Abstract
In current endodontic practice, introduction of operating microscope, ultrasonic instruments, and microinstruments has induced a big change in the field of surgical retreatment. In this study, we aimed to offer key steps of endodontic microsurgery procedure compared with traditional root-end surgery, and to evaluate factors influencing success and failure based on published articles.
Endodontic microsurgery is a surgical procedure performed with the aid of a microscope, ultrasonic instruments and modern microsurgical instruments. The microscope provides magnification and illumination - essential for identifying minute details of the apical anatomy. Ultrasonic instruments facilitate the precise root-end preparation that is within the anatomical space of the canal. Modern endodontics can therefore be performed with precision and predictability, thus eliminating the disadvantages inherent in traditional periapical surgery such as large osteotomy, beveled apicoectomy, inaccurate root-end preparation and the inability to observe isthmus.
Factors influencing the outcomes of endodontic microsurgery may be diverse, but standardization of procedures can minimize its range. Among patient and tooth-related factors, periodontal status and tooth position are known to be prognostic, but there are only few articles concerning this matter. High-evidence randomized clinical trials or prospective cohort studies are needed to confirm these findings.
Figures and Tables
 | Figure 1Example of each category of the cause of endodontic failure. Note the arrows. (a) Missing canal, MB2 with an isthmus in maxillary molar; (b) Leaky canal, gap between the gutta-percha and dentin; (c)-1 & (c)-2 apical calculus, calculus deposition due to chronic sinus tract; (c)-3 Scanning electron microscopic image of apical calculus (×30K); (d) Anatomical complexity, accessory canals that has not been touched; (e) Underfilling; (f) Crack, apical crack at lingual side of root; (g) Iatrogenic problem, broken file in mesial root in mandibular molar; (h) Overfilling, over-extended gutta-percha.9
|
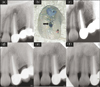 | Figure 2Typical failure case of endodontic surgery. (a) Preoperative radiograph with periradicular radiolucency showing a root-end filling apart from the filled canal; (b) Coronal surface of the resected apical fragment. Note the missing canal (arrow) that had not been touched, even after both nonsurgical and surgical retreatments. G, Gutta-percha canal filling of nonsurgical retreatment; R, Root-end filling of surgical retreatment; (c) Immediate postoperative radiograph. Super EBA was used for the root-end filling; (d), (e), and (f) Seven-year follow-up radiographs with 3 different angles showing complete healing.10
|
References
1. Friedman S. Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). Endodontic Topics. 2002. 1:54–78.

2. Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature-part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010. 36:1757–1765.

3. Creasy JE, Mines P, Sweet M. Surgical trends among endodontists: the results of a web-based survey. J Endod. 2009. 35:30–34.

4. Yang Y, Rossi FM, Putnins EE. Periodontal regeneration using engineered bone marrow mesenchymal stromal cells. Biomaterials. 2010. 31:8574–8582.

5. Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006. 32:601–623.

6. Ricucci D, Siqueira JF Jr. Fate of the tissue in lateral canals and apical ramifications in response to pathologic conditions and treatment procedures. J Endod. 2010. 36:1–15.

7. Kim E, Fallahrastegar A, Hur YY, Jung IY, Kim S, Lee SJ. Difference in root canal length between Asians and Caucasians. Int Endod J. 2005. 38:149–151.

8. Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008. 34:546–551.

9. Song M, Kim H, Lee W, Kim E. Analysis of the cause of failure in nonsurgical endodntic treatment by microscopic inspection during endodontic microsurgery. J Endod. 2011. 37:1516–1519.

10. Song M, Shin SJ, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011. 37:316–320.

11. Saunders WP, Saunders EM, Gutmann JL. Ultrasonic root-end preparation, part 2. microleakage of EBA root-end fillings. Int Endod J. 1994. 27:325–329.

12. De Bruyne MA, De Moor RJ. Influence of cracks on leakage and obturation efficiency of root-end filling materials after ultrasonic preparation: an in vitro evaluation. Quintessence Int. 2008. 39:685–692.
13. Christiansen R, Kirkevang LL, Hørsted-Bindslev P, Wenzel A. Randomized clinical trial of root-end resection followed by root-end filling with mineral trioxide aggregate or smoothing of the orthograde gutta-percha root filling-1-year follow-up. Int Endod J. 2009. 42:105–114.

14. Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008. 34:660–665.

15. Baek SH, Lee WC, Setzer FC, Kim S. Periapical bone regeneration after endodontic microsurgery with three different root-end filling materials: amalgam, Super EBA, and mineral trioxide aggregate. J Endod. 2010. 36:1323–1325.

16. Chong BS, Pitt Ford TR, Hudson MB. A prospective clinical study of mineral trioxide aggregate and IRM when used as root-end filling materials in endodontic surgery. Int Endod J. 2009. 42:414–420.

17. Song M, Jung IY, Lee SJ, Lee CY, Kim E. Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod. 2011. 37:927–933.

18. Taschieri S, Del Fabbro M, Testori T, Francetti L, Weinstein R. Endodontic surgery using 2 different magnification devices: preliminary results of a randomized controlled study. J Oral Maxillofac Surg. 2006. 64:235–242.

19. Rahbaran S, Gilthorpe MS, Harrison SD, Gulabivala K. Comparison of clinical outcome of periapical surgery in endodontic and oral surgery units of a teaching dental hospital: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001. 91:700–709.

20. Tsesis I, Rosen E, Schwartz-Arad D, Fuss Z. Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod. 2006. 32:412–416.

21. Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009. 35:930–937.

22. Tsesis I, Faivishevsky V, Kfir A, Rosen E. Outcome of surgical endodontic treatment performed by a modern technique: a meta-analysis of literature. J Endod. 2009. 35:1505–1511.

23. Wang N, Knight K, Dao T, Friedman S. Treatment outcome in endodontics-the Toronto study. phases I and II: apical surgery. J Endod. 2004. 30:751–761.

24. Zuolo ML, Ferreira MO, Gutmann JL. Prognosis in periradicular surgery: a clinical prospective study. Int Endod J. 2000. 33:91–98.

25. Lindeboom JA, Frenken JW, Kroon FH, van den. A comparative prospective randomized clinical study of MTA and IRM as root-end filling materials in single-rooted teeth in endodontic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:495–500.

26. von Arx T, Frei C, Bornstein MM. Periradicular surgery with and without endoscopy: a prospective clinical comparative study. Schweiz Monatsschr Zahnmed. 2003. 113:860–865.
27. Rud J, Andreasen JO, Jensen JE. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg. 1972. 1:195–214.

28. Molven O, Halse A, Grung B. Observer strategy and the radiographic classification of healing after endodontic surgery. Int J Oral Maxillofac Surg. 1987. 16:432–439.

29. Molven O, Halse A, Grung B. Surgical management of endodontic failures: indications and treatment results. Int Dent J. 1991. 41:33–42.
30. von Arx T, Hänni S, Jensen SS. Correlation of bone defect dimensions with healing outcome one year after apical surgery. J Endod. 2007. 33:1044–1048.

31. von Arx T, Hänni S, Jensen SS. Clinical results with two different methods of root-end preparation and filling in apical surgery: mineral trioxide aggregate and adhesive resin composite. J Endod. 2010. 36:1122–1129.

32. Rubinstein RA, Kim S. Short-term observation of the results of endodontic surgery with the use of a surgical operation microscope and super-EBA as root-end filling material. J Endod. 1999. 25:43–48.

33. Taschieri S, Del Fabbro M, Testori T, Weinstein R. Endoscopic periradicular surgery: a prospective clinical study. Br J Oral Maxillofac Surg. 2007. 45:242–244.

34. von Arx T, Jensen SS, Hänni S. Clinical and radiographic assessment of various predictors for healing outcome 1 year after periapical surgery. J Endod. 2007. 33:123–128.

35. Taschieri S, Del Fabbro M, Testori T, Weinstein R. Microscope versus endoscope in root-end management: a randomized controlled study. Int J Oral Maxillofac Surg. 2008. 37:1022–1026.

