Abstract
Objectives
The objective of this study was to assess the efficacy of the Korean fracture-risk assessment tool (FRAX) model for routine application in women who had a general check-up for bone mineral density (BMD).
Methods
This retrospective study was conducted at a university hospital and comprised 343 patients, whose BMD and clinical risk factors were assessed for FRAX calculation. The 10-year probabilities of hip and major osteoporotic fractures were compared with the result of the FRAX® tool (http://www.shef.ac.uk/FRAX, web version 3.5) applied to Korean models developed at the World Health Organization Collaborating Center with or without femoral neck bone mineral density.
Results
The T-score gradually decreased with increasing age. Additionally, the 10-year probability of a major osteoporotic fracture increased with age. However, the probability of hip fracture showed no correlation with age if BMD was not included in the estimation.
Conclusion
Previous report on patients whose probability of a proximal femoral fracture were calculated using Korean FRAX models produced a higher score than our data because our data involved a general population. A larger general population is needed to confirm the Korean FRAX model. However, our data provide information for physicians to assess the Korean FRAX model in the general female population.
Osteoporosis is a deficiency in bone density that increases the risk of fractures. After menopause, osteoporosis is carefully evaluated and counseled by physicians. The World Health Organization (WHO) recommended the definition of osteoporosis to be a bone mineral density (BMD) using dual-energy X-ray absorptiometry (DXA) that lies 2.5 standard deviations (SD) or more below the mean value for young healthy women (T-score ≤ -2.5 SD).1
The International Society for Clinical Densitometry (ISCD) has also developed Official Positions to assist physicians in the use of BMD assessed by DXA to diagnose osteoporosis. We have already revealed that the frequency of osteoporosis diagnosed in postmenopausal women using the WHO criteria is much lower than that using the 2007 ISCD Official Positions.2 The WHO criteria are more liberal than the ISCD Official Positions. In 2008, the WHO Metabolic Disease Group focused on developing a fracture-risk assessment tool (FRAX) using clinical risk factors combined with femoral neck BMD to predict 10-year fracture risk. The FRAX model is focused on country-specific risk factors. After June 2010, the Korean FRAX model was applied. Previous reports regarding FRAX included hip fracture and vertebral fracture patients instead of a general population.1,3
By integrating these risk factors, WHO suggested the FRAX tool to compute the 10-year probability of an osteoporotic fracture. The advantage of the FRAX tool is that it can be used without BMD measurement and can make ethnic-specific adjustments. In fact, it has been used to determine thresholds for initiating treatment of osteoporosis in a Japanese setting. However, few studies have evaluated the application of FRAX models in the Korean population. The 10-year probabilities of hip and major osteoporotic fractures were compared with the result of the FRAX® tool (http://www.shef.ac.uk/FRAX, web version 3.5, Fig. 1) applied to the Korean model developed by the WHO Collaborating Center with or without femoral neck BMD.
The objective of the present study was to assess the efficacy of the Korean FRAX model in women who had a general check-up for BMD.
The present study was conducted at a university hospital in Bucheon, Korea. All women who had visited the department of obstetrics and gynecology (OBGY) and were measured for BMD during the period from January 2010 to December 2011 were enrolled. During that period, 466 patients were measured for BMD in the OBGY department, but 123 were excluded from the present study because of missing data. Thus, the present retrospective study comprised 343 patients, whose BMD as well as clinical risk factors were assessed for FRAX calculation.
Information on each patient's background such as age, body weight, height, coexisting diseases, and drug prescriptions was obtained from the hospital information system. Additionally, detailed information concerning risk factors of osteoporosis was obtained by telephone interview with a trained research assistant. The risk factors included age, height, body weight, previous fracture history as an adult, parental history of hip fracture, current smoking, use of systemic corticosteroids, rheumatoid arthritis, secondary osteoporosis (e.g., type I diabetes, osteogenesis imperfecta as an adult, untreated long-standing hypethyroidism, and hypogonadism or premature menopause [< 45 years]), and alcohol intake of more than three units daily (1 unit: beer [285 mL], a single measure of spirits [30 mL], a medium-sized glass of wine [120 mL]), or 1 measure of an aperitif [60 mL]). A prior fragility fracture was defined as a major osteoporotic fracture before BMD testing. Prolonged corticosteroid use was defined as over 90 days of medication dispended in the year prior to BMD evaluation at a mean prednisolone-equivalent dose of ≥ 5 mg per day. Weight and height recorded at the time of DXA evaluation were used. BMD was evaluated at the L1-4 lumbar spine and the femoral neck using the same DXA machine (GE Lunar Prodigy, GE Lunar Corp., Madison, WI, USA).
All results are expressed as the mean ± SD, unless otherwise stated. Fisher's exact test was used to compare frequencies. A paired t-test was used to analyze differences according to inclusion of BMD values. Statistical correlation between ages and risk factors was evaluated using the one-way analysis of variance (ANOVA) or the Kruskal-Wallis test. Each result was analyzed using PASW Statistics software (version 17.0; SPSS Inc., Chicago, IL, USA). A P-value < 0.05 was considered statistically significant.
When research assistants interviewed patients via telephone, informed consent was obtained.
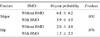
Three hundred forty-three women between the ages of 41 and 85 years were enrolled in the present study. The clinical risk factors for fracture are presented in Table 1. Data on T-score at the femoral neck were calculated to be -1.007 ± 1.392 (Table 1, Table 4).
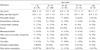
The 10-year probabilities of major osteoporotic and hip fractures using the Korean model are shown in Table 2. A paired t-test presented the differences of major osteoporotic fracture risk according to inclusion of BMD values. However, the differences of hip fracture risk according to inclusion of BMD were not significant.
Table 3 shows the clinical risk factors according to age. Among the age-groups, clinical risk factors showed no significant difference.
Table 4 shows T-score of femoral neck in the present study subjects. The T-score decreased with increasing age except for the age group ≥ 80 years.
Figure 2 shows fracture probabilities in the Korean FRAX model according to age. The data were analyzed by Kruskal-Wallis test. The 10-year probabilities of major osteoporotic fractures increased with age regardless of whether BMD was included in the estimation of risk (without BMD, P < .001; with BMD, P < .001). If BMD was not included in the estimation, the probability of hip fractures showed no correlation with age (without BMD, P < .001; with BMD, P < .001).
Elderly people are prevalent in Korea, and one of the most serious causes of mortality and morbidity is fracture disease. Osteoporosis is an important cause of fracture in the elderly. The Health Insurance System has revealed that Korean osteoporotic patients are predominantly female (89.9%).4 Only 61.6% of cases diagnosed with osteoporosis are managed by drugs,4 of these, 43.2% are males, and 63.7% are females. Postmenopausal women were more likely to have an examination for diagnosis of osteoporosis and to receive conservative management.5 Thus, earlier diagnosis of osteoporosis and evaluation of osteoporotic risk factors are important for public health. The 25(OH) vitamin D3 levels in postmenopausal women of the Bucheon area were low; thus, studies to elucidate and assess the dietary intake of vitamin D3 in menopausal women of this region will be beneficial.6 The history of previous child birth and/or miscarriages did not affect BMD; however, further prospective multicenter studies regarding obstetric history should be considered for prevention of osteoporosis before menopause.7 When the WHO threshold for postmenopausal women was applied, the frequency of osteoporosis diagnosed was 22.8% at the lumbar spine, 30.4% at the femoral neck, and 38% in at least one of the evaluated sites.2 Several previous studies have developed models to predict fracture risk from the combination of clinical risk factors and BMD. Including all risk factors, WHO provides a model for assessment of fracture probability in men and women.
The FRAX model uses data derived from nine cohorts worldwide, including North America, Europe, Asia, and Australia, and has been validated in 11 independent cohorts with a similar geographic distribution.2 The FRAX® tool defines fracture risk more accurately than does the use of BMD alone.8
Postmenopausal women from the general population were evaluated based on models from Japan, Turkey, and China.9 The Japan model is suitable for Koreans, but these general population data produced higher scores for fracture probabilities than our data. Previous data on patients with proximal femoral fracture probabilities calculated using the Korean FRAX model produced higher scores than our data because our data involved a general population.3 In individuals aged 70~79 years, the combination of BMD and FRAX in our study produced a higher probability of major osteoporotic fractures and hip fractures. We recommend BMD evaluation age for the 70- to 79-year age group.
There were some limitations to the current study. First, present study were single center, single department (OBGY) study, so the distribution of clinical risk factors might not represent that of general population. Second, this study has a limitation stemming from its small sample size. Finally, limitation of this study included the lack of specific information about the size and shape of the spaxel. A cohort study with a larger general population is needed to confirm the Korean FRAX model; however, our data provide information for physicians to assess the Korean FRAX model in the general female population.
Figures and Tables
 | Fig. 2Ten-year probabilities using Korean fracture-risk assessment tool (FRAX) model according to age. (A) Major osteoporotic fracture, (B) Hip fracture. (*,†,‡,§P < 0.001 by Kruskal-Wallis test) |
Table 2
Ten-year fracture probabilities calculated using Korean fracture-risk assessment tool (FRAX) model
References
1. So GY, Park KH, Yoon DH, Ryu JH, Choi YS. Feasibility of FRAX for prediction of osteoporotic vertebral fractures in Korea. Asian Spine J. 2012. 6:22–28.

2. Kim TH, Lee HH, Chung SH. A difference of bone fracture rate and frequency to have determined in diagnosis standards. Osteoporosis. 2010. 8:266–270.
3. Ji HM, Won YY, Park MJ. Clinical efficacy of Korean FRAX® model in patients with hip fracture. Osteoporosis. 2011. 9:170–174.
4. Jang S, Park C, Jang S, et al. Medical service utilization with osteoporosis. Endocrinol Metab. 2010. 25:326–339.

5. Kim TH, Lee HH, Chung SH, Park HS. Differentiation in the management of osteoporosis between premenopausal and menopausal women. J Korean Soc Menopause. 2011. 17:21–26.
6. Chung SH, Kim TH, Lee HH. Relationship between vitamin D level and bone mineral density in postmenopausal women from Bucheon area. J Korean Soc Osteoporos. 2009. 7:198–202.
7. Kim TH, Lee HH, Chung SH, Jung EA. Relationship between history of pregnancies and bone mineral density. Osteoporosis. 2011. 9:89–92.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download