1. Haikel Y, Wittenmeyer W, Bateman G, Bentaleb A, Allemann C. A new method for the quantitative analysis of endodontic microleakage. J Endod. 1999. 25:172–177.

2. Jacobson SM, von Fraunhofer JA. The investigation of microleakage in root canal therapy. An electrochemical technique. Oral Surg Oral Med Oral Pathol. 1976. 42:817–823.
3. Araki K, Isaka H, Ishii T, Suda H. Excretin of
14C-formaldehyde distributed systemically through root canal following pulpectomy. Endod Dent Traumatol. 1993. 9:196–199.

4. Mittal M, Chandra S, Chandra S. Comparative tissue toxicity evaluation of four endodontic sealers. J Endod. 1995. 21:622–624.

5. Pascon EA, Leonardo MR, Safavi K, Langeland K. Tissue reaction to endodontic materials: methods, criteria, assessment, and observations. Oral Surg. 1991. 72:222–237.

6. LeGeros RZ. Calcium phosphate materials in restorative dentistry: a review. Adv Dent Res. 1988. 2:164–180.

7. Levin MP, Getter L, Adrian J, Cutright DE. Healing of periodontal defects with ceramic implants. J Clin Periodontol. 1974. 1:197–205.

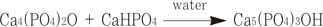
8. Brown WE, Chow LC. A new calcium phosphate setting cement. J Dent Res. 1990. 69:672.
9. Fukase Y, Eanes ED, Tagaki S, Chow LC, Brown WE. Setting reaction and compressive strength of calcium phosphate cements. J Dent Res. 1990. 69:1852–1856.

10. Gruninger SE, Siew C, Chow LC, O'Young A, Ts'AO NK, Brown WE. Evaluation of the biocompatibility of a new calcium phosphate setting cement[abstract]. J Dent Res. 1984. 63:200.
11. Hong CY, Lin SK, Kok SH, Wong MY, Hong VC. Histological reaction to a newly developed calcium phosphate cement implanted in the periapical and periodontal tissues. J Formos Med Assoc. 1990. 89:297–304.
12. Shindo ML, Costantino PD, