Abstract
Objectives
The purpose of the present in vitro study was to evaluate the biocompatibility of mineral trioxide aggregate (MTA) mixed with glass ionomer cement (GIC), and to compare it with that of MTA, GIC, IRM and SuperEBA.
Materials and Methods
Experimental groups were divided into 3 groups such as 1 : 1, 2 : 1, and 1 : 2 groups depending on the mixing ratios of MTA powder and GIC powder. Instead of distilled water, GIC liquid was mixed with the powder. This study was carried out using MG-63 cells derived from human osteosarcoma. They were incubated for 1 day on the surfaces of disc samples and examined by scanning electron microscopy. To evaluate the cytotoxicity of test materials quantitatively, XTT assay was used. The cells were exposed to the extracts and incubated. Cell viability was recorded by measuring the optical density of each test well in reference to controls.
Results
The SEM revealed that elongated, dense, and almost confluent cells were observed in the cultures of MTA mixed with GIC, MTA and GIC. On the contrary, cells on the surface of IRM or SuperEBA were round in shape. In XTT assay, cell viability of MTA mixed with GIC group was similar to that of MTA or GIC at all time points. IRM and SuperEBA showed significantly lower cell viability than other groups at all time points (p < 0.05).
Mineral trioxide aggregate (MTA) has been proposed for use as root-end filling material, root or furcal perforation repair material, apexification and obturation of the root canal system. Additionally, MTA is an effective pulp capping material able to stimulate reparative dentin formation by the defensive mechanism of early pulpal wound healing.1
The initial pH of MTA is 10.2, with an increase to 12.5, 3 hours after mixing.2 MTA offers a biologically active substrate for bone cells and stimulates interlukin production because of its alkaline pH and calcium ion release.3
The biocompatibility of MTA has been assessed in many studies.3-14 Calcium hydroxide which is biocompatible with tissue, is the main compound released by MTA in water.3 The results of an in vitro study showed that MTA was less toxic than amalgam, SuperEBA and IRM.4 Kwon et al. reported that MTA inhibits the stimulatory function of growth factors on granulation tissue formation and promotes the healing process modulated by bone-remodeling cells.5 MTA extracts were reported to be more biocompatible with human osteogenic sarcoma cells than calcium hydroxide based material and eugenol based material. 6 In an in vitro study assessing cell viability on the surface of MTA, MTA showed low cytotoxicity similar to control group.7 Koh et al. reported that MTA offers a biologically active substrate for bone cells and stimulates interleukin production.8 In animal studies, MTA proved to be more biocompatible to pulp tissue than calcium hydroxide and calcium sulfate as pulp capping material.9 MTA was also the only material studied that allowed cementum overgrowth.10,11 In vitro studies of human osteoblasts showed that MTA stimulated cytokine release and interleukin production.12,13 These studies suggest that MTA is not just an inert material but may actively promote hard tissue formation.14
Glass ionomer cement (GIC) has been used extensively in dentistry in spite of its technique-sensitivity. One of the advantages of GIC is its good biocompatibility and low cytotoxicity which have been well described in the previous studies.15,16
Recently, some studies that used MTA with another vehicle,17,18 or with various additives19 have been reported. The purpose of those studies was to facilitate the use of MTA, but there was still the risk of impairing the biocompatibility of MTA. Therefore, it would be of interest to investigate the feasibility of using MTA mixed with GIC which is well known biocompatible material.
The main drawbacks of MTA are the setting time, its handling characteristics, and its high cost. The setting time of MTA is about 3 hours2 and the mixture of MTA and distilled water is difficult to deliver and condense.14 As a preliminary study, the setting time of MTA mixed with GIC was assessed. The setting time proved to be significantly shorter than MTA. In addition to it, the handling characteristics were improved as it became more sticky and was easier to compact. Moreover, GIC is much cheaper than MTA.
The purpose of the present study was to evaluate the biocompatibility of MTA mixed with GIC and to compare it with that of MTA, GIC, IRM, and SuperEBA using SEM observation and cell viability assay. MTA mixed with GIC was devised with the intention of improving the handling characteristics of MTA and the ultimate goal of this study was to evaluate the clinical feasibility of MTA mixed with GIC.
Four materials were used: white mineral trioxide aggregate (MTA: ProRoot MTA, Dentsply Tulsa Dental, Tulsa, OK, USA), glass ionomer cement (GIC: Fuji II, GC Corporation, Tokyo, Japan), and two types of reinforced zinc oxide-eugenol cements including IRM (Dentsply International Inc., York, PA, USA) and SuperEBA fast set (Bosworth Co., Skokie, IL, USA).
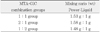
Experimental groups were divided into the following 3 categories depending on the MTA and GIC powder mixture volume ratios: 1) 1 : 1 group (MTA powder : GIC powder = 1 : 1) 2) 2 : 1 group (MTA powder : GIC powder = 2 : 1) 3) 1 : 2 group (MTA powder : IC powder = 1 : 2). The experimental powder was mixed with GIC liquid instead of distilled water. Powder-to-liquid mixing ratios for MTA-GIC combination groups are described in Table 1. Powder-to-liquid ratio for each MTA-GIC combination group was the same as each other in volume because the same level scoop and liquid dispensing method were used. However, it varied in weight because the same volume of MTA weighs more than that of GIC powder.
All the other groups except the MTA-GIC combination groups were mixed according to the manufacturers' instructions.
The selected cell line, MG-63 cells derived from human osteosarcoma, were maintained in Dulbeco's Modified Eagle's Medium (DMEM High Glucose 1X, GIBCO, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS, JR Scientific, Inc., Woodland, CA, USA) and 1% antibiotics (Pen Strep, GIBCO, Grand Island, NY, USA) in a humidified 37℃ CO2 incubator.
The samples were fabricated in a sterile cylindrical polyethylene tube, and yielded the discs of the size of 5 mm in diameter and 3 mm in height. The materials were mixed and placed into the mold. Excess flash was removed. After the samples had set, they were sterilized with ethylene oxide gas.
Six samples for each test material were fabricated and placed in the bottom of 96 well culture plates with one disc per well. After the samples were immersed in DMEM for 72 hours, the media was discarded. MG-63 cells were seeded into the wells at density of 1 × 106 cells per well in 300 µL medium. The plates were then incubated for 1 day. After incubation, the discs of materials along with the cells grown on their surface were washed three times with tris-buffered saline (TBS) for 10 minutes each, fixed with 2.5% glutaraldehyde in 0.1 M TBS buffer (pH 7.4) for 2 hours and rinsed with TBS solution. The samples were dehydrated in ascending grades of ethanol (40% for 10 minutes, 50% for 10 minutes, 60% for 10 minutes, 70% for 10 minutes, 80% for 10 minutes, 90% for 10 minutes, and three times in 100% for 10 minutes each), air-dried,20,21 and sputter-coated with 15 nm gold palladium. Samples were then observed using a scanning electron microscope (Hitachi S4700, Hitachi High-Tech Corp., Tokyo, Japan) at various magnifications.
Cytotocixity testing was done through XTT assay of MG-63 cells exposed to the extract media of test materials. The extracts were prepared as follows. Ten sample discs per material were fabricated and placed into each well of a 24 well culture plate. Into each well, 0.5 ml serum-free DMEM with 1% antibiotics was added.
After 1 day, the extracts were collected and diluted with DMEM supplemented with 10% fetal bovine serum and 1% antibiotics to make the extracts contain 2% fetal bovine serum. The extracts were filtered for sterilization.
The cells were placed in 24 well plates at a density of 1.0 × 105 cells per well and allowed to attach for 24 hours.22 After overnight attachment, 500 µL of the material extracts were added into each well. Negative control was composed of 500 µL of DMEM supplemented with 2% fetal bovine serum and 1% antibiotics. MG-63 cells and 500 µL of DMEM supplemented with 2% fetal bovine serum and 1% antibiotics were used as the positive control. The cells exposed to the extracts were incubated for 1, 4, and 7 days and XTT assay was performed at each time point.
Cell viability was determined by the ability of the cells to cleave the tetrazolium salt (2,3-bis [2-methoxy-4-nitro-5-[(sulfenylamino) carbonyl]-2H-tetrazolium-hydroxide]) (XTT) to a formazan dye. The cleavage of the tetrazolium salt into the water-soluble formazan was performed by succinate-tetra-zolium reductase system which belongs to the respiratory chain of the mitochondria and active only in the viable cells. The amount of the formazan dye was directly proportional to the number of living cells. Therefore XTT assay is one of the colormetric assay for analyzing the number of viable cells. The formazan dye produced by viable cells can be quantified by multi-well spectrophotometer by measuring the absorbance of the dye solution at wavelength between 420 and 480 nm.
XTT reagent (Ez CyTox, Itsbio, Inc., Seoul, Korea) was added to the well, 40 µL per well, and the wells were incubated for 30 minutes. Two hundred µL of media were transferred to 96 well plate and read in a multiwell spectrophotometer (ELX 800UV, BioTek Instruments, Inc., Winooski, VT, USA) at primary wave length of 450 nm and reference wave length of 630 nm.
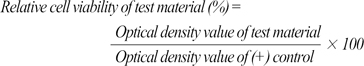
Relative cell viability of test material was calculated as follows.
Figure 1 shows the surfaces of the test materials and the morphology of the cells incubated on them for 1 day.
Elongated, dense, and almost confluent cells were observed in the cultures of the experimental groups (Figures 1a-1c), MTA (Figure 1d) and GIC (Figure 1e). Anchoring processes extended from cells to the cement surface and to other cells. On the contrary, cells on the surface of IRM or SuperEBA were round in shape and the numbers and the density of the cells were much smaller than those of other groups (Figures 1f and 1g).
Mean values of optical density meaning cell viability are presented in Table 2. In the positive control, cells were cultivated without adding extracts. Relative cell viability of MG-63 cells exposed to the extracts is presented in Figure 2.
Irrespective of the mixture ratios and the cultivation time, cell viability of MTA mixed with GIC was similar to that of MTA or GIC at all time points (Table 2). On the contrary, IRM and SuperEBA showed significantly lower cell viability than other groups at all time points (p< 0.05, Table 2).
In the relative cell viability depending on the cultivation time, there was no definite tendency about the cultivation time in each test material (Figure 2b). However, there were significant difference between cultivation for 1 day and for 4 days in 1 : 1 group, IRM, and SuperEBA (p< 0.01, Figure 2b).
There have been various trials to improve the drawbacks of MTA such as setting time and handling characteristics. The idea of mixing MTA with GIC was also devised to facilitate the use of MTA. As a preliminary test, the setting time of MTA mixed with GIC was assessed and it was shorter than that of MTA. To evaluate the clinical feasibility of MTA mixed with GIC, the biocompatibility of MTA mixed with GIC was assessed in this paper.
An important decision when designing an in vitro biocompatibility study involves selecting a cell type to test. Researchers have used osteoblasts, mouse fibroblasts, human fibroblasts, and human osteosarcoma cell line.6,8,18 For this experiment the human osteosarcoma cell line (MG-63) was chosen because it is available immediately and can be cultured easily. The cell line's response with respect to cytokine production has been shown to be similar to that of human osteoblasts.8
Cytotoxicity testing is one of the most commonly used in vitro measures of biocompatibility. The method is a simple, rapid, and cost-effective biocompatibility screening test. It gives valuable indications as to which materials should be discarded and which should be subjected to further testing.6
The use of scanning electron microscopy to examine the morphology of established cell lines in the presence of dental materials as ways of assessing cytotoxicity have been described before.8,20,23 Adhesion and spreading of cells on a material surface are the initial phase for cellular function. The persistence of round cells with little or no spreading suggests the surface material may be toxic.20 This study found human osteosarcoma cells have a favorable response to MTA, GIC, and MTA mixed with GIC, compared with IRM and SuperEBA. The results of this study are in accordance with the previous in vitro studies on MTA.8,20
Using the extracts of the root end filling materials is useful for toxicity screening in vitro.6 It offers the advantages of being easily sterilized by filtration and the ability to examine the effect of materials on cells that are both distant to and in contact with them. The in vitro extract testing simulates the immediate postsurgical periradicular environment in which toxic elements of the root end filling materials might leach into the surrounding fluids in the bony crypt because the root end filling material is in contact with the osseous tissue.6
