Abstract
Objectives
The purpose of this retrospective study was to evaluate the success rate of intentionally replanted mandibular second molar with C-shaped canal configurations and to access the impact of preoperative periapical lesion on the success of intentional replantation procedure.
Materials and Methods
This retrospective chart review study evaluated 52 intentionally replanted mandibular second molar teeth treated at Seoul National University Dental Hospital Department of Conservative Dentistry from January 2005 to December 2007. Seventeen teeth were lost for the follow-up, and another 6 teeth did not meet inclusion criteria of C-shaped root canal configurations. Healing outcome such as success, uncertain healing, and failure after follow-up was evaluated by clinical criteria and radiographs.
For the successful root canal treatment, thorough cleaning and shaping of the root canal system is a necessary procedure. C-shaped canals are known to have a complex canal anatomy with numerous fins connecting individual canals, thus require supplementary effort to accomplish a successful root canal treatment.1,2 Generally, anthropologic differences in tooth shape is not an important issue in the root canal treatment, however, mandibular second molar is a matter of concern due to its high incidence of C-shaped root canal configurations especially in Asian populations. In this regard, recent studies3-5 reported that more than 30% of Chinese or Koreans have C-shaped mandibular second molar in their arch. This C-shaped root canal configuration is difficult to execute a successful root canal treatment because of the anatomical variations in the root canal system.6 Since the isthmus-like small canals are connecting the C-shaped fin area, perforation or overinstrumentation may occur during the canal instrumentation. The possibility of the strip perforation in this area can be much higher than in the normal tooth with a divergent root shape.5,7 Although the success rate of the root canal treatment for this type of tooth is not clarified yet, we suspect that there can be much more treatment failure than the other teeth in the arch because the transverse anastomoses connecting the C-shaped root canal configuration can harbor bacteria and infected pulp tissue and as a result, their removal can be extremely difficult.8,9
Intentional replantation is a viable treatment option when original trial of root canal treatment or even retreatment was unsuccessful and also in cases where a dental implant or a surgical treatment is not possible. Peer suggested that intentional replantation should be considered more often as a treatment modality in an effort to maintain the natural dentition.10 Therefore, intentional replantation is now considered as a reliable and predictable procedure.11 In this aspect, C-shaped mandibular second molar can be a good candidate for the intentional replantation procedure due to its conical shape of the root.9 However, there are no reports on the success rate for this type of tooth when it was intentionally replanted. Therefore, the purpose of this study is to evaluate the success rate of intentionally replanted mandibular second molar with C-shaped canal system and to access the impact of preoperative periapical lesion on the success of intentional replantation procedure by retrospective chart review.
Data for this study were obtained from the chart of the patients treated at Seoul National University Dental Hospital Department of Conservative Dentistry from January 2005 to December 2007. The study protocol was approved by the Institutional Review Board of the Seoul National University Dental Hospital. Records of all patients were screened retrospectively for intentional replantation procedures performed on mandibular second molar teeth with radiographically diagnosed to have a root with C-shaped canal system. From the charts of patients receiving intentional replantation treatment in this 3-year period, 52 replantation cases fit the preliminary inclusion criteria. Existence of preoperative periapical lesion of the tooth and the reason for the failure of the conventional endodontic treatment were recorded from the patient charts and radiographs (Table 1).
Detailed clinical procedure of the intentional replantation was as follows. The tooth was intentionally extracted with forceps under local anesthesia with 2% Lidocaine. Right after the extraction, the apical area of the tooth was carefully inspected under the operating microscope. Apical 3 mm was resected with high speed diamond bur and the granulation tissue attached to the root surface was carefully removed. Root-end cavity was prepared with #330 bur under the microscopic examination, then the cavity was filled with mineral trioxide aggregate (ProrootMTA, Dentsply, Johnson city, TN, USA). All this procedure was done within 10 minutes, and the tooth was placed back to its socket.
All the replanted teeth were evaluated 3, 6, 9 and 12 months after the treatment, and then the case was followed twice a year. The teeth were evaluated according to the clinical criteria and radiographically examined at each observation. Evaluation periods ranged from 6 months to 3 years. The radiographic and clinical data from recall visits were collected and evaluated according to the assessment criteria established by Rud et al.12 and Molven et al.13
Success was defined as complete resolution of the former periapical radiolucency during the follow-up period and the tooth was in function with no symptoms demonstrated by recorded clinical data. Uncertain healing was assumed if the teeth were present in the mouth with incomplete healing of periapical lesion or with certain degree of clinical symptoms. A case with unresolved periapical lesion or persistent clinical symptoms which needed extraction was considered as a failure.
The effect of the existence of previous periapical lesion on the success of intentional replantation procedure was analyzed by Chi-square test at a significance level of p = 0.05.
This retrospective chart review study included 52 replanted mandibular second molar teeth. However, 6 teeth did not meet inclusion criteria for C-shaped root canal configuration as Fan et al. had suggested and another 17 teeth were lost for the 1 year follow-up.14 Average follow-up period was 18.6 months.
