Abstract
Background and Objectives
The harmonic scalpel using the ultrasonic energy is able to grasp and divide tissue while sealing small vessels in narrow operating fields. The aim of the present study was to evaluate the usefulness of the harmonic scalpel in thyroid surgery.
Materials and Methods
This study was performed for 247 patients who underwent thyroidectomy. According to the use of harmonic Scalpel, the patients could be divided into two groups: the conventional technique (CT) group of knot tying and the harmonic scalpel (HS) group.
Results
For hemithyroidectomy, operation time and hospital stay were shorter in the HS group compared with the CT group (p<0.05). For total thyroidectomy with central neck dissection (CND), operation time, total drainage volume, drain removal date, and hospital stay were significantly reduced in the HS group (p<0.05). Among the patients who underwent total thyroidectomy with CND with the HS, one patient (2.9%) showed transient recurrent laryngeal nerve palsy. Transient hypoparathyroidism showed significantly lower incidence in the HS group (p<0.05).
The standardized thyroid surgery developed by Theodor Kocher and Theodor Billroth, the pioneers of thyroid surgery, has not undergone a major change in operative technique in the last century.1) Even if alternative surgical methods in thyroid gland, including endoscopic surgery or recurrent laryngeal nerve stimulation, have been tried during the last decade, they have not been widely accepted.2,3) Recently, there was a major development in the device using ultrasonic energy and it has been using for various surgeries, especially by laparoscopists.
The ultrasonically activated scalpel (harmonic scalpel) that uses high frequency mechanical energy makes it possible to cut and coagulate tissues and vessels simultaneously, without the need of knot tying.4) Therefore, this device might be useful to reduce operation time and hypoparathyroidism since in thyroid surgery that requires a large amount of knot tying and may impair the pedicle of parathyroid gland during knot tying.
The present study was conducted to evaluate the strength and weakness of the harmonic scalpel by comparing two groups that used the conventional technique (knot tying) and the harmonic scalpel in thyroid surgery.
We performed the hemithyroidectomy and total thyroidectomy in 286 patients with thyroid benign and malignant nodules, from January 2006 to June 2007. Among them, thirty-nine patients who were associated with toxic goiter and who underwent complete thyroidectomy or total thyroidectomy with lateral neck dissection were excluded. Thus, a total of 247 patients were included in the study population. Institutional ethical board approval and preoperative informed consent from all patients were obtained. All patients were explained in the price and functions of harmonic scalpel and then harmonic scalpel was used only in patients with permission to use it.
According to the use of harmonic scalpel, the patients could be divided into two groups, prospectively: the conventional technique (CT) group of tying and knots (hemithyroidectomy, n=100; total thyroidectomy, n=52) and the harmonic scalpel (HS) group (hemithyroidectomy, n=60; total thyroidectomy, n=35). All patients were examined about age, gender, operation time, postoperative drainage (duration and volume), hospital stay, and postoperative complication including bleeding, recurrent laryngeal nerve palsy, and hypoparathyroidism. Operation time was defined as the time between skin incision and skin closure. Vacuum drains were placed in all patients, and postoperative drainage was estimated every morning. When the drainage volume was less than 20 mL per 24 hours, the suction device was removed. All patients who were removed suction device were discharged from the hospital the next day. In the patients who underwent total thyroidectomy, a series of serum calcium levels were obtained every postoperative day until patients were discharged. All the patients with serum calcium levels of less than 2.10 mmol/L (reference range, 2.10-2.60 mmol/L) during the first 3 postoperative days were considered as having hypocalcemia and received oral calcium carbonate and vitamin D3 supplementation. If serum calcium levels returned to normal within 6 months, hypoparathyroidism was classified as transient, and in the other cases, it was classified as permanent.
All patients had the same anesthetic and hospital care and the patients were positioned and draped in the conventional manner. About 5 cm incision was made over the level of the thyroid isthmus. After elevation of subplastysmal flaps, the strap muscles were separated in the midline and laterally reflected. The superior and inferior thyroid vessels were then divided either with the harmonic scalpel with the CS-14C handpiece (Harmonic Synergy Curved Blade, Ethicon Endosurgery Inc., Cincinnati, OH, USA) or with conventional knot tying and electric cauterization. The only small vessels in the ligament of Berry were clamped with clips in both groups. After that, the wound was irrigated and closed using absorbable suture material to approximate strap muscle, platysmal layer, and subcutaneous layer. Then, the skin was sutured with non-absorbable material.
The indications of hemithyroidectomy were benign nodule and single micropapillary carcinoma (1 cm and less) without nodal metastasis or extrathyroid spread. In the other malignant nodule, total thyroidectomy with central neck dissection (level VI) was performed.
Hemithyroidectomy and total thyroidectomy groups were divided into two groups using either the HS or conventional knot tying. All the patients who were to undergo surgery during the study period were selected using simple random sampling. Each group was analyzed to estimate the usefulness of HS. Statistical analysis was performed using the independent t-test, the Pearson χ2 test, and Fisher's exact test to compare the series. For all tests, a probability of less than 0.05 was accepted as statistically significant. All statistical analyses were done with SPSS software version 12.0 (SPSS Inc., Chicago, IL, USA).
All groups were similar regarding age and sex, and there were no intraoperative complications. For hemithyroidectomy, there was no significant difference according to drainage volume and drain removal date between the 2 groups. However, operation time (p=0.006) and hospital stay date (p=0.048) were shorter in the HS group compared with the CT group (Table 1).
