Abstract
The purpose of this study was to compare the sealing abilities of four endodontic temporary restorative materials using a methylene blue dye penetration test under dynamic loading. Standardized access cavities were prepared in forty-four intact human permanent molar teeth, and the cavities were restored with Caviton, MD-Temp, IRM, or ZOE. After thermocycling, an intermittent load of 98 N at 1 Hz was applied for 1,000 cycles to the long axis of the functional cusp of each of the teeth, which were immersed in a 1% methylene blue solution. The teeth were split in half, and the linear depth of dye penetration was evaluated according to the criteria. The results were analyzed using one-way ANOVA (p = 0.05) and Duncan's multiple range test. The results demonstrated that Caviton and MD-Temp showed significantly lower microleakage than IRM and ZOE. It was concluded that Caviton and MD-Temp exhibited better sealing ability than IRM and ZOE under dynamic loading.
During endodontic treatment, it is important to create a fluid-tight seal in the access cavity in order to prevent marginal leakage and the ingress of oral fluids and microorganisms into the root canal1). Nevertheless, temporary filling materials have received less attention than materials used for a permanent and prolonged use. However, they are an essential link in the chain that leads to disinfecting and preventing contamination or recontamination of the root canals2).
Numerous methods have been described to determine the sealing ability of endodontic temporary restorative materials. Beside dye penetration tests, autoradiography3), electrochemical methods4), fluid filtration techniques5), and bacterial penetration tests6) have been applied to determine microleakage. Among these methods, dye penetration tests are the most popular method for studying microleakage because they are easy to conduct. In most of the previous studies regarding microleakage, specimens were placed in a dye solution after a thermal or mechanical load was applied7-9). Jung et al.10) reported a new method called "dynamic loading," which evaluated the microleakage while the specimens were placed in a dye solution under mechanical loading. However, to our knowledge, there has been no microleakage study for endodontic temporary materials using dynamic loading.
The purpose of this study was to compare the sealing abilities of four endodontic temporary restorative materials using a methylene blue dye penetration test under dynamic loading.
Forty-four intact, freshly extracted maxillary and mandibular posterior human teeth were used. Immediately after extraction, all of the teeth were kept in a 0.9% sodium chloride solution (Travenol Laboratories Inc., Deerfield, IL, USA) to avoid dehydration.
4-mm × 4-mm standardized access cavities were prepared under water spray using a #4 round carbide bur at high-speed and then defined to the designed occlusal outline with an Endo Z bur (Dentsply-Maillefer, Ballaigues, Switzerland). All access preparations were made by the same operator. A periodontal probe was used to measure the depth of the opening to ensure that it could accommodate at least 4 mm of the temporary filling material11).
The teeth were randomly divided into six groups, four experimental and two control groups. Each experimental group consisted of 10 molar teeth, and each control group consisted of 2 molar teeth. Group 1 teeth were restored with Caviton (GC, Tokyo, Japan). Group 2 teeth were restored with MD-Temp (Meta-biomed, Cheongju, Korea). Group 3 teeth were restored with reinforced zinc oxide eugenol cement (IRM; Dentsply-Caulk, Milford, DE, USA). The powder-to-liquid ratio used was 4 g/mL, which has previously been shown to provide the optimal mix for this material12). Group 4 teeth were restored with zinc oxide and eugenol cement (ZOE; Sultan, Englewood, NJ, USA) with the same consistency (4 g/mL) as group 3. The control group teeth were restored with thermal plasticized gutta-percha, with the same technique as that used for the experimental groups. They were further divided into positive and negative control groups.
Thereafter, all specimens were immediately stored at 37℃ and 100% humidity for 1 day to ensure complete setting of the temporary filling materials. The teeth were thermocycled (500 cycles 5℃/60℃ for 60s each, Tauchbad No.10, 3M ESPE, Seefeld, Germany). The specimens were air dried and the teeth in the negative control group were covered with two layers of nail varnish. The teeth in the experimental groups and in the positive control group were coated with two layers of nail varnish, except for 1 mm around the tooth-restoration interface.
Root surfaces were then covered with a 0.2-mm-thick heat-resistant poly-tetrafluoroethylene adhesive tape (Nitoflon; Nitto Denko Corp, Fukaya, Japan) to simulate the periodontal ligament and to resist the heat generated during the polymerization of the embedding resin. Subsequently, the specimen roots were embedded using auto-polymerizing acrylic resin (Ortho-jet acrylic; Lang Dental Mfg, Wheeling, IL, USA) in a polytetrafluoroethylene mold with an internal diameter of 25 mm and a height of 20 mm. Then, the specimens were then placed in the Cyclic Loading Machine (WONCLMC-04-1; Won Engineering, Iksan, Korea), which had the chamber filled with 1% methylene blue solution (Figure 1). Since the average number of chewing strokes on one side is about 1,000 strokes per day13) and the loads on mandibular molars varied between 70.6 and 146 N14,15), a load of 98 N at 1 Hz was applied for 1,000 cycles to the long axis of the functional cusp of each tooth.
