Abstract
Objectives
This study was aimed to examine the patients' perception and satisfaction with the results of endodontic microsurgery which was apicoectomy with retrofilling.
Materials and Methods
A questionnaire was given to 109 patients, who were recalled after a minimum of 3 months upon endodontic microsurgery in the Department of Conservative Dentistry, Yonsei University. A contingency table and correlation analysis were used to determine if there were any correlations between age/gender and the patients' responses (p = 0.05).
Results
Approximately 60% of respondents answered they had never heard of surgical endodontic procedures. 63.3% of respondents chose the surgical option because they wanted to keep their natural teeth. If the patient required the same procedure on another tooth later, 100 out of 109 respondents answered they would choose microsurgery instead of extraction. Most patients (82.57%) appeared to be satisfied with the surgical procedure.
The success rate of current endodontic microsurgery has been reported to range between 70% and 95%.1-4 Recently, at our institution, Kim et al. reported a 91.5% overall success rate in 188 apicoectomy with retrofilling cases.5 They considered the cases successful when there was the absence of clinical signs and/or symptoms and radiographic evidence of complete or incomplete healing. Although apicoectomy is an established procedure, it may not be familiar to the general population compared to non-surgical root canal therapy or dental implants. In order to make this endodontic surgical procedure available to future patients and dentists unfamiliar with the procedure, it would be valuable to assess apicoectomy not only from a scientific point of view, but also from the patients who underwent the procedure.6-8
This study investigated the patient's perception and satisfaction for apicoectomy with retrofilling by survey.
A questionnaire was given to patients, who were recalled for recall after endodontic microsurgery in the Department of Conservative Dentistry, Yonsei University Dental Hospital and GangNam Severance Dental Hospital, Yonsei University, Seoul, Korea between July 2006 and June 2008. The patients who returned for at least 3-month routine check-up after surgery were enrolled in this study. The aim of the survey was explained to the patients who wished to participate in this study. The institutional Review Board of GangNam Severance Hospital, Yonsei University approved both the protocol and the informed consent. The written informed consent was obtained from each patient (No 3-2008-0082).
Those who visited the clinic within 3 months after the surgical procedure and/or could not express their own opinions on the medical reasons were excluded. Those who underwent surgical intentional replantation and autotransplantation were also excluded.
The surgical procedures were performed according to the methods reported by Kim et al.5 All the patients were treated by faculties who had been specially trained for endodontics. Surgical procedures were carried out using a dental operating microscope (OPMI PICO, Carl Zeiss, Göttingen, Germany) except for local anesthesia, incision, flap elevation and suture.
The questionnaire is shown in Table 1.
One hundred and nine patients (41 male patients and 68 female) participated in the survey. The average age of the patients' age was 41.4 years (Table 2).
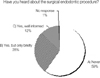
Approximately 60% of respondents answered that they had never heard of surgical endodontics before. Only 12% of patients said that they had sufficient knowledge (Figure 1).
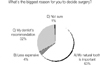
Most patients (63.3%) decided on the surgical procedure instead of extraction because that they wanted to keep their natural tooth. There were a relatively low percentage of respondents (4%) who were treated with surgery due to economical reasons (Figure 2).
If the patient required the same procedure on another tooth in the future, 100 out of 109 respondents answered that they would prefer microsurgery instead of extraction. Similarly, if a friend or family member required endodontic surgery, 90 patients said they would recommend the procedure to them (Figure 3).
Most patients (82.6%) appeared to be satisfied with the surgical procedure. Although the prognosis of the procedure was not always positive in the short term, 83.% of patients responded they would have no regrets because they felt that they had done any attempt to save their natural dentition (Figure 4).
Although apicoectomy is already a well-established procedure, it may not have been familiar to the general population compared to dental implants. This survey clearly showed that most patients who underwent the procedure were unaware of the procedure before. From the patients' point of view, it is more important to save their natural teeth rather than save money. Another interesting finding is that most of the patients responded that they would have no regrets if the treated tooth required extraction because they felt that they had made any effort to save their natural tooth.
Even though the survey did not included postoperative symptoms, patients' high satisfaction indirectly indicates that post operative sequelae of apical surgery are not a major issue.
The small sample size might be a limitation of this study. In addition, those patients who did not return for a routine check-up may have responded differently. Harrison et al.mentioned that very satisfied and very dissatisfied respondents might have a tendency to participate actively in the survey.8 However, the results of the survey might be meaningful to endodontists because it canvassed the patients' opinions of apical surgery.
This study highlights the need to provide sufficient information on endodontic surgical procedures through as many routes as possible.
Figures and Tables
References
1. Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 2002. 28:378–383.

2. Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008. 34:660–665.

3. Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009. 35:930–937.

4. Zuolo ML, Ferreira MO, Gutmann JL. Prognosis in periradicular surgery: a clinical prospective study. Int Endod J. 2000. 33:91–98.

5. Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008. 34:546–551.

6. Hassel AJ, Wegener I, Rolko C, Nitschke I. Self-rating of satisfaction with dental appearance in an elderly German population. Int Dent J. 2008. 58:98–102.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download