Abstract
Objectives
This study aimed to assess prospectively the clinical outcome of nonsurgical endodontic treatment and identify patient- and tooth-related factors, rather than treatment-related factors, that were the best predictors of this outcome.
Materials and Methods
The inception cohort comprised 441 teeth (320 patients) and 175 teeth (123 patients) were followed up for 1-2 years. Age, gender, presence of medical disease, number of canals, previous endodontic treatment, presence of sensitivity and pain, pulp vitality, swelling or sinus tract of pulpal origin on the gingiva, periapical radiolucency and tendency of unilateral bite on the affected tooth were recorded at treatment start.
Results
The outcome was classified on the basis of periapical radiolucency as healed or non healed. The overall healed rate in these cases, including nonsurgical retreatment, was 81.1%. Four tooth-related factors had a negative impact in the bivariate analysis: previous endodontic treatment, necrotic pulp, preoperative gingival swelling or sinus tract of pulpal origin, and preoperative periapical radiolucency. Stepwise logistic regression analysis including patient-, tooth-related factors and level of the root canal filling as a treatment-related factor showed that preoperative gingival lesion (odds ratio [OR]: 4.4; p = 0.005), preoperative periapical radiolucency (OR: 3.6; p = 0.011), and ≤ 1-2 mm under root filling length (OR: 9.6; p = 0.012) were significant predictors of failure.
The outcome of endodontic treatment and its related factors have been assessed in many studies.1,2 The success rate and associated factors of the tooth being treated are important to estimate the prognosis and provide sound evidence for treatment decisions. The concept of evidence-based treatment has gained increasing recognition in the last decade. The patient should be informed regarding the possible outcome of nonsurgical root canal therapy and the available evidence on the procedure during treatment planning.
The success of nonsurgical endodontic treatment is dependent on preoperative, intraoperative, and postoperative factors,3,4 including preoperative absence of periapical radiolucency, root filling without voids, root filling within 2 mm of the radiographic apex, and satisfactory coronal restoration. Of these factors, the pulpal and periapical diagnoses are considered the most important. Further, the preoperative presence versus absence of periapical radiolucency is a major indicator of postoperative healing or failure.1-10
To assess the treatment outcome and elucidate the effect of specific factors on the outcome, randomized controlled trials are graded higher scores for the strength of level of evidence.11 Treatment techniques and instruments have been effectively evaluated in randomized controlled studies.12-16 However, the special prospective cohort study models have been proposed to assess the outcome of endodontic treatment and elucidate the effect of various preoperative factors on the outcome in several studies.7-10 A conspicuous aspect of these studies was the identified inception cohort, standardized treatment procedures, and data recording at the start of the study.
The objective of the present study was to assess prospectively the 1- to 2- year clinical outcome of nonsurgical endodontic treatment by one endodontist and identify patient- and tooth-related factors rather than treatment-related factors as the best predictors of this outcome.
The study population comprised patients who received dental treatment between March 2006 and December 2007 at the Department of Dentistry in Kangdong Sacred Heart Hospital. The inception cohort comprised 441 teeth (320 patients), which were treated nonsurgically by one endodontic specialist. Data on diagnostic radiographs and clinical signs and symptoms were collected at the start of treatment. If the patient was referred by another operator after access cavity preparation, the signs and symptoms were confirmed from the clinical records and the history.
Age, gender, and the presence of medical disease were recorded as patient-related factors. The number of canals, initial treatment versus retreatment, presence of sensitivity and pain, pulp vitality, gingival swelling or presence of sinus tract of pulpal origin, preoperative apical radiolucency, and tendency for unilateral bite on the affected tooth were classified as tooth-related factors. The diagnostic radiographs (periapical radiographs or orthopantomogram) were interpreted by an oral radiologist, and the periapical radiographs for working length determination were interpreted by the endodontist. A distinct radiolucent area with loss of lamina dura (periapical index [PAI]17 score, 3-5) was considered to indicate periapical radiolucency, and a normal periapical condition or widened periodontal ligament space (PAI score, 1 or 2) suggested the absence of periapical disease.
After conventional straight-line access cavity preparation, instrumentation was completed in a crown-down manner with NiTi rotary instruments (ProFile .06/.04; Maillefer Instruments Holding Srl, Dentsply International, Ballaigues, Switzerland) or a combination of NiTi rotary and stainless steel hand filing (Mani, Inc., Tochigi, Japan). During root canal instrumentation, 5.25% NaOCl was used only as an irrigant. The canals were filled by lateral condensation with gutta-percha and sealapex (SybronEndo, Glendora, CA, USA). No intracanal medicament was used between the treatment sessions, because it could not be applied during single-visit treatment and no root canal microbial culture was obtained.
After the endodontic treatment, the teeth were restored with a crown (62.6%) or definitively sealed with amalgam, glass ionomer cement, or composite resin (37.4%). The level of the root canal filling was measured as a treatment-related factor and scored as 0 (flush to the radiographic apex), 1 (< 1 mm underfilled), 2 (≤ 1-2 mm underfilled), or 3 (overfilled) according to the periapical radiograph taken after obturation. Periapical radiographic exposures were made with YOSHIDA dental X-ray unit (Model REX 601, Toshiba, Japan) with CDR 2000 sensor (Shick Technologies, Long island, NY, USA). The digital radiograph images were processed and saved by using the Computerized dental X-ray (CDX) view (Pointnix co. Seoul, Korea). Periapical radiographs were taken using bisecting technique and saved in a picture archiving communication system (PACS).
