Abstract
Objectives
Nowadays most infants on exclusively breast feeding have vitamin D deficiency due to the increase of breast feeding. However, domestic research lacks appropriate materials. Therefore, we researched practical clinical aspects of vitamin D deficiency related to breast milk feeding for infants who have a high amount of alkaline phosphatase (> 500 IU/L).
Methods
The subjects of the study were 31 infants with high alkaline phosphatase level. We tested with 25-hydroxycholecalciferol (25-OHD3), parathyroid hormone, calcium, ionized calcium, phosphorus in their blood and with a wrist x-ray. Then, we divided them into two groups of breast feeding and formula feeding and compared the results.
Results
Eighteen infants (58%) out of 31 infants that have high alkaline phosphatase were vitamin D insufficiency or deficiency, and 16 (100%) breast feeding infants of them showed vitamin D deficiency or insufficiency. However, only 2 (13%) of 15 formula feeding infants were at insufficiency. There was a correlation between alkaline phosphatase and 25-OHD3 concentration in multiple regression analysis, but no correlation in other variables was found in group of breast milk feeding infants. There was neither correlation between vitamin D concentration and alkaline phosphatase nor other correlated variables in the group of formula milk feeding infants.
Conclusions
In this study, there was a high probability of vitamin D deficiency in the breast feeding infants with a high alkaline phosphatase level. Therefore, it is considered to be worth utilizing alkaline phosphatase as a screening test for vitamin D deficiency or rickets for breast feeding infants.
Figures and Tables
Fig. 1
Association between alkaline phosphatase and 25-hydroxycholecalciferol in breast milk feeding infants
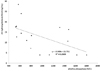
Fig. 2
Radiograph of wrist in a patient of asymptomatic rickets. there are cupping, spraying and fraying in ulna and radius. It is grade 2, moderate.

Table 2
Comparison of clinical profile between breast feeding infants and formula milk feeding infants (n=31)

References
2. Prentice A, Goldberg GR, Schoenmakers I. Vitamin D across the lifecycle: physiology and biomarkers. Am J Clin Nutr. 2008. 88:500S–506S.

3. Park SY, Park SW, Kang SK, Jun YH, Kim SK, Son BK, et al. Subclinical rickets in breastfed infants. Korean J Pediatr. 2007. 50:1188–1193.

4. Ladhani S, Srinivasan L, Buchanan C, Allgrove J. Presentation of vitamin D deficiency. Arch Dis Child. 2004. 89:781–784.

5. Wagner CL, Greer FR. American Academy of Pediatrics Section on Breastfeeding. American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008. 122:1142–1152.

6. Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. 2008. 122:398–417.

7. Ward LM, Gaboury I, Ladhani M, Zlotkin S. Vitamin D-deficiency rickets among children in Canada. CMAJ. 2007. 177:161–166.

8. Foo LH, Zhang Q, Zhu K, Ma G, Hu X, Greenfield H, et al. Low vitamin D status has an adverse influence on bone mass, bone turnover, and muscle strength in Chinese adolescent girls. J Nutr. 2009. 139:1002–1007.

9. Strand MA, Perry J, Jin M, Tracer DP, Fischer PR, Zhang P, et al. Diagnosis of rickets and reassessment of prevalence among rural children in northern China. Pediatr Int. 2007. 49:202–209.

11. Blok BH, Grant CC, McNeil AR, Reid IR. Characteristics of children with florid vitamin D deficient rickets in the Auckland region in 1998. N Z Med J. 2000. 113:374–376.
12. Shaw NJ, Pal BR. Vitamin D deficiency in UK Asian families: activating a new concern. Arch Dis Child. 2002. 86:147–149.

13. Lee HS, Lim BT, Lee HS, Hwang JS. Vitamin D Deficiency in Breastfed Infants. J Korean Soc Pediatr Endocrinol. 2008. 13:158–162.
14. Choi EH, Jung SH, Jun YH, Lee YJ, Park JY, You JS, et al. Iron Deficiency Anemia and Vitamin D Deficiency in Breastfed Infants. Korean J Pediatr Gastroenterol Nutr. 2010. 13:164–171.

15. Kliegman RM, Behrman RE, Jenson HB, Stanton BF. Nelson textbook of pediatrics. 2000. 18th ed. Philadelphia PA: W.B. Saunders.
16. Weisberg P, Scanlon KS, Li R, Cogswell ME. Nutritional rickets among children in the United States: review of cases reported between 1986 and 2003. Am J Clin Nutr. 2004. 80:1697S–1705S.

17. Haddad JG. Vitamin D-solar rays, the Milky Way, or both? N Engl J Med. 1992. 326:1213–1215.
18. Sampson HA, McCaskill CC. Food hypersensitivity and atopic dermatitis: evaluation of 113 patients. J Pediatr. 1985. 107:669–675.

19. Norman AW, Bouillon R, Whiting SJ, Vieth R, Lips P. 13th Workshop consensus for vitamin D nutritional guidelines. J Steroid Biochem Mol Biol. 2007. 103:204–205.

20. Kimlin MG, Schallhorn KA. Estimations of the human 'vitamin D' UV exposure in the USA. Photochem Photobiol Sci. 2004. 3:1067–1070.

21. Fox AT, Du Toit G, Lang A, Lack G. Food allergy as a risk factor for nutritional rickets. Pediatr Allergy Immunol. 2004. 15:566–569.

22. Seo JY, Kim C, Lee HW, Ahn YM. Eight cases of incidentally diagnosed as subclinical rickets. Korean J Pediatr. 2008. 51:812–819.

23. Kim SK, Kim YK, Cho AJ, Kim HR, Lim SE. Kim SK, editor. Current status of maternal and child health care. 2006 The survey on the national fertility, family health and welfare in Korea. 2009. Korea Institute for Health and Social Affairs;283.
24. Heinig MJ. Vitamin D and the breastfed infant: controversies and concerns. J Hum Lact. 2003. 19:247–249.

25. Gartner LM, Greer FR. Section on Breastfeeding and Committee on Nutrition. American Academy of Pediatrics. Prevention of rickets and vitamin D deficiency: new guidelines for vitamin D intake. Pediatrics. 2003. 111:908–910.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download