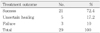
The overall success rate was 72.4% for the 29 intentionally replanted teeth (Table 2). Teeth with preoperative periapical lesions showed similar success rate when it was campared with that of replanted teeth which have no preoperative periapical lesions (Table 3). The most frequent reason for re-treatment failure which requires intentional replantation was the blockage of the root canals.
The overall success rate of intentional replantation for C-shaped mandibular second molar was 72.4%. This result was slightly lower than the success rate of intentional replantation reported in other studies.15,16 This can be explained by the fact that most studies included all tooth types in the arch. When only molar tooth of intentional replantation was considered, a success rate of 72% was reported by Raghoebar and Vissink,17 and it was comparable to that of our study.
According to Jerome, a root with C-shaped configuration is a good candidate for the intentional replantation procedure because the extraction of a tooth with this type of root can be relatively easy.9 In regard to this, Cotter and Panzarino reported one intentional replantation case which was proved to be a C-shaped mandibular second molar.18 Super EBA was used as a root-end filling material in their case and it was successfully maintained after 1 year follow-up.
In this study, MTA was used for the root end-filling. Although no confirmed protocol was set for the root-end filling material of the intentional replantation upto now, there were multiple reasons for using MTA during the intentional replantation procedure. Recent prospective clinical study19 demonstrated that periapical surgery using MTA as a root-end filling showed high success rate. A meta-analysis20 of root-end filling materials also reported that MTA was associated with the highest success when it was compared with IRM, Super-EBA or amalgam. The fact that the success rate of this study was similar to the weighted average success rate of periapical surgery21 was a good evidence for the use of MTA as a root-end filling during the intentional replantation procedure.
Pre-operative recognition of the C-shaped root canal configuration can facilitate diagnosis and treatment decision making process.22 For this purpose, radiographs can be the best practical methods to provide clues about the morphology of the root canal system. Recent study23 suggested that the presence and the configuration of C-shaped root canal system could be predicted by the periapical radiographic appearance. In this respect, Calsen demonstrated that 76.3% of the mandibular second molar with one-root shape showed a good concordance with the actual canal configuration.24 Computed tomography (CT) can be a good diagnostic aid before the intentional replantation is performed. In fact, Jin et al. demonstrated that more than 44.5% of mandibular second molars were found to have C-shaped canals by CT analysis in Korean population.5
Due to its high cost, we could not take CT for each patient in this study. From the 52 teeth which were expected to have C-shaped canal configurations by the preoperative radiographic root morphology, 6 teeth did not meet the inclusion criteria because the tooth qualified as having a C-shaped canal system had to exhibit all three following features: fused roots, a longitudinal groove on the lingual or buccal surfaces of the root, and at least one cross-section of the canal belong to the C1, C2, or C3 configuration according to the Fan's classification.14 This was because of the superimposition of the mandibular alveolar bone, even though preoperative radiographs indicated the presence of a C-shaped root.22,25,26
In this study, the main reason for the failure of the intentional replantation of C-shaped root canal seemed to be the periodontal bone breakdown (data not shown). Ricucci et al. demonstrated that periodontal involvement was the cause of failure when conventional root canal treatment of C-shaped mandibular molar cases was followed-up for 1 year.27 When intentional replantation procedure was considered, periodontal ligament could be damaged during the extraction and repositioning procedure. In fact, most of the failed cases could not obtain enough stability and in turn, periodontal bone breakdown was detected along the lingual groove. A longitudinal groove located on the lingual surface of this type of the root presumed to transmit periodontal disease from coronal part to the apical area of replanted tooth. Since this groove begins 3.8 mm below the cementoenamel junction,28 if the replanted tooth could not get enough stability, then this groove act as a highway to transport periodontal inflammation directly to the periapical tissue of the replanted tooth.
In the present study, blockage of the C-shaped root canal system was the most frequent reason for the conventional root canal treatment failure requiring additional surgical procedure such as intentional replantation. Canal bifurcation under mesial orifice or MB-D orifice was the main cause of the calcification and canal blockage.2 Complete negotiation of C-shaped canal system was impossible due to this canal bifurcation especially in the apical third. In fact, 36.4% of the canal bifurcation was present within 2 mm from the apex and the 90% of the canal below the bifurcation was blocked.2 Because of this complex anatomy, it would be extremely difficult to negotiate and debride the root canal system completely. Moreover, NiTi rotary file instrumentation is not useful in shaping fins and isthmus area of the C-shaped canal system.28,29
In conclusion, C-shaped canal exhibits multiple canal irregularities and provides a challenge in root canal treatment. If the treatment failure occurs on this type of tooth because of the bifurcation or canal blockage, then the intentional replantation can be a good alternative treatment option.
When indicated, root canal treatment failure on C-shaped mandibular second molar tooth can be predictably treated by intentional replantation regardless of the presence of periapical lesion.
Figures and Tables
References
1. Jafarzadeh H, Wu Y-N. The C-shaped root canal configuration: a review. J Endod. 2007. 33:517–523.