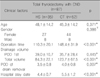
For total thyroidectomy with central neck dissection, there was no difference of drainage volume of first postoperative day between the 2 groups. However, operation time (p<0.001), total drainage volume (p<0.001), drain removal date (p=0.007), and hospital stay date (p<0.001) were significantly different between them (Table 2). There was no significant difference according to tumor volume and malignancy between the 2 groups.
In terms of postoperative complication, postoperative hemorrhage and transient recurrent laryngeal nerve palsy occurred in one patient each (1%) who underwent hemithyroidectomy with the CT. Among the patients who underwent total thyroidectomy with central neck dissection (CND) with the HS, only one patient (2.9%) showed transient recurrent laryngeal nerve palsy. The incidences of these complications were too low to reach statistical significance, with the exception of transient hypoparathyroidism that showed significantly lower incidence in the HS group than in the CT group (p=0.009) (Table 3).
The meticulous hemostasis is important in thyroid surgery because the thyroid gland has an extensive vascular network. Especially, the control of small vessels around recurrent laryngeal nerve and parathyroid gland on preserving their function is a time-consuming step in thyroid surgery. To date, various techniques, including knot-tying, electric cauterization and HS to cutting and hemostasis in surgery have been used. Among them, knot-tying has been the most frequently used technique and relatively safe and reliable ligation without injury of adjacent structure. However, it requires good skill and has a tendency to delay the operation time. On the other hand, electrical cauterization can reduce the operation time but usually injure the adjacent tissue and its use around a nerve is dangerous. However, the use of ultrasonic energy recently made it possible to cut tissue and perform hemostasis at the same time with minimal injury to the adjacent tissue.4)
The HS using the ultrasonic energy has been used for cardiac, abdominal, and gynecologic surgery because of its ability to access narrow operating fields.5-8) In addition, the usefulness of the HS in thyroid surgery has been reported and it provides an alternative method to conventional hemostasis technique.9-16) All these studies have shown that the HS is a safe method for controlling bleeding and shortens the operation time, same as our study. While a majority of studies used only the HS, we used hemoclips for small vessels around the ligament of Berry because of the relatively blunt tip of HS. In case of the patients who underwent total thyroidectomy with CND and had a plan of postoperative radioactive iodine ablation, the complete resection of thyroid tissue is a very important prognostic factor. Therefore, the exclusive use of HS may result in incomplete removal of thyroid tissue. In addition, since there is a recurrent laryngeal nerve near the ligament of Berry, the blunt tip of HS may make a recurrent laryngeal nerve palsy. In the studies that described postoperative recurrent laryngeal nerve palsy in detail, the incidence rate of transient injury of recurrent laryngeal nerve was from 3% to 10.5%.11-13,16) In our study, transient recurrent laryngeal nerve palsy was observed in one case (2.9%) of total thyroidectomy with CND group, using the HS, and it may result from the handling of HS around the ligament of Berry. However, except for this weak point of HS, the reduction of operation time, postoperative drainage, and hospital stay was shown in a majority of previous studies.
In our study, there was a significant difference of the incidence of transient hypoparathyroidism between HS and conventional technique groups in cases of total thyroidectomy with CND. Although a similar study, which transient hypoparathyroidism was reduced in the cases that used the HS, was reported, a majority of the other studies have reported that the difference of transient hypoparathyroidism was not statistically significant.15) The discrepancy between these studies may result from the difference of time for estimating postoperative serum calcium. Controversy exists concerning the best time for estimation of serum calcium in predicting postoperative transient or permanent hypoparathyroidism.17) Some previous studies have suggested that decreasing serum calcium levels within the first 48 hours after surgery may be a predictor of postoperative hypoparathyroidism and the other study described serum calcium level at the first 72 hours after surgery as a better predictor.17-20) Therefore, we routinely measured serum calcium levels during 72 hours after surgery and this may explain higher incidence of transient hypoparathyroidism and significantly different incidence of transient hypoparathyroidism between HS and CT groups in contrast with the previous studies.12,13,16) Transient hypocalcemia may result from mechanical force or perioperative hemodilution.21) However, hypocalcemia within the first 3 days postoperatively may be caused by the stretching or heating during operation.17) Consequently, our results seem to support that the low heat generation and gentle cutting without stretching by the HS may lead to reduce the injury of parathyroid gland vascularity.
We have demonstrated the weak and strong points of the HS. Even if the HS is expensive, the reduced operation time and hospital stay without increased postoperative complications actually might make it cost-effective. However, since the exclusive use of the HS may make an incomplete resection of thyroid gland and a recurrent laryngeal nerve injury, especially around Berry's ligament, the exceptional use of hemoclip or knot tying may be important in some cases.
Figures and Tables
Table 1
Difference between harmonic scalpel group and conventional technique group according to clinical factors in patients who underwent the hemithyroidectomy
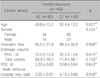
Table 2
Difference between harmonic scalpel group and conventional technique group according to clinical factors in patients who underwent total thyroidectomy with central neck dissection
References
1. Becker WF. Presidential address: Pioneers in thyroid surgery. Ann Surg. 1977. 185(5):493–504.
2. Chowbey PK, Mann V, Khullar R, Sharma A, Baijal M, Vashistha A. Endoscopic neck surgery: expanding horizons. J Laparoendosc Adv Surg Tech A. 1999. 9(5):397–400.

3. Echeverri A, Flexon PB. Electrophysiologic nerve stimulation for identifying the recurrent laryngeal nerve in thyroid surgery: review of 70 consecutive thyroid surgeries. Am Surg. 1998. 64(4):328–333.
4. Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Laparosc Endosc. 1994. 4(2):92–99.
5. Rothenberg SS. Laparoscopic splenectomy using the harmonic
scalpel. J Laparoendosc Surg. 1996. 6:Suppl 1. S61–S63.
6. Amaral JF. Laparoscopic cholecystectomy in 200 consecutive patients using an ultrasonically activated scalpel. Surg Laparosc Endosc. 1995. 5(4):255–262.
7. Wolf RK, Ohtsuka T, Flege JB Jr. Early results of thoracoscopic internal mammary artery harvest using an ultrasonic scalpel. Eur J Cardiothorac Surg. 1998. 14:Suppl 1. S54–S57.

8. Robbins ML, Ferland RJ. Laparoscopic-assisted vaginal hysterectomy using the laparosonic coagulating shears. J Am Assoc Gynecol Laparosc. 1995. 2(3):339–343.

9. Siperstein AE, Berber E, Morkoyun E. The use of the harmonic scalpel vs conventional knot tying for vessel ligation in thyroid surgery. Arch Surg. 2002. 137(2):137–142.

10. Shemen L. Thyroidectomy using the harmonic scalpel: analysis of 105 consecutive cases. Otolaryngol Head Neck Surg. 2002. 127(4):284–288.

11. Ortega J, Sala C, Flor B, Lledo S. Efficacy and cost-effectiveness of the UltraCision harmonic scalpel in thyroid surgery: an analysis of 200 cases in a randomized trial. J Laparoendosc Adv Surg Tech A. 2004. 14(1):9–12.

12. Voutilainen PE, Haglund CH. Ultrasonically activated shears in thyroidectomies: a randomized trial. Ann Surg. 2000. 231(3):322–328.
13. Karvounaris DC, Antonopoulos V, Psarras K, Sakadamis A. Efficacy and safety of ultrasonically activated shears in thyroid surgery. Head Neck. 2006. 28(11):1028–1031.

14. Koutsoumanis K, Koutras AS, Drimousis PG, Stamou KM, Theodorou D, Katsaragakis S, et al. The use of a harmonic scalpel in thyroid surgery: report of a 3-year experience. Am J Surg. 2007. 193(6):693–696.

15. Miccoli P, Berti P, Dionigi G, D'Agostino J, Orlandini C, Donatini G. Randomized controlled trial of harmonic scalpel use during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2006. 132(10):1069–1073.

16. Koh YW, Park JH, Lee SW, Choi EC. The harmonic scalpel technique without supplementary ligation in total thyroidectomy with central neck dissection: a prospective randomized study. Ann Surg. 2008. 247(6):945–949.

17. Asari R, Passler C, Kaczirek K, Scheuba C, Niederle B. Hypoparathyroidism after total thyroidectomy: a prospective study. Arch Surg. 2008. 143(2):132–137.
18. Adams J, Andersen P, Everts E, Cohen J. Early postoperative calcium levels as predictors of hypocalcemia. Laryngoscope. 1998. 108(12):1829–1831.

19. Luu Q, Andersen PE, Adams J, Wax MK, Cohen JI. The predictive value of perioperative calcium levels after thyroid/parathyroid surgery. Head Neck. 2002. 24(1):63–67.

20. Bentrem DJ, Rademaker A, Angelos P. Evaluation of serum calcium levels in predicting hypoparathyroidism after total/neartotal thyroidectomy or parathyroidectomy. Am Surg. 2001. 67(3):249–251. discussion 51-2.
21. McHenry CR, Speroff T, Wentworth D, Murphy T. Risk factors for postthyroidectomy hypocalcemia. Surgery. 1994. 116(4):641–647. discussion 7-8s.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download