In total, 123 patients (175 teeth) were recalled at prescheduled periods or required other dental treatment after 12-24 months. The history and clinical examinations were reviewed by the endodontist, and the follow-up periapical radiographs were assessed jointly by an oral radiologist and the endodontist until a consensus was reached; the main outcome measure was the absence (PAI score 1 or 2) or presence (PAI score, 3-5) of periapical radiolucency. On the basis of this measure, the outcome was dichotomized as healed or non-healed.
Outcome analysis was performed by using the tooth as a unit of analysis. Univariate analysis involved calculation of the frequency of variables. Bivariate analyses (chi-square test or Fisher's exact test) were used to examine the associations between the treatment outcome and each variable, and multivariate analysis with logistic regression analysis was used to evaluate the combined associations of the factors. The dependent variable in the bivariate and multivariate analyses was the dichotomous outcome (i.e., healed versus non-healed). All statistical tests were two-tailed, and significance was set at the 5% probability level.
Table 1 is a summary of the characteristics of the treated and follow-up teeth. The patient age ranged from 10 years to 85 years, and the number of roots ranged from 1 to 4. These factors were analyzed as continuous rather than categorical variables. The level of root canal filling was categorized into 4 groups, whereas the other factors were categorized as dichotomous variables.
The overall success rate of the follow-up cases was 81.1%. The success rate was 92% for teeth with vital pulps, 64.1% for those with preoperative periapical radiolucency, and 51.6% for those with preoperative gingival swelling or sinus tract of pulpal origin. Of the 175 teeth analyzed, 142 were classified as healed and 33 as non-healed with periapical radiolucency.
Among the 33 teeth classified as non-healed, the radiolucency decreased in size or remained the same without clinical symptoms in 15 teeth, and emerged or increased in 18 teeth. Therefore, 157 teeth (89.7%) were considered as functional. Of the 18 symptomatic teeth, 4 received nonsurgical endodontic retreatment, 10 underwent endodontic surgical procedures, and 4 were extracted. The reasons for extraction were failure of apical healing with root fracture (1 tooth), disease of the furcation area (1 tooth), and combined periodontal problem (2 teeth).
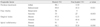
The chi-square test showed the statistically significant associations of four tooth-related categorical factors, which were endodontic treatment history, necrotic pulp status, preoperative gingival swelling or sinus tract of pulpal origin, and periapical radiolucency, with the healed rate (Table 2). Bivariate analyses showed that gender (p = 0.63), presence of medical disease (p = 1.00), sensitivity and pain (p = 0.19), unilateral bite (p = 0.37), and length of root filling (p = 0.29) were not statistically significant.
Stepwise logistic regression analysis for the relationship of the patient- and tooth-related factors to treatment failure showed that the presence of a preoperative gingival lesion and periapical radiolucency were significantly associated with failure (Table 3). A stepwise logistic regression analysis for the potential of all the factors including canal filling level to prevent healing showed that preoperative gingival lesion (p = 0.005), preoperative periapical radiolucency (p = 0.011), and ≤ 1-2 mm underfilled root canal obturation (p = 0.012), were significantly associated with treatment failure, with odds ratios (ORs) of 4.4, 3.6, and 9.6, respectively (Table 4).
In this study, the overall healed rate was calculated as 81.1% on the basis of the radiographic findings, and 89.7% of the analyzed teeth were functional without clinical symptoms. Among the preoperative factors, preoperative apical radiolucency and preoperative gingival swelling or sinus tract of pulpal origin were significantly associated with failure of nonsurgical endodontic treatment.
On the basis of the radiographic findings, the success rate was 92% for the teeth with vital pulps, but 69.8% for those with previous endodontic treatment. These rates evaluated by using periapical radiographs, might be overestimated because the validity of using PAI scores for all tooth positions except maxillary incisor region was reported to be questionable.18 It was also suggested that recall rates should be considered in the outcomes of longitudinal studies.19 The success rate in the present study is questionable because the recall rate was 39.7%. However, the results of the relative impact of the prognostic factors in this study are not meaningless because the frequencies of the predisposing factors in the analyzed sample were similar to those in the total population (Table 1).
In the present study, the endodontist confirmed that the successful cases were clinically asymptomatic and functional without preoperative symptoms when they were followed up. The symptomatic unhealed cases underwent nonsurgical endodontic retreatment, apical surgery, or extraction. The investigated prognostic factors were clinical signs and symptoms, which were independent from the radiographic diagnosis except for preoperative apical radiolucency. Bender and Seltzer20,21 have indicated that clinical symptoms such as pain, swelling, and presence of a sinus tract can occur without radiographic evidence of bone destruction. The clinically detectable factors indicating the pulpal and periapical state are more important because a patient's questions regarding the success rate and prognosis of root canal therapy should be answered during treatment planning.
More than 90% of the teeth without a preoperative periapical lesion were clinically healthy, whereas only 64.1% with a preoperative periapical radiolucency healed in this study. These results are in agreement with earlier findings that teeth with apical periodontitis have a significantly lower success rate than those without such lesions.5-10 Stepwise logistic regression analysis revealed that preoperative apical radiolucency was important for predicting treatment failure, with an OR of 3.6 (p = 0.011): in other words, teeth with diseased periapical status have a 3.6 times greater risk of failure than those with a normal periapex. This OR is similar to the values reported in the Toronto studies,8,9 but lower than that found in other studies.7,10,21
In addition to apical radiolucency, preoperative gingival swelling and sinus tract of pulpal origin had a significant effect on the nonsurgical endodontic treatment; the least favorable healed rate (51.6%) was associated with this factor. This result is similar to the success rate for teeth with sinus tracts reported by Chugal et al. (40.7%, p < 0.001).7 In that study, the preoperative presence of a sinus tract was classified into a group that included necrotic pulp and chronic apical periodontitis. In the present study, in addition to the presence of a sinus tract, a gingival lesion, including swelling of the gingiva and face, was analyzed as an independent variable, because these signs and symptoms were not associated with other clinical symptoms in all cases.
Every tooth, in this study, was obturated when the previous symptoms except periapical radiolucency had been disappeared. The cases were excluded if they could not obturated because of the persistent symptoms. However, 10 unhealed teeth were symptomatic at recall and required periapical surgery. Of these, 7 had a preoperative gingival problem. This result equates to 22.6% of the teeth with a preoperative gingival lesion requiring apical endodontic surgery, whereas 9.4% (6 teeth) with preoperative periapical periodontitis underwent surgical treatment. These finding suggest that the presence of a gingival problem of pulpal origin can be as decisive for predicting treatment failure as the presence of preoperative apical radiolucency. Therefore, additional surgical endodontic treatment should be considered in patients with preoperative gingival swelling or sinus tract of pulpal origin during initial treatment planning.
The treatment factors considered in the majority of the previous studies on nonsurgical root canal treatment were associated with canal obturation, regarded as the most important factor in nonsurgical endodontic treatment.7-10,22-24 Multivariate analysis in the present study showed that the level of the root canal filling was also indispensable to the treatment outcome and that the canal should be filled within 1 mm of the radiographic apex. However, a significant association between the treatment outcome and this factor was not obtained by the chi-square test, even if the level of canal filling was divided into adequate (< 1 mm underfilled) or inadequate (≤ 1-2 mm underfilled or overfilled). In contrast, the impact of inadequate canal obturation on treatment failure was a prominent and significant factor in the logistic regression analysis, despite the greater 95% confidence interval (Table 4). These results suggest that the presence of various treatment related-factors alters the impact of preoperative variables on treatment outcome in stepwise logistic regression analysis. The comparison of relative impact could be obtained in the stepwise logistic regression analysis by elimination of the least significant independent variables.
Some reviewers of studies concerning the outcome of root canal treatment concluded that it is desirable to standardize aspects of the study design, data recording, and presentation format of outcome data.2,3 However, it is difficult to standardize the study design to evaluate all prognostic factors because statistical analysis of the affecting factors is influenced by the number of these factors included. In this study, the result of the logistic regression analysis without the treatment-related factor was slightly different from that including the factor (i.e., level of root canal filling).
A prospective cohort study design was chosen because clinical and radiographic examinations of the preoperative factors are the most common procedures used to predict the outcome of root canal therapy prior to treatment. However, the level of evidence obtained with the data is limited owing to the lack of randomization and the predetermined treatment protocol. To ascertain the validity and reliability of these findings, further studies are needed by using a greater number of teeth with preoperative gingival swelling and sinus tract, presence of sensitivity and pain, tendency of unilateral occlusion, or other preoperative symptoms. Randomized clinical trials should also be performed to evaluate treatment-related factors such as canal enlargement and obturation techniques, intracanal medicaments, and instruments for effective disinfection.
The overall healed rate of nonsurgical endodontic treatment by one endodontist was 81.1% on the basis of the radiographic findings, with 89.7% of the teeth being functional. Among the clinically detectable preoperative factors, preoperative apical radiolucency and preoperative gingival swelling or sinus tract of pulpal origin were significantly associated with the failure of nonsurgical endodontic treatment. Therefore, randomized clinical trials with the predetermined protocol regarding these symptoms are needed to improve success rates of root canal treatment.
Figures and Tables
Table 2
Significant associations of the four tooth-related factors with the healed rate calculated by the chi-square test
References
1. Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, et al. Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97:95–99.

2. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature-Part 1. Effects of study characteristics on probability of success. Int Endod J. 2007. 40:921–939.

3. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature-Part 2. Influence of clinical factors. Int Endod J. 2008. 41:6–31.
4. Ng Y-L, Mann V, Gulabivala K. The probability of and factors influencing tooth survival following non-surgical root canal treatment-a prospective study. Int Endod J. 2010. 43:171–189.
5. Sjogren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990. 16:498–504.

6. Friedman S, Löst C, Zarrabian M, Trope M. Evaluation of success and failure after endodontic therapy using a glass ionomer cement sealer. J Endod. 1995. 21:384–390.

7. Chugal NM, Clive JM, Spångberg LSW. A prognostic model for assessment of the outcome of endodontic treatment: effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001. 91:342–352.

8. Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto study. Phase I: initial treatment. J Endod. 2003. 29:787–793.

9. Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study. Phase III: initial treatment. J Endod. 2006. 32:299–306.

10. Marending M, Peters OA, Zehnder M. Factors affecting the outcome of orthograde root canal therapy in a general dentistry hospital practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 99:119–124.

11. Torabinejad M, Kutsenko D, Machnick TK, Ismail A, Newton CW. Levels of evidence for the outcome of nonsurgical endodontic treatment. J Endod. 2005. 31:637–646.

12. Orstavik D, Hörsted-Bindslev P. A comparison of endodontic treatment results at two dental schools. Int Endod J. 1993. 26:348–354.

13. Trope M, Delano EO, Ørstavik D. Endodontic treatment of teeth with apical periodontitis: single vs. multivisit treatment. J Endod. 1999. 25:345–350.

14. Weiger R, Rosendahl R, Löst C. Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. Int Endod J. 2000. 33:219–226.

15. Pettiette MT, Delano EO, Trope M. Evaluation of success rate of endodontic treatment performed by students with stainless-steel K-files and nickel-titanium hand files. J Endod. 2001. 27:124–127.

16. Kim HC, Park JK, Hur B. Relative efficacy of three Ni-Ti file systems used by undergraduates. J Korean Acad Conserv Dent. 2005. 30(1):38–48.

17. Orstavik E, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986. 2:20–34.

18. Huumonen S, Ørstavik D. Radioligical aspects of apical periodontitis. Endod Topics. 2002. 1:3–25.
19. Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J. 2009. 42:656–666.

20. Bender IB, Seltzer S. The oral fistula: its diagnosis and treatment. Oral Surg Oral Med Oral Pathol. 1961. 14:1367–1376.

21. Seltzer S, Bender IB, Nazimov H. Differential diagnosis of pulp conditions. Oral Surg Oral Med Oral Pathol. 1965. 19:383–391.

22. Imura N, Pinheiro ET, Gomes BP, Zaia AA, Ferraz CC, Souza-Filho FJ. The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod. 2007. 33:1278–1282.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download