All of the specimens were sectioned mesio-distally through their longitudinal axis with a diamond saw (RB 205 Metsaw; R&B Inc, Daejeon, Korea), and the linear depth of the dye penetration was evaluated according to the criteria presented in Figure 2. One-way ANOVA (p = 0.05) and Duncan's multiple range tests were used for statistical analysis.
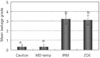
The mean microleakage values for each group are presented Figure 3. No samples were lost during the study. The positive control teeth showed 100% staining with methylene blue from the most coronal point of the access cavities to the most apical location of the access. The negative control group teeth did not show any sign of coronal microleakage.
The microleakage values indicated significant differences among the materials. Caviton and MD-temp presented the least microleakage, followed by ZOE and IRM. Caviton and MD-temp showed a mean leakage grade of 0.30, and IRM had the highest mean leakage grade of 3.20. ZOE revealed a mean leakage grade of 3.10. In addition, dye penetration into the filling material was noted in the MD-temp group (Figure 4).
There were statistically significant differences in coronal leakage between the groups (p < 0.05). Groups 1 and 2 showed significantly lower microleakage than groups 3 and 4 (Figure 3).
The use of temporary restorative materials between appointments is one of the factors that determine the success or failure of root canal treatment. These materials serve to seal the tooth temporarily, preventing the entry of fluids, microorganisms, and other debris into the root canal space9).
The results of this in vitro study indicated that Caviton and MD-Temp provided a better coronal marginal seal in standardized access preparations than did IRM and ZOE. Caviton and MD-Temp are known as premixed temporary filling materials similar to Cavit, which is the most widely used temporary restoration in the USA16). They contain zinc oxide, calcium sulfate, zinc sulfate, glycol acetate, polyvinylacetate resins, polyvinyl chloride acetate, triethanolamine, and pigments. IRM is a zinc oxide-eugenol cement reinforced with polymethyl methacrylate. Caviton and MD-temp are hygroscopic materials that exhibit linear expansion, which results from water absorption in setting. This expansion is almost double that of ZOE17) and could enhance the contact between the material and the access cavity, resulting in an improvement in the seal. Another reason for the higher performance might be related to the fact that the material is premixed, which could reduce any inconsistencies related to chair side mixing. IRM and ZOE showed the lowest coronal seal, and the inabilities of these materials to prevent microleakage have been reported. The poor sealing abilities of IRM and ZOE may be linked to the fact that a powder and liquid have to be mixed together to produce the paste to be inserted, which could cause a reduced homogeneity.
In this study, MD-Temp exhibited penetration of the dye into the filling material. A similar finding was noted in previous studies18,19). This was due to a property of the hygroscopic material, which tends to absorb fluids. However, this was not observed in the case of Caviton. This result indicates that Caviton has a better property in terms of preventing the penetration of fluids into the material itself.
Most clinicians placed a cotton pellet for ease of removal and location of the chamber before final restoration16). The wicking effect of cotton, however, may enhance coronal leakage. In this respect, the temporary filling materials were introduced into the access cavity from the bottom up without any intervening material. In this study, however, the thickness of filling materials was not standardized, and this might affect the results.
The present study utilized a dynamic loading procedure to simulate intraoral conditions. In this study, the specimens were placed in a dye solution under dynamic loading, under which microleakage could be directly influenced by the mechanical properties of the temporary materials. To our knowledge, no previous studies have measured microleakage in teeth restored with temporary filling materials while subjected to dynamic loading, an important experimental design consideration for microleakage studies.
Collectively, Caviton and MD-Temp were found to exhibit a better sealing ability than IRM and ZOE under dynamic loading. Additional studies may be needed to verify the quality of the seal provided by these materials for prolonged periods.
Figures and Tables
Figure 2
Grade of dye penetration: 1, Dye penetration within DEJ; 2, Dye penetration within half of the pulp chamber; 3, Dye penetration over half of the pulp chamber; 4, Dye penetration over the pulp chamber.

References
1. Noguera AP, McDonald NJ. A comparative in vitro coronal microleakage study of new endodontic restorative materials. J Endod. 1990. 16:523–527.

2. Saunders WP, Saunders EM. Coronal leakage as a cause of failure in root canal therapy: a review. Endod Dent Traumatol. 1994. 10:105–108.
3. Delivanis PD, Chapman KA. Comparison and reliability of techniques for measuring leakage and marginal penetration. Oral Surg Oral Med Oral Pathol. 1982. 53:410–416.

4. Jacquot BM, Panighi MM, Steinmetz P, G'sell C. Evaluation of temporary restorations'microleakage by means of electrochemical impedance measurements. J Endod. 1996. 22:586–589.

5. Anderson RW, Powell BJ, Pashley DH. Microleakage of temporary restorations in complex endodontic access preparation. J Endod. 1989. 15:526–529.

6. Krakow AA, de Stoppelaar JD, Gron P. In vivo study of temporary filling materials used in endodontics in anterior teeth. Oral Surg Oral Med Oral Pathol. 1977. 43:615–620.

7. Mayer T, Eickholz P. Microleakage of temporary restorations after thermocycling and mechanical loading. J Endod. 1997. 23:320–322.

8. Liberman R, Ben-Amar A, Frayberg E, Abramovitz I, Metzger Z. Effect of repeated vertical loads on microleakage of IRM and calcium sulfate-based temporary fillings. J Endod. 2001. 27:724–729.

9. Cruz EV, Shigetani Y, Ishikawa K, Kota K, Iwaku M, Goodis HE. A laboratory study of coronal microleakage using four temporary restorative materials. Int Endod J. 2002. 35:315–320.

10. Jung SH, Min KS, Chang HS, Park SD, Kwon SN, Bae JM. Microleakage and fracture pat terns of teeth restored with different posts under dynamic loading. J Prosthet Dent. 2007. 98:270–276.

11. Webber RT, del Rio CE, Brady JM, Segall RO. Sealing quality of a temporary filling material. Oral Surg Oral Med Oral Pathol. 1978. 46:123–130.

12. Anderson RW, Powell BJ, Pashley DH. Microleakage of three temporary endodontic restorations. J Endod. 1988. 14:497–501.

13. Graf H. Bruxim. Dent Clin North Am. 1969. 13:659–665.
14. Anderson DJ. Measurements of stress in mastication 1. J Dent Res. 1956. 35:664–670.
15. Anderson DJ. Measurements of stress in mastication 2. J Dent Res. 1956. 35:671–673.
16. Vail MM, Steffel CL. Preference of temporary restorations and spacers: a survey of Diplomates of the American Board of Endodontists. J Endod. 2006. 32:513–515.

17. Widerman FH, Eames WB, Serene TP. The physical and biologic properties of Cavit. J Am Dent Assoc. 1971. 82:378–382.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download