A colorimetric method based on the tetrazolium salt was first described by Scudiero in 198824 and widely used in cell viability assay.6,18,19 In the present study, the toxicity assay was used to measure mitochondrial dehydrogenase activity, as shown by the cleavage of XTT to a formazan dye. The reaction only occurs in living, metabolically active cells.6 In the XTT assay of this study, MTA mixed with GIC presented similar cell viability as MTA or GIC. Low toxicity of MTA and GIC has been already well documented.3,6,7,14,15
Research on the biocompatibility of GICs in conventional and surgical endodontics exhibit good biocompatibility for three main reasons: (i) they set with minimal exotherm; (ii) neutralization is generally sufficiently rapid that any potential irritation because of the presence of free acid is minimal; and (iii) the substances leached from the set cement are generally either benign or beneficial to the tissue in which the cement is placed.15 Good biocompatibility of GIC is also presented in the result of this study. SEM observation showed cells on the surface of GIC were elongated and dense (Figure 1e). XTT assay exhibited the cell viability of GIC group was not significantly different from that of MTA and control group (Table 2).
IRM is zinc oxide eugenol cement reinforced by addition of 20% polymethacylate. SuperEBA is zinc oxide eugenol cement modified with ethoxybenzoic acid to alter the setting time and increase the strength of the mixture. The zinc oxide eugenol cements are generally inclined to cause inflammatory reactions in the tissues, mainly due to the presence of free eugenol. Both eugenol-containing cement induce mild to moderate toxicity when they are freshly mixed, probably because of the eugenol component. 8 In this study, SEM observation showed cells on the surface of IRM and SuperEBA were round in shape and the numbers and the density of the cells were much smaller than those of other groups (Figures 1f and 1g). XTT assay exhibited the cell viability of IRM and SuperEBA groups was significantly lower than that of MTA and control group (Table 2). Although cytotoxicity was presented in this study, it is already known that cytotoxicity diminishes as the cements set, and long-term inflammatory potential appears to be minimal.25
Previous study also used IRM as a comparative material because it has been widely used in recent years as a root-end filling material.8 The tissue response was characterized by marked rounding of the cells and depletion of cell numbers, indicating that IRM was toxic. These results are in agreement with those found in the present study.
Various authors have suggested the properties for an ideal retrofilling material. These suggestions can be reduced to a list of 3 critical elements: (1) biocompatibility, (2) apical sealability, and (3) handling properties.23 Although MTA mixed with GIC showed good biocompatibility in this study, further studies on sealing ability, physical and chemical properties are required for its clinical use.
The purpose of this study was to evaluate the biocompatibility of MTA mixed with GIC and to compare it with that of MTA, GIC, IRM, and SuperEBA. To assess the biocompatibility, SEM observation and XTT assay were performed.
The SEM revealed that elongated, dense, and almost confluent cells were observed in the cultures of MTA mixed with GIC, MTA and GIC. On the contrary, cells on the surface of IRM or SuperEBA were round in shape and the number of the cells were smaller.
In XTT assay, cell viability of MTA mixed with GIC group was similar to that of MTA or GIC at all time points. IRM and SuperEBA showed significantly lower cell viability than other groups at all time points (p< 0.05).
In this research MTA mixed with GIC showed similar cellular responses as MTA and GIC. It suggests that MTA mixed with GIC has good biocompatibility like MTA and GIC.
Figures and Tables
 | Figure 1Cells after the incubation for 1 day (×1,000). a, 1 : 1 group; b, 2 : 1 group; c 1 : 2 group; d, MTA; e, GIC; f, IRM; g, SuperEBA. MTA, mineral trioxide aggregate; GIC, glass ionomer cement. |
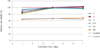 | Figure 2Relative viability of cells exposed to 1-day extracts. MTA, mineral trioxide aggregate; GIC, glass ionomer cement. |
References
1. Koulaouzidou EA, Economides N, Beltes P, Geromichalos G, Papazisis K. In vitro evaluation of the cytotoxicity of ProRoot MTA and MTA Angelus. J Oral Sci. 2008. 50:397–402.

2. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995. 21:349–353.

3. Bodrumlu E. Biocompatibility of retrograde root filling materials: a review. Aust Endod J. 2008. 34:30–35.

4. Torabinejad M, Hong CU, Pitt Ford TR, Kettering JD. Cytotoxicity of four root end filling materials. J Endod. 1995. 21:489–492.

5. Kwon JY, Lim SS, Baek SH, Bae KS, Kang MH, Lee WC. The Effect of Mineral Trioxide Aggregate on the Production of Growth Factors and Cytokine by Human Periodontal Ligament Fibroblasts. J Korean Acad Conserv Dent. 2007. 32:191–197.

6. Huang TH, Yang CC, Ding SJ, Yan M, Chou MY, Kao CT. Biocompatibility of human osteosarcoma cells to root end filling materials. J Biomed Mater Res B Appl Biomater. 2005. 72:140–145.

7. Kang MK, Bae IH, Koh JT, Hwang YC, Hwang IN, Oh WM. Comparison of Biocompatibility of Four Root perforation repair Materials. J Korean Acad Conserv Dent. 2009. 34:192–198.

8. Koh ET, McDonald F, Pitt Ford TR, Torabinejad M. Cellular response to Mineral Trioxide Aggregate. J Endod. 1998. 24:543–547.

9. Yun YR, Yang IS, Hwang YC, Hwang IN, Choi HR, Yoon SJ, Kim SH, Oh WM. Pulp response of Mineral trioxide aggregate, calcium sulfate or calcium hydroxide. J Korean Acad Conserv Dent. 2007. 32:95–101.

10. Torabinejad M, Hong CU, Lee SJ, Monsef M, Pitt Ford TR. Investigation of mineral trioxide aggregate for root-end filling in dogs. J Endod. 1995. 21:603–608.

11. Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod. 1997. 23:225–228.

12. Koh ET, Torabinejad M, Pitt Ford TR, Brady K, McDonald F. Mineral trioxide aggregate stimulates a biological response in human osteoblasts. J Biomed Mater Res. 1997. 37:432–439.

13. Koh ET, McDonald F, Pitt Ford TR, Torabinejad M. Cellular response to Mineral Trioxide Aggregate. J Endod. 1998. 24:543–547.

14. Schwartz RS, Mauger M, Clement DJ, Walker WA 3rd. Mineral trioxide aggregate: a new material for endodontics. J Am Dent Assoc. 1999. 130:967–975.

15. De Bruyne MA, De Moor RJ. The use of glass ionomer cements in both conventional and surgical endodontics. Int Endod J. 2004. 37:91–104.

16. de Souza Costa CA, Hebling J, Garcia-Godoy F, Hanks CT. In vitro cytotoxicity of glass-ionomer cements. Biomaterials. 2003. 24:3853–3858.
17. Holland R, Mazuqueli L, de Souza V, Murata SS, Dezan Júnior E, Suzuki P. Influence of the type of vehicle and limit of obturation on apical and periapical tissue response in dogs' teeth after root canal fillingwith mineral trioxide aggregate. J Endod. 2007. 33:693–693.
18. Karimjee CK, Koka S, Rallis DM, Gound TG. Cellular toxicity of mineral trioxide aggregate mixed with an alternative delivery vehicle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006. 102:e115–e120.

19. Jafarnia B, Jiang J, He J, Wang YH, Safavi KE, Zhu Q. Evaluation of cytotoxicity of MTA employing various additives. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 107:739–744.

20. Zhu Q, Haglund R, Safavi KE, Spangberg LS. Adhesion of human osteoblasts on root-end filling materials. J Endod. 2000. 26:404–406.

21. Gandolfi MG, Perut F, Ciapetti G, Mongiorgi R, Prati C. New Portland cement-based materials for endodontics mixed with articaine solution: a study of cellular response. J Endod. 2008. 34:39–44.

22. Liu HC, Lee IC, Wang JH, Yang SH, Young TH. Preparation of PLLA membranes with different morphologies for culture of MG-63 Cells. Biomaterials. 2004. 25:4047–4056.

23. Al-Sabek F, Shostad S, Kirkwood KL. Preferential attachment of human gingival fibroblasts to the resin ionomer Geristore. J Endod. 2005. 31:205–208.

24. Scudiero DA, Shoemaker RH, Paull KD, Monks A, Tierney S, Nofziger TH, Currens MJ, Seniff D, Boyd MR. Evaluation of a soluble tetrazolium/formazan assay for cell growth and drug sensitivity in culture using human and other tumor cell lines. Cancer Res. 1988. 48:4827–4833.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download