result, a significant size reduction of the lymph node enlargement was found. Prednisolone 10 mg/day is continuously administered at present, and the patient does not show any particular side effect during the treatment.
IgG4-related disease, which is a disease caused by the infiltration of IgG4 positive plasma cells into various target organs, is characterized by the infiltration into multiple organs including the pancreas, the kidneys, and the salivary glands.2 The basic requirements of the diagnosis of an IgG4-related disease are the serum IgG4 level test and the biopsy of affected organs, and radiological tests may also be performed depending on the affected organs.2 As the name implies, many of the IgG4-related disease patients show an increase in their serum IgG4 level. According to a report, 86% of 114 IgG4-related disease patients showed a serum IgG4 level higher than 135 mg/dl, the normal upper limit.5 Another study showed that the IgG4 level was increased as the number of affected organs was increased.7 However, even when the serum IgG4 level is within the normal range, an IgG4-related disease may be diagnosed with reference to the ratio of IgG4 plasma cell/HPF. The IgG4 plasma cell/HPF ratio, which enables an IgG4-related disease to be diagnosed on the basis of the biopsy result, is dependent on the affected organs.3 Since the IgG4 plasma cell/HPF ratio, which enables the diagnoses of an IgG4-related disease, is dependent on the affected organs, some researchers employ the ratio of IgG4 plasma cell/IgG plasma cell as the reference for the diagnosis. If the ratio of IgG4 plasma cell/IgG plasma cell is higher than 40% in all the organs, an IgG4-related disease may be diagnosed.8
In the present case, an autoimmune antibody test and a serum complement test were performed to differentiate systemic lupus erythematosus and Sjogren syndrome, which may also accompany lymph node enlargement. The results were a positive antinuclear antibody reaction (> 1:320) and a positive Anti-myeloperoxidase antibody reaction, serum C3 27 mg/dl, and C4 12 mg/dl. However, the patient had neither the systemic symptoms that may accompany systemic lupus erythematosus such as rash, arthralgia, and canker, nor the symptoms of Sjogren syndrome such as ophthalmoxerosis and xerostomia. Therefore, for the differential diagnosis of a neoplastic lesion such as Hodgkin's lymphoma and non-Hodgkin's lymphoma or an infectious disease by Epstein-Barr virus, a biopsy was performed at the left cervical lymph node. The biopsy results were IgG4 positive plasma cell level of 100 /HPF or higher and IgG4 plasma cell/IgG plasma cell ratio of 60% or higher, and thus an IgG4-related disease with lymphadenopathy was diagnosed.
Since IgG4 is unable to fix a complement in a typical pathway to precipitate an antibody in contrast to IgG1 and IgE,9 studies are still conducted on the correlation between the actual contribution of IgG4 to the pathogenesis of an IgG4-related disease and the autoimmune antibodies such as antinuclear antibody and antineutrophil cytoplasmic antibody. A decrease of C3 and C4 has been reported in about 56 to 78% of the IgG4-related disease patients, as in the present case.9
The treatment of an IgG4-related disease is based on steroids. The initial treatment dosage is generally prednisolone 0.6 to 1.0 mg/kg/day.10 The reaction to the treatment is evaluated by referring to the improvement of patient's symptoms, size change or functional improvement of the organs into which IgG4 plasma cells are infiltrated, and the decrease of serum IgG4 level. Some patients show improvements in just a few weeks, but others show no reaction to the treatment.2 For patients showing no reaction to steroids, the fibrosis may be irreversible. For patients having no reaction to steroids or the patients to whom a steroid cannot be administered, the use of an immunosuppressant such as rituximab as a secondary drug may be considered.11
Currently, the prognosis of IgG4-related disease has not been clearly identified. Some patients are completely healed without any special treatment, but it has been reported that relapse is common in many patients, as the disease turns into a type of chronic disease. If not treated after diagnosis, the IgG4-related disease may be accompanied by systemic symptoms such as aortic aneurysm and dissection and biliary obstruction, significantly increasing the mortality.12
In the case of a patient with lymph node enlargement, as in the present case, the possibility of an infectious disease by viral or bacterial infection, an autoimmune disease, and a neoplastic lesion may be generally considered,1 but IgG4-related disease with lymphadenopathy may also cause lymph node enlargement. IgG4-related disease with lymphadenopathy often causes lymphadenopathy at the lymph glands close to a target organ. When this occurs to the lymph nodes of the head and neck, Mikulicz's disease and Riedel's thyroiditis are commonly accompanied.13 However, since IgG4-related disease with lymphadenopathy may cause lymph node enlargement without affecting an organ in some patients,6 consideration of IgG4-related disease with lymphadenopathy is necessary to diagnose a patient having the isolated symptom of lymph node enlargement without dacryoadenitis or thyroiditis. Currently, the general treatment of an IgG4-related disease is based on steroids. If there is no reaction to the steroid-based treatment, the use of an immunosuppressant such as rituximab is considered as a secondary drug.11 In the present case, prednisolone was administered for six months by gradually decreasing the dosage, but no particular change was found in the reaction evaluation. At this point, the dosage of prednisolone was increased again, and a decrease in the lymph node enlargement was verified in the reaction evaluation. This indicates that an increased dosage of steroid may be attempted even though no change is found in the reaction evaluation following an initial steroid-based treatment. Further studies should be conducted to address this issue.
The present case report is about a patient who visited our institution with the chief complaint of cervical lymph node enlargement and was diagnosed with IgG4-related disease with lymphadenopathy (Type I–Multicentric Castleman disease-like) through a histological examination. We report the case herein because the cervical CT showed a significant decrease in the lymph node enlargement after a continued steroid-based treatment.
Figures and Tables
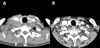 | Fig. 1Fig. 1A. Initial neck CT(Computed Tomography) showed multiple cervical lymph node enlargement, Fig. 1B. Post-steroid treatment image (The size of the cervical lymph node decreased after 8 month steroid trial) |
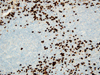 | Fig. 3Histological findings in Lt. cervical LN biopsy specimen, Interfollicular and perisinusoidal infiltration of small and large lymphocytes, admixed atrophic and hyperplastic germinal centers, large numbers of plasma cells showing IgG4 immunoreactivities (>100/HPF), Immunohistochemicalstaining × 200 |
References
3. Khosroshahi A, Stone JH. Treatment approaches to IgG4-related systemic disease. Curr Opin Rheumatol. 2011; 23:67–71.

4. Nizar AH, Toubi E. IgG4-related disease: case report and literature review. Auto Immun Highlights. 2015; 6:7–15.

5. Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol. 2010; 34:1812–1819.
6. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol. 2012; 22:1–14.

8. Ghably JG, Borthwick T, O'Neil TJ, Youngberg GA, Datta AA, Krishnaswamy G. IgG4-related disease: a primer on diagnosis and management. Ann Allergy Asthma Immunol. 2015; 114:447–454.

10. Shimosegawa T, Chari ST, Frulloni L, Kamisawa T, Kawa S, Mino-kenudson M, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011; 40:352–358.

11. Khosroshahi A, Bloch DB, Deshpande V, Stone JH. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. 2010; 62:1755–1762.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download