Abstract
The objective of this in situ study was to evaluate the effects of whitening strip (Claren, LG Household & Health Care Ltd, 2.6% hydrogen peroxide) and gel (Opalescence, Ultradent, 10% carbamide peroxide) on microhardness of enamel in comparison with untreated control. Extracted twenty human upper incisors were disinfected, cleaned, and labial side of each incisor sectioned into 3 fragments by 2 × 2 mm size. After sectioning, labial sides of fragments were flattened and fixed to orthodontic bracket using flowable composite resin. Specimens prepared from each tooth were attached to the labial side of upper incisors of twenty volunteers one by one and treated by three different methods: (1) untreated control (2) treated with whitening strip for 14 days (3) treated with whitening gel for 14 days.
Microhardness (Microhardness tester, Zwick) of each specimen was measured at the baseline of pre-treatment, immediate after bleaching treatment, 14 days after bleaching treatment and Knoop Hardness Number was determined. Microhardness changes of experimental groups were compared.
The results show that tooth whitening strip and gel used in this study does not effect the micro-hardness of enamel during bleaching procedure.
The demand for conservative esthetic dentistry has dramatically grown and so has the rapid development of new non-restorative treatments for discolored teeth1). Nightguard vital bleaching has become one of the most frequently used treatment modality for improving the esthetic appearance of teeth, primarily because of its relative ease of application, the safety of 10% carbamide peroxide bleaching materials, reduced patient chair time, lower cost, and high percentage of success2). The recent development of a strip-based system allows for vital tooth bleaching without fabrication of a custom tray. Applied directly to the tooth surface, this thin, flexible polyethylene strip coated with a hydrogen peroxide bleaching gel may afford some in-use advantages relative to tray-based systems3).
Carbamide peroxide is usually used at a concentration of 10% to 15% in dental bleaching. 10% carbamide peroxide is equivalent in strength to 3% hydrogen peroxide. The hydrogen peroxide, because of its instability and ease of decomposition into water and oxygen, penetrates through the pores of enamel and dentin to provide the lightening of the teeth. Bleaching agents affect the lightening of tooth structure through decomposition of peroxides into free radicals. The free radicals break down large pigmented molecules in enamel and dentin into smaller, less pigmented molecules4). If a prolonged contact time is spent, protein matrix of enamel and dentin might be broken. Therefore, one possible side-effect of bleaching products is that the enamel and dentin may be weakened by oxidation of the organic or inorganic elements4).
Whitening strips are being used more and more commonly at home. However, there was no previous studies on side-effects to enamel bleached with commercially available whitening strips.
The purpose of this in situ study was to evaluate the effects of whitening strip and gel on the microhardness of enamel in comparison with untreated control in situ.
Commercially avaliable whitening strip and bleaching gel were used in this study: Claren dental whitening solution (LG Household & Health Care, Seoul, Korea) and Opalescence tooth whitening gel (Ultradent Product Inc, South Jordan, USA). Claren dental whitening solution is strip type and has the hydrogen peroxide at the concentration of 2.6%. The Opalescence bleaching gel used in nightguard bleaching is composed of 10% carbamide peroxide with carbopol.
The volunteers were 20 adults (15 males and 5 females) from 24 to 35 years of age. Each volunteer was informed of the objectives, benefits and possible risks involved in this experiment and participated only after providing written formal consent of Institutional Review Board of Kangnung National University Dental Hospital. Exclusion criteria for participating in this study were who has fixed or removable dentures or orthodontic appliances, pregnant or nursing women, smokers and had dentin sensitivity. All volunteers were used same tooth brush & toothpastes for experimental period.
We used freshly extracted twenty upper incisors containing no apparent evidence of cracks, restorations, fracture, cervical abrasion and caries for this study. Teeth were disinfected, cleaned, and labial side of each incisor sectioned into 3 fragments by 2 × 2 mm size using precision cutting device (Acutom P-50, Struers, Copenhagen, Denmark). After sectioning, the labial sides of fragments were flattened and fixed to orthodontic bracket using flowable composite resin (FiltekFlow, 3M ESPE, St. Paul, USA) and stored in distilled water until used. Before fixed to orthodontic brackets, specimens were examined under surgical microscope (OPMI, Carl Zeiss, GmbH, Germany) for checking cracks or fractures
of enamel.
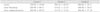
Three orthodontic brackets with a dental fragment from one tooth were randomly fixed to the central labial surface of the maxillary incisors using Glass ionomer luting cement (Rely-X luting, 3M ESPE, St. Paul, USA). Bleaching gel group (Group C) was attached to the maxillary right central incisor, control group (Group G) to the maxillary right lateral incisor, bleaching strip group (Group S) to the maxillary left central incisor (Table 1).
Orthodontic brackets were blocked out using utility wax for reservoir of bleaching gel. And then impressions were taken with alginate and stone cast models were made. Mouthguard trays were fabricated for each volunteer in a vacuum-forming machine using a flexible ethyl vinyl acetate polymer that was 0.4 mm thick. Bleaching was performed for 2 hours per day for 14 days using fabricated custom tray.
Microhardness test was performed using a Hardness testing machine (Microhardness tester, Zwick, Ulm, Germany) and TestXpert program (Zwick, Ulm, Germany). Three indentations on each specimen were made with a load of 300 g for 25 seconds dwell times.
Microhardness were measured at three different periods.
Microhardness measurement were performed before brackets were attached to volunteers.
Microhardness changes were statistically analyzed and compared between groups using Repeated measure of ANOVA and Scheffe post-hoc test at the 95% level of confidence. One way-ANOVA and Scheffe post-hoc test was used to compare differences for degree of microhardness change between groups at the 95% confidence level.
The mean values and standard deviations of experimental groups at initial, after bleaching and after remineralization are shown in Table 2. Although the mean microhardness values for all groups were increased after 14 days, they decreased after remineralization (Figure 1). There was no difference in the microhardness between experimental groups at all measurement time.
Table 3 shows that the mean and standard deviations of the changes in the microhardness (After bleaching-initial, after remineralization-after bleaching) of experimental groups. There was no difference between experimental groups.
