Abstract
Use of recombinant tissue plasminogen activator (rt-PA) for the treatment of acute cerebral infarction secondary to aortic dissection is challenging because of a narrow time window and potential life-threatening complications. An 80-year-old woman with right middle cerebral artery infarction was treated with rt-PA. Although she had no history, symptoms, or sign of aortic dissection, carotid CT angiography revealed aortic arch dissection. Mediastinal widening, which did not show on initial chest X-ray, developed on follow-up chest X-ray. This observation indicates that physicians should monitor patient symptoms for signs of aortic dissection during thrombolysis and perform chest X-ray or carotid angiography immediately after thrombolysis even if the patient has no symptoms or signs of aortic dissection on onset of acute cerebral infarction.
When intravenous thrombolytic agents are administered to patients with aortic dissection, it may result in aortic rupture and also dilated intramural hematoma, leading to stenosis or distal emobolism in the aorta and branch arteries. In the case of invasion of the origin of the aorta, hemopericardium or cardiac tamponade may occur, resulting in death.12 However, when a patient who has no previous aortic dissection is admitted to a hospital with distinct acute cerebral infarction symptoms, and in a situation where a prompt thrombolytic therapy has to be decided, there is no time to delay thrombolytic therapy with testing for a pre-existing aortic dissection. In several previous studies there were case reports of discovering an aortic dissection in the process of considering or administering a thrombolytic agent in patients with acute cerebral infarction.345 Among these cases, there were cases of symptoms showing aortic dissection at the time of admission and in some cases, the aortic dissection symptoms newly appeared or aortic dissection was diagnosed during the consideration or administration of thrombolytic agent. However, it is rarely reported that aortic dissection is discovered with a routine carotid angiography to find out the cause of cerebral infarction without newly developed aortic dissection symptoms at the time of admission and before and after the administration of thrombolytic agent. The authors report the discovery of aortic dissection from carotid CT angiography routinely performed after administering the intervenors thrombolytic agent in patients with acute cerebral infarction who had no symptoms of aortic dissection before or after thrombolytic therapy.
An 80-year-old woman came to the emergency room with a sudden onset of consciousness degradation and left hemiplegia that had occurred 32 minutes ago. The patient had no specific medical history except that she was taking an antihypertensive drug due to hypertension. At the time of admission, the vital signs were 110/70 mmHg blood pressure, 62 times/min pulse rate, 20 times/min respiratory rate and 36.5 degree Celsius body temperature. In the neurological examinations performed on admission, the level of consciousness was a hypnoleptic state, and the symptoms were gaze deviation to the right, dysarthria, left central facial paralysis, left hemiparesis (MRC grade I) and positive for left Babinski symptoms. The results of basic blood tests and electrocardiograms were all normal and it was confirmed that there was no medical history of contraindication for intravenous thrombolytic therapy.
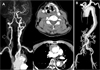
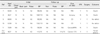
From brain CT scans performed 43 minutes after the onset of symptoms, it was confirmed that there was no cerebral hemorrhage or low shade areas. At 66 minutes after the onset, 34.2 ㎎ (0.9 ㎎/㎏) of the recombinant tissue plasminogen activator (rt-PA, Alteplase) was administered. After administration of rt-PA, consciousness deterioration and dysarthria were improved. Additionally, from the Diffusion-Weighted Brain MRI imaging performed a mild high signal intensity lesion along the cortex in the right cerebral artery region was found (Fig. 1A), and there was stenosis of the right cerebral artery and intracranial internal carotid artery stenosis in the brain magnetic resonance angiography (Fig. 1B). An intra-arterial thrombectomy was not performed because the brain lesion was large and there was no arterial occlusion. The chest X-ray performed 109 minutes after the onset was found to be normal (Fig. 2A). In the carotid CT angiography, which is routinely performed to determine the cause of cerebral infarction, we found that there was aortic dissection at the ascending aorta, right common carotid artery and aortic arch (Fig. 3A). Vital signs were all normal, and there was no pain in the chest, abdomen, side and back. Cardiac enzyme tests were normal and the transthoracic echocardiography showed overall hypokinesia and cardiac output rate of 39.11%. Aortic CT angiography showed aortic dissection from the origin of the aorta to the abdominal aorta and bilateral iliac arteries (Stanford A, DeBakey I) (Fig. 3B). A chest X-ray showed mediastinal widening that was not present in the initial X-ray (Fig. 2B). The patient underwent surgery for aortic dissection 12 hours after intravenous thrombolytic therapy and 3 months later, she is under rehabilitation with left upper and lower paralysis (MRC grade I).
Intravenous thrombolytic agents may cause aortic rupture and dilation of dissection in patients with aortic dissection.12 According to the newly revised American Clinical Practice Guidelines for Stroke, intravenous thrombolytic therapy is not recommended for patients with aortic dissection.6 In addition, routine chest X-ray is not recommended before the administration of the thrombolytic agent in order to prevent the delay of intravenous thrombolytic agent administration. However, in exceptional circumstances when there are clinical findings that suggest aortic dissection, it is stated that chest X-ray or CT angiography are recommended before the administration of the thrombolytic agent. Suspected symptoms of aortic dissection include weak pulse, hypotension, pain in the chest, abdomen, side, or back. Examination findings include mediastinal widening in the chest X-ray, and common carotid artery dissection (especially, on the right) in the carotid artery angiography.
Reports of newly discovered aortic dissection during the consideration or administration of intravenous thrombolytic agent in patients with acute cerebral infarction without a history of aortic dissection have been reported frequently, including in literature reviews.345 In some reports, chest pain, hypotension or weak pulse at the time of admission was a sign of aortic dissection. Some other reports suggested that a newly developed chest, abdomen, side or back pain, hypotension, weak pulse, or cardiac arrest after the admission led to the diagnosis of aortic dissection. In other reports, there were no clinical findings of suspecting aortic dissection at admission, but the aortic dissection was discovered through carotid angiography (carotid MR angiography, carotid Doppler ultrasound, or esophageal echocardiography) to determine the cause of cerebral infarction or autopsy.7891011 However, these reports did not mention if there were any clinical findings of suspecting aortic dissection after admission (Table 1). On the other hand, in this case the patient has no chest, abdomen, side, or back pain or decreased blood pressure and pulse at the time of admission and after admission. Aortic dissection was suspected based on the findings of a carotid artery CT angiograph that is performed routinely for patients with cerebral infarction. Finally, aortic CT angiography showed the Stanford A aortic dissection invading from the origin of the aorta to ascending aorta and the Debake I aortic dissection connected from ascending aorta to aortic arch, abdominal aorta and iliac artery. In addition, unlike other reports, in this case the change was observed in the chest X-ray. The mediastinal widening was newly present in the follow-up X-ray, but in the light of initial chest X-ray which was normal, it is thought that a slight premorbid asymptomatic aortic dissection caused the cerebral infarction and aortic dissection was exacerbated further due to the intravenous thrombolytic therapy or aortic dissection occurred as a rare complication of intravenous thrombolytic therapy in a patient with acute cerebral infarction.
When considering intravenous thrombolytic therapy in patients with acute cerebral infarction, careful observation should be made before and after the administration of thrombolytic agents if there are any suspected aortic dissection symptoms according to the American Clinical Practice Guidelines for Stroke. However, since the suspected aortic dissection symptoms may not appear especially in elderly patients, it may be necessary to perform a routine chest X-ray and carotid angiography after the intravenous thrombolytic therapy to perform an additional check on the aortic dissection symptoms.
Figures and Tables
Fig. 1
MR diffusion weighted images (A) and MR angiography (B) shows acute right hemispheric infarction with stenosis of the right middle cerebral artery and intracranial internal carotid artery (white arrows).
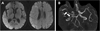
Fig. 2
Comparing with unremarkable initial chest X-ray (A), followed-up chest X-ray revealed mediastinal widening (B, black arrowheads).