2. Fan B, Min Y, Lu G, Yang J, Cheung GSP, Gutmann Jl. Negotiation of C-shaped canal systems in mandibular second molars. J Endod. 2009. 35:1003–1008.

3. Yang ZP, Yang SF, Lin YC, Shay JC, Chi CY. C-shaped root canals in mandibular second molars in a Chinese population. Endod Dent Traumatol. 1988. 4:160–163.

4. Seo MS, Park DS. C-shaped root canals of mandibular second molars in a Korean population: clinical observation and in vitro analysis. Int Endod J. 2004. 37:139–144.

5. Jin GC, Lee SJ, Roh BD. Anatomical study of C-shaped canals in mandibular second molars by analysis of computed tomography. J Endod. 2006. 32:10–13.

6. Melton DC, Krell KV, Fuller MW. Anatomical and histological features of C-shaped canals in mandibular second molars. J Endod. 1991. 17:384–388.

7. Gao Y, Fan B, Cheung GSP, Gutmann Jl, Fan M. C-shaped canal system in mandibular second molars Part IV-3D morphological analysis and transverse measurement. J Endod. 2006. 32:1062–1065.

8. Ingle J, Bakland L. Endodontics. 2002. 5th ed. Philadelphia: Lea & Febiger;558.
9. Jerome CE. C-shaped root canal systems: diagnosis, treatment, and restoration. Gen Dent. 1994. 42:424–427.
10. Peer M. Intentional replantation - a "last resort" treatment or a conventional treatment procedure: Nine case reports. Dent Traumatol. 2004. 20:48–55.

11. Wolcott J, Rossman LE. Intentional replantation of endodontically treated teeth: an update. Compend Contin Educ Dent. 2003. 24:68–74.
12. Rud J, Andreasen JO, Jensen JE. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg. 1972. 1:195–214.

13. Molven O, Halse A, Grung B. Observer strategy and the radiographic classification of healing after endodontic surgery. Int J Oral Maxillofac Surg. 1987. 16:432–439.

14. Fan B, Cheung GSP, Fan M, Gutmann JL, Bian Z. C-shaped canal system in mandibular second molars: Part I-anatomical features. J Endod. 2004. 30:899–903.

15. Bender IB, Rossman LE. Intentional replantation of endodontically treated teeth. Oral Surg Oral Med Oral Pathol. 1993. 76:623–630.

16. Kingsbury BC Jr, Wiesenbaugh JM Jr. Intentional replantation of mandibular premolars and molars. J Am Dent Assoc. 1971. 83:1053–1057.

17. Raghoebar GM, Vissink A. Results of intentional replantation of molars. J Oral Maxillofac Surg. 1999. 57:240–244.

19. Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008. 34:660–665.

20. Fernandez-Yanez Sanchez A, Leco-Berrocal MI, Martinez-Gonzalez JM. Metaanalysis of filler materials in periapical surgery. Med Oral Patol Oral Cir Bucal. 2008. 13:E180–E185.
21. Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009. 35:930–937.

22. Fan W, Fan B, Gutmann JL, Cheung GSP. Identification of C-shaped canal in mandibular second molars: Part I - radiographic and anatomical features revealed by intraradicular contrast medium. J Endod. 2007. 33:806–810.

23. Fan B, Cheung GSP, Fan M, Gutmann JL, Fan W. C-shaped canal system in mandibular second molars: Part II - radiographic features. J Endod. 2004. 30:904–908.

24. Carlsen O. Root complex and root canal system: a correlation analysis using one-rooted mandibular second molars. Scand J Dent Res. 1990. 98:273–285.

25. Fan W, Fan B, Gutmann JL, fan M. Identification of C-shaped canal in mandibular second molars - Part III: Anatomical features revealed by digital subtraction radiography. J Endod. 2008. 34:1187–1190.

26. Fan B, Gao Y, Fan W, Gutmann JL. Identification of C-shaped canal in mandibular second molars - Part II: the effect of bone image superimposition and intraradicular contrast medium on radiograph interpretation. J Endod. 2008. 34:160–165.

27. Ricucci D, Pascon EA, Langeland K. Long-term follow-up on C-shaped mandibular molars. J Endod. 1996. 22:185–187.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download