Currently, the general population relates modern dentistry to improved facial aesthetics, health, and social success. A lighter dentition is associated with health, youth, and vigor. A recent survey of American women showed that 55% of those between 34 and 55 years would have their teeth whitened or straightened to create a more youthful appearance5). Tooth whitening is now the most commonly requested elective cosmetic service in the dental office.
The recent development of a strip-based system allows for vital tooth bleaching without fabrication of a custom tray. Previous research on whitening strips had demonstrated that twice daily treatment over 14 day period resulted in a meaningful improvement in tooth color relative to baseline and placebo6). The magnitude of the benefit was similar to that achieved using a conventional 10% carbamide peroxide system in a custom tray, and superior to that seen with a 10% combination carbamide peroxide system in a stock tray7).
One of the possible side effects of bleaching products is that the enamel structure may be weakened by oxidation of the organic or inorganic elements4). Various test methods, such as SEM, AFM have been used to evaluated the changes in enamel surface during bleaching. In this study, effect to bleaching was assessed by the microhardness changes. Microhardness changes are related to a loss or gain of mineral (demineralization or remineralization) of the tooth structure8). It has been shown that the microhardness test is suitable for determining small changes in surface microhardness that demonstrate the effects of acids, acidic beverages and bleaching products on enamel9-11). Morphological characterization by SEM is a good complement to microhardness measures in offering a more complete understanding of tooth surface conditions following bleaching exposureb12).
For bleached enamel surfaces, there was a tendency of reduction of the microhardness of either bleaching agents compared to the unbleached ones13-15). However, this study indicated no statistically significant differences in microhardness changes between groups. Using similar methodology to evaluate the microhardness after 10% carbamide peroxide treatment on enamel, Justino et al16) and other investigators17-18) found similar results. Conflicting results have been obtained in studies evaluating the adverse effects of bleaching treatment. It is possible that discrepancies found in these studies can be explained by variables in methodology related to exposure time, pH of solution, type of teeth, and storage medium. In that regard, the storage medium seems to be an important factor for such variation in results. In the study of Justino et al16), difference between the in situ and in vitro condition could be attributed to the important role of human saliva in the remineralization process and while enamel slabs from the in vitro methodology were stored in deionized water, slabs from the in situ group were submitted to a clinical condition in oral appliances used four volunteers. The presence of saliva could prevent the demineralizing effect of bleaching gel in situ.
There is a correlation between the values of microhardness evaluations allowed by the dynamics of the oral cavity. Demineralization of enamel structure occurs at a critical pH of 5.519). In a pH of less than 5.5 the amount of Ca and P in saliva is lower than the solubility rate of hydroxyapatite, with enamel having a tendency to lose Ca and P to the oral environment16). When the bleaching agent causes demineralization in enamel, ionic changes are induced, increasing mineral uptake, which replaces the mineral lost during treatment. In addition to, because bleaching is a time-and dose-related treatment, it is conceivable that the effect of bleaching treatment on human enamel is directly related to the bleaching agent's concentration of peroxide and the contact time13). In this study, 10% carbamide peroxide and 2.6% hydrogen peroxide strip were used to bleaching only for 2 weeks, so it can be thought that there was relatively short bleaching period and low concentration of bleaching agent compared to other studies.
In this study, mean microhardness values for all groups increased after 14 days, where as microhardness decreased after remineralization for experimental period (Figure 1). A possible cause for this pattern might have been the storage medium used during the preparation of the enamel fragments, namely distilled and deionized water. Araujo et al18) have observed in pilot studies that when enamel is immersed in deionized water for long periods of time, microhardness values drop. A few studies have shown that demineralization enamel is more susceptible to remineralization than intact enamel20). Thus, in spite of bleaching agents having a slightly acidic pH, the solution is rapidly neutralized, which cancels its demineralization potential21). According to Leonard et al21), 10% carbamide peroxide significantly increases salivary pH during the first 15 to 20 minute interval. This saliva neutralization is apparently related to the breaking down of carbamide peroxide into urea, whereby the pH is raised. This might explain the slight increase in microhardness observed to occur in this study.
In the laboratory it is difficult to duplicate the clinical conditions completely in which bleaching treatment is conducted. Therefore, it may not be entirely possible to extrapolate the results of in vitro studies to the clinical setting. In the study of Araujo et al18), they used removable appliance to replicate closely the intraoral conditions. But several limitations and variables have to be considered. The appliances containing the enamel specimens were removed from the mouth during meals and toothbrushing. This was necessary to avoid the contact of the specimens with chemicals that could affect enamel hardness. In this study, enamel fragments were fixed on the upper incisors of 20 volunteers during experimental period except microhardness test procedure.
In this study, microhardness to enamel bleached with commercially available bleaching agents were evaluated in situ. Although the mean microhardness values for all groups increased after 14 days, where as microhardness decreased after remineralization, bleached groups did not show significant differences from untreated control group in tendency and amount of microhardness changes (p > 0.05).
Therefore, it can be stated that bleaching with whitening strips and the bleaching gel did not influence the microhardness to enamel within 14 days.
Figures and Tables
References
1. Heymann HO. Nonrestorative treatment of discolored teeth: reports from an International Symposium. J Am Dent Assoc. 1997. 128(6):710–711.
2. Haywood VB. History, safety, and effectiveness of current bleaching techniques and applications of the nightguard vital bleaching technique. Quintessence Int. 1992. 23(7):471–488.
3. Gerlach RW. Shifting paradigms in whitening: introduction of a novel system for vital tooth bleaching. Compend Contin Educ Dent Suppl. 2000. (29):S4–S9.
4. Goldstein GR, Kiremidjian-Schumacher L. Bleaching: is it safe and effective? J Prosthet Dent. 1993. 69(3):325–328.