36. Kvist T, Reit C. Results of endodontic retreatment: a randomized clinical study comparing surgical and non-surgical procedures. J Endod. 1999. 25:814–817.

37. Jesslén P, Zetterqvist L, Heimdahl A. Long-term results of amalgam versus glass ionomer cement as apical sealant after apicectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995. 79:101–103.

38. Molven O, Halse A, Grung B. Incomplete healing (scar tissue) after periapical surgery-radiographic findings 8 to 12 years after treatment. J Endod. 1996. 22:264–268.

39. Friedman S. Outcome of endodontic surgery: a meta-analysis of the literature-part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2011. 37:577–578.

40. Halse A, Molven O, Grung B. Follow-up after periapical surgery: the value of the one-year control. Endod Dent Traumatol. 1991. 7:246–250.

41. Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 2002. 28:378–383.

42. Wesson CM, Gale TM. Molar apicectomy with amalgam root-end filling: results of a prospective study in two district general hospitals. Br Dent J. 2003. 195:707–714.

43. Yazdi PM, Schou S, Jensen SS, Stoltze K, Kenrad B, Sewerin I. Dentine-bonded resin composite (Retroplast) for root-end filling: a prospective clinical and radiographic study with a mean follow-up period of 8 years. Int Endod J. 2007. 40:493–503.

44. Calişkan MK. Nonsurgical retreatment of teeth with periapical lesions previously managed by either endodontic or surgical intervention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:242–248.

45. Fava LR. Calcium hydroxide in endodontic retreatment after two nonsurgical and two surgical failures: report of a case. Int Endod J. 2001. 34:72–80.

46. Schwartz-Arad D, Yarom N, Lustig JP, Kaffe I. A retrospective radiographic study of root-end surgery with amalgam and intermediate restorative material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 96:472–477.

47. Peterson J, Gutmann JL. The outcome of endodontic resurgery: a systematic review. Int Endod J. 2001. 34:169–175.

48. Gagliani MM, Gorni FG, Strohmenger L. Periapical resurgery versus periapical surgery: a 5-year longitudinal comparison. Int Endod J. 2005. 38:320–327.

49. Bahcall JK, DiFiore PM, Poulakidas TK. An endoscopic technique for endodontic surgery. J Endod. 1999. 25:132–135.

50. Lustmann J, Friedman S, Shaharabany V. Relation of pre- and intraoperative factors to prognosis of posterior apical surgery. J Endod. 1991. 17:239–241.

51. Jensen SS, Nattestad A, Egdø P, Sewerin I, Munksgaard EC, Schou S. A prospective, randomized, comparative clinical study of resin composite and glass ionomer cement for retrograde root filling. Clin Oral Investig. 2002. 6:236–243.

52. Wang Q, Cheung GS, Ng RP. Survival of surgical endodontic treatment performed in a dental teaching hospital: a cohort study. Int Endod J. 2004. 37:764–775.

53. Barone C, Dao TT, Basrani BB, Wang N, Friedman S. Treatment outcome in endodontics: the Toronto study-phases 3, 4, and 5: apical surgery. J Endod. 2010. 36:28–35.

54. von Arx T, Peñarrocha M, Jensen S. Prognostic factors in apical surgery with root-end filling: a meta-analysis. J Endod. 2010. 36:957–973.

55. Rapp EL, Brown CE Jr, Newton CW. An analysis of success and failure of apicoectomies. J Endod. 1991. 17:508–512.

56. Duncan HF, Pitt Ford TR. The potential association between smoking and endodontic disease. Int Endod J. 2006. 39:843–854.

57. Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005. 19:151–157.

58. W-Dahl A, Toksvig-Larsen S. Cigarette smoking delays bone healing: a prospective study of 200 patients operated on by the hemicallotasis technique. Acta Orthop Scand. 2004. 75:347–351.

59. Chang LD, Buncke G, Slezak S, Buncke HJ. Cigarette smoking, plastic surgery, and microsurgery. J Reconstr Microsurg. 1996. 12:467–474.

60. Testori T, Capelli M, Milani S, Weinstein RL. Success and failure in periradicular surgery: a longitudinal retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:493–498.

