Abstract
Spontaneous rupture of the urinary bladder is a rare clinical entity, with the incidence reported as 1 in 126,000 hospital admissions. It is often associated with malignancy, inflammatory lesions, irradiation, calculus, diverticulum, binge alcohol drinking, continuous bladder irrigation, and neurogenic bladder. In rare instances, bladder rupture occurs without obvious causes. This rare clinical condition is difficult to diagnose because of vague symptoms. High index of suspicion is needed as the mortality rate is high if untreated. A 37-year-old woman with uncontrolled type 2 diabetes, was admitted to the emergency room complaining of progressive abdominal distension and discomfort. She had a past history of tubo-ovarian and bladder abscess, and had undergone multiple surgical operations. From ascites fluid study, she was diagnosed as spontaneous bladder rupture. A transurethral catheter was inserted and the symptoms and signs resolved. Bladder rupture, mimicking acute kidney injury of diabetic nephropathy was disclosed without surgery.
Spontaneous rupture of the urinary bladder is a rare clinical entity, with the incidence reported as 1 in 126,000 hospital admissions.1 It is often associated with malignancy, inflammatory lesions, irradiation, calculus, diverticulum, binge alcohol drinking, continuous bladder irrigation, and neurogenic bladder.1,2 In rare instances, bladder rupture occurs without obvious causes. Diagnosis of a spontaneous bladder rupture requires a high index of suspicion, as most patients initially present with nonspecific symptoms. This report described a 37-year-old woman with type 2 diabetes, who presented with progressive abdominal distension and discomfort with clinical manifestation of oliguric acute renal failure.
A 37-year-old woman with type 2 diabetes mellitus presented with progressive abdominal distension for 3 days. She has been diagnosed with type 2 diabetes 10 years ago and was on insulin therapy. She also had a past history of tubo-ovarian and bladder abscess, which developed after intrauterine device removal, five years ago. Left adnexectomy with right ovary wedge resection and partial cystectomy was performed. Five months after the surgery, adhesive ileus developed and she underwent adhesiolysis. One year after adhesiolysis, she was admitted again due to recurrent adhesive ileus and panperitonitis. A large amount of ascites with diffuse enhancement along the peritoneal lining was seen in abdominal computed tomography (CT). Explorative laparotomy documented pus like fluid collection in the pelvic cavity, and adhesiolysis was again performed.
On this admission, she complained of dyspnea, abdominal distension, oliguria and dysuria. Severe abdominal distension with a large fluid wave was detected during physical examination. However, peripheral edema was mild on both lower extremities. Initial blood pressure was 160/100 mmHg, respiration rate was 22 /min, heart rate was 124 /min and body temperature was 36.7℃. Laboratory data showed fasting blood glucose of 707 mg/dL, HbA1c of 12.1%, serum blood urea nitrogen of 41.6 mg/dL and serum creatinine of 2.2 mg/dL. Serum sodium was 120 mEq/L and potassium was 4.9 mEq/L. Liver function tests were all within normal ranges. Total protein and albumin were 8.4 g/dL and 4.5 g/dL, respectively. Complete blood cell count showed a white blood cell count of 12.8×103 /uL with segment neutrophil 82.8%, and a hemoglobin level of 9.8 g/dL. Urinalysis showed glucosuria and proteinuria. She was already accompanied with stage 4 diabetic nephropathy presenting and macroalbuminuria. The most recent laboratory data before this admission showed serum creatinine of 1.4 mg/dL. The posteroanterior chest radiograph showed neither pleural effusion nor cardiomegaly. Transthoracic echocardiogram showed an ejection fraction of 63.4% without wall motion abnormality.
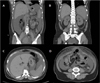
Abdominal CT showed large amount of ascites with focal ventral hernia of the small bowel loop, but there was no evidence of hydronephrosis (Fig. 1). Diagnostic paracentesis was performed which showed serum albumin-ascites gradient of 4.2 g/dL. Results of cultures and cytologic examinations of ascites were all negative for bacterial or fungal infection. 7 days after the admission, her glucose level was still uncontrollable and serum creatinine level increased up to 6.4 mg/dL. The urine volume decreased to less than 50 ml/day and the abdominal circumference was progressively increasing. Biochemistry of initially drained ascites was then performed in doubt of urine leakage and the result revealed a creatinine concentration of 10.6 mg/dL, which was nearly five times as high as the serum creatinine of 2.2 mg/dL.
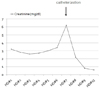
After insertion of an indwelling transurethral catheter, 2,300 mL of urine was drained, symptoms of abdominal distension and discomfort then subsided. Two days after transurethral catheter insertion, serum creatinine and urea nitrogen decreased to 0.8 mg/dL and 7.5 g/dL, respectively (Fig. 2). No abnormality was observed in urodynamic study and voiding cystourethrogram did not reveal any contrast leakage outside of the bladder wall. Follow up CT urography showed resolved ascites and diverticulum-like outpouching of the dome portion of the bladder; however, contrast leakage from the bladder was not detected (Fig. 3).