5. Gherilyn GS, Jacinthe MP, Robert SW. Tooth-whitening modalities for pulpless and discolored teeth. Pathways of the Pulp. 2002. 8th ed. St Louis: Mosby;749–762.
6. Park DY, Jung SH, Ma DS, Chang SY, Yun SY. Randomized controlled clinical trial of the efficacy and safety of a 2.6% hydrogen peroxide containing tooth-whitening strips. J Korean Acad Dent Health. 2002. 26(3):385–396.
7. Gerlach RW, Barker ML, Sagel PA. Comparative efficacy and tolerability of two direct-to-consumer tooth whitening systems. Am J Dent. 2001. 14(5):267–272.
8. Featherstone JD, Ten Cate JM, Shariati M, Arends J. Comparison of artificial caries-like lesions by quantitative microradiography and microhardness profiles. Caries Res. 1983. 17(5):385–391.

9. Savarino L, Saponara TA, Tarabusi C, Breschi L, Prati C. Enamel microhardness after in vitro demineralization and role of different restorative materials. J Biomater Sci Polym Ed. 2002. 13(3):349–357.

10. Lussi A, Jaggi T, Scharer S. The influence of different factors on in vitro enamel erosion. Caries Res. 1993. 27(5):387–393.

11. Seghi RR, Denry I. Effects of external bleaching on indentation and abrasion characteristics of human enamel in vitro. J Dent Res. 1992. 71(6):1340–1344.

12. White DJ, Kozak KM, Zoladz JR, Duschner HJ, Gotz H. Effects of Crest Whitestrips bleaching on surface morphology and fracture susceptibility of teeth in vitro. J Clin Dent. 2003. 14(4):82–87.
13. Basting RT, Rodrigues JA, Serra MC. The effects of seven carbamide peroxide bleaching agents on enamel microhardness over time. J Am Dent Assoc. 2003. 134(10):1335–1342.

14. Rodrigues JA, Basting RT, Serra MC, Rodrigues AL. Effects of 10% carbamide peroxide bleaching materials on enamel microhardness. Am J Dent. 2001. 14(2):67–71.
15. Basting RT, Rodrigues AL, Serra MC. The effect of 10% carbamide peroxide bleaching material on microhardness of sound and demineralized enamel and dentin in situ. Oper Dent. 2001. 26(6):531–539.
16. Justino LM, Tames DR, Demarco FF. In situ and in vitro effects of bleaching with carbamide peroxide on human enamel. Oper Dent. 2004. 29(2):219–225.
17. Potocnik I, Kosec L, Gaspersic D. Effect of 10% carbamide peroxide bleaching gel on enamel microhardness, microstructure, and mineral content. J Endod. 2000. 26(4):203–206.

18. Araujo EM, Baratieri LN, Vieira LC, Ritter AV. In situ effect of 10% carbamide peroxide on microhardness of human enamel: function of time. J Esthet Restor Dent. 2003. 15(3):166–173.

19. Feagin F, Sierra O, Thiradilok S, Jeansonne B. Effects of fluoride in remineralized human surface enamel on dissolution resistance. J Dent Res. 1980. 59(6):1016–1021.

20. Pickel FD, Cort W, Starr N, Bilotti A, Pigman W. Evaluation of enamel-rehardening agents in saliva. J Dent Res. 1965. 44(5):855–859.

21. Leonard RH, Bentley CD, Haywood VB. Salivary pH changes during 10% carbamide peroxide bleaching. Quintessence Int. 1994. 25(8):547–550.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download