Fig. 3
Carotid (A) and aorta CT angiography (B) shows that aortic dissection (Stanford A, DeBakey I) with the occlusion ofthe right common carotid artery (black arrows).
References
1. Marian AJ, Harris SL, Pickett JD, Campbell E, Fromm RE. Inadvertent administration of rtPA to a patient with type 1 aortic dissection and subsequent cardiac tamponade. Am J Emerg Med. 1993; 11:613–615.

2. Tsigkas G, Kasimis G, Theodoropoulos K, Chouchoulis K, Baikoussis NG, Aopstolakis E, et al. A successfully thrombolysed acute inferior myocardial infarction due to type A aortic dissection with lethal consequences: the importance of early cardiac echocardiography. J Cardiothorac Surg. 2011; 6:101.

3. Grupper M, Eran A, Shifrin A. Ischemic stroke, aortic dissection, and thrombolytic therapy--the importance of basic clinical skills. J Gen Intern Med. 2007; 22:1370–1372.

4. Hong KS, Park SY, Whang SI, Seo SY, Lee DH, Kim HJ, et al. Intravenous recombinant tissue plasminogen activator thrombolysis in a patient with acute ischemic stroke secondary to aortic dissection. J Clin Neurol. 2009; 5:49–52.

5. Ramalingam VS, Sinnakirouchenan R, Sudhakar S, Brasch AV. Acute ischemic stroke in aortic dissection: case report and review of literature. Indian J Med Sci. 2010; 64:385–389.

6. Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC, et al. Scientific Rationale for the Inclusion and Exclusion Criteria for Intravenous Alteplase in Acute Ischemic Stroke: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016; 47:581–641.

7. Fessler AJ, Alberts MJ. Stroke treatment with tissue plasminogen activator in the setting of aortic dissection. Neurology. 2000; 54:1010.

8. Villa A, Molgora M, Licari S, Omboni E. Acute ischemic stroke, aortic dissection, and thrombolytic therapy. Am J Emerg Med. 2003; 21:159–160.

9. Yamashiro S, Arakaki R, Kise Y, Kuniyoshi Y. Emergency operation for aortic dissection with ischemic stroke. Asian Cardiovasc Thorac Ann. 2014; 22:208–211.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download