61. Maddalone M, Gagliani M. Periapical endodontic surgery: a 3-year follow-up study. Int Endod J. 2003. 36:193–198.

62. Taschieri S, Del Fabbro M, Testori T, Francetti L, Weinstein R. Endodontic surgery with ultrasonic retrotips: one-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:380–387.

63. Friedman S. The prognosis and expected outcome of apical surgery. Endodontic Topics. 2005. 11:219–262.

64. Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006. 39:249–281.

65. Farzaneh M, Abitbol S, Lawrence HP, Friedman S. Treatment outcome in endodontics-the Toronto study. phase II: initial treatment. J Endod. 2004. 30:302–309.

66. Hirsch JM, Ahlstroöm U, Henrikson PA, Heyden G, Peterson LE. Periapical surgery. Int J Oral Surg. 1979. 8:173–185.

67. Skoglund A, Persson G. A follow-up study of apicoectomized teeth with total loss of the buccal bone plate. Oral Surg Oral Med Oral Pathol. 1985. 59:78–81.

68. Forssell H, Tammisalo T, Forssell K. A follow-up study of apicectomized teeth. Proc Finn Dent Soc. 1988. 84:85–93.
69. Friedman S. Treatment outcome and prognosis of endodontic therapy. 2008. 2nd ed. Malden, MA: Blackwell Science.
70. Douthitt JC, Gutmann JL, Witherspoon DE. Histologic assessment of healing after the use of a bioresorbable membrane in the management of buccal bone loss concomitant with periradicular surgery. J Endod. 2001. 27:404–410.

71. Britain SK, von Arx T, Schenk RK, Buser D, Nummikoski P, Cochran DL. The use of guided tissue regeneration principles in endodontic surgery for induced chronic periodontic-endodontic lesions: a clinical, radiographic, and histologic evaluation. J Periodontol. 2005. 76:450–460.

72. Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Periapical and periodontal healing after osseous grafting and guided tissue regeneration treatment of apicomarginal defects in periradicular surgery: results after 12 months. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:474–482.

73. Marín-Botero ML, Domínguez-Mejía JS, Arismendi-Echavarría JA, Mesa-Jaramillo AL, Flórez-Moreno GA, Tobón-Arroyave SI. Healing response of apicomarginal defects to two guided tissue regeneration techniques in periradicular surgery: a double-blind, randomized-clinical trial. Int Endod J. 2006. 39:368–377.

74. Grung B, Molven O, Halse A. Periapical surgery in a Norwegian county hospital: follow-up findings of 477 teeth. J Endod. 1990. 16:411–417.

75. Dorn SO, Gartner AH. Retrograde filling materials: a retrospective success-failure study of amalgam, EBA, and IRM. J Endod. 1990. 16:391–393.

76. Pantschev A, Carlsson AP, Andersson L. Retrograde root filling with EBA cement or amalgam. A comparative clinical study. Oral Surg Oral Med Oral Pathol. 1994. 78:101–104.
77. Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993. 19:591–595.

78. Torabinejad M, Rastegar AF, Kettering JD, Pitt Ford TR. Bacterial leakage of mineral trioxide aggregate as a root-end filling material. J Endod. 1995. 21:109–112.

79. Torabinejad M, Smith PW, Kettering JD, Pitt Ford TR. Comparative investigation of marginal adaptation of mineral trioxide aggregate and other commonly used root-end filling materials. J Endod. 1995. 21:295–299.

80. Bates CF, Carnes DL, del Rio CE. Longitudinal sealing ability of mineral trioxide aggregate as a root-end filling material. J Endod. 1996. 22:575–578.

81. Pichardo MR, George SW, Bergeron BE, Jeansonne BG, Rutledge R. Apical leakage of root-end placed superEBA, MTA, and Geristore restorations in human teeth previously stored in 10% formalin. J Endod. 2006. 32:956–959.

82. Andreasen JO, Munksgaard EC, Fredebo L, Rud J. Periodontal tissue regeneration including cementogenesis adjacent to dentin-bonded retrograde composite fillings in humans. J Endod. 1993. 19:151–153.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download