The patient was discharged with a diagnosis of spontaneous intraperitoneal rupture of the bladder. On hospital day 14, the patient was discharged with normal renal function with serum creatinine of 0.8 mg/dL and well controlled blood glucose level. Her weight reduced by 8 kg and the abdominal circumference decreased by 10 cm.
Because of vague symptoms, definite diagnosis of bladder rupture is difficult, and a high index of suspicion is required for diagnosis of this rare condition. Symptoms include abdominal pain, suprapubic tenderness, oliguria and newly onset ascites. When the usual factors such as cirrhosis, congestive heart failure, hypoproteinemic states and disseminated carcinomatosis cannot explain the cause of ascites, it is important to look for an alternative diagnosis. At first, this case was considered as rapid progression of previous diabetic nephropathy associated with newly developed ascites. Acute kidney injury can be accompanied with diabetic nephropathy from various causes including inflammations, infections, contrast-media, NSAID and other diabetic complications such as heart failure or foot ulcer. In this case, there was no sign of inflammation or infection to indicate acute kidney injury. Mild pitting edema was observed in the lower extremities, suggesting incompatible edema due to diabetic nephropathy with nephrotic range proteinuira and hypoalbuminemia; however, abdominal distension and ascites were aggravated with rapid elevation of creatinine level. Urine leakage into the peritoneal cavity due to bladder rupture may cause pseudo-renal failure, a condition in which renal function is normal with presence of elevated serum creatinine. Elevation of serum creatinine and urea is caused by peritoneal reabsorption of urinary ascites across the peritoneum, a condition that may be described as "inverted peritoneal auto-dialysis".3,4
Ratios of serum BUN/Cr more than 10.8 and ascites Cr/serum Cr more than 1.0 are two diagnostic indicators of bladder rupture.5 The ratios of this case were 18.9 and 4.82 respectively, which were compatible with bladder rupture. Detection of N-acetyl-beta-D-glucosaminidase (NAG), an enzyme from renal epithelial tubular cells to urine, can also be helpful in diagnosis of bladder rupture.3
The conventional CT protocol may or may not reveal the presence of bladder rupture because visualization of the rupture site on CT requires the bladder to be filled with fluid and under pressure.6 Therefore, CT cystography is indicated when bladder rupture is highly suspected. In this case, CT urography could not detect obvious leakage. This might be due to spontaneous closer of the perforation site after catheterization of the bladder prior to CT urography.
Accurate identification of bladder rupture for subsequent management is important. Delayed diagnosis and treatment may increase the patient's morbidity and mortality. The mortality rate associated with bladder rupture has been described as high, approximately 50% due to its complications including hyperkalemia, hyperuricemia, acidemia and sepsis.1 The mortality rate of bladder rupture can be elevated, when no prompt management is given.
It has been reported that catheterization might lead to remission of clinical manifestations of bladder rupture, particularly with small leaks.7 However, when either they repeat or large leaks of bladder rupture are observed, surgery for bladder perforation should be performed. Therefore, early diagnosis of bladder rupture is needed for a good prognosis. Also, as in this case, ascites and hyperuricemia also resolved after simple bladder catheterization.
Relationship between diabetes and non-traumatic bladder rupture was not obviously evaluated. Some cases of spontaneous bladder rupture have been reported in patients with diabetes. In these cases, susceptibility to infection in diabetes, especially urinary bladder and neurogenic bladder as a diabetic neuropathy, was explained as factors of bladder rupture.8,9 Furthermore, polyuria in hyperglycemia could also be a possible cause of bladder rupture in diabetes.4 In our case, we think that a previous poorly controlled blood glucose level may have contributed in part to development of spontaneous bladder rupture.
We present a case with spontaneous bladder rupture, which mimicked acute kidney injury of diabetic nephropathy with massive ascites in type 2 diabetes. Although cystogram and CT urogram did not reveal leakage from the bladder due to prior transurethral catheterization, elevated ratios of serum BUN/Cr and ascites Cr/serum Cr lead to diagnosis of bladder rupture. The possible cause of the bladder rupture is thought to be multiple surgical operations on internal pelvic organs and recurrent episodes of ileus. Furthermore polyuria caused by recent hyperglycemia also might contribute to this condition. Although one case of spontaneous bladder rupture associated with polyuria was reported in heavy drinking state,10 it had not been reported in patients with uncontrolled diabetes in Korea. Bladder rupture could be considered as a possible factor of acute kidney injury and ascites, especially in patient with history of previous abdominal surgery. High index of suspicions with early diagnosis and proper management is needed for better prognosis.
Figures and Tables
Fig. 1
(A-D) A abdominal computed tomography (CT) shows a large amount of ascites and focal ventral hernia of the small bowel loop, without hydronephrosis. The right and left kidney sizes are within normal limits, measuring 10.8 cm and 10.5 cm, respectively.
References
1. Bastable JR, De Jode LR, Warren RP. Spontaneous rupture of the bladder. Br J Urol. 1959. 31:78–86.

2. Khan AU, Stern JM, Posalaky Z. Vesical necrosis associated with acute bladder overdistention. Urology. 1982. 19:197–199.

3. Horino T, Okazaki M, Nishikawa H, Takao T, Taniguchi Y, Morita T, et al. A case with spontaneous bladder rupture mimicking acute kidney injury. Clin Nephrol. 2009. 72:391–393.
4. Manna R, Mirk P, Sallustio G, Brisinda G, Izzi D, La Regina M, et al. Hypercreatininemia and hyperglycemia: diabetic nephropathy or "inverted peritoneal auto-dialysis"? Clin Nephrol. 2005. 63:167–169.

5. Sullivan MJ, Lackner LH, Banowsky LH. Intraperitoneal extravasation of urine. BUN-serum creatinine disproportion. JAMA. 1972. 221:491–492.

6. Chan DP, Abujudeh HH, Cushing GL Jr, Novelline RA. CT cystography with multiplanar reformation for suspected bladder rupture: experience in 234 cases. AJR Am J Roentgenol. 2006. 187:1296–1302.

7. Mulkey AP Jr, Witherington R. Conservative management of vesical rupture. Urology. 1974. 4:426–430.

8. Mardani M, Shahzadi M, Rakhshani N, Rahnavardi M, Rezvani J, Sharifinejad A. Spontaneous perforation of urinary bladder secondary to Candida cystitis: acute abdomen of urologic origin. Surg Infect (Larchmt). 2008. 9:525–527.

9. Comiter CV, McDonald M, Minton J, Yalla SV. Fungal bezoar and bladder rupture secondary to candida tropicalis. Urology. 1996. 47:439–441.

10. Lee MH, Jung JY, Beak DH, Park YS, Yoo TK, Sung SA, et al. A case of sponataneous bladder rupture after a bout of heavy drinking. Korean J Med. 2009. 76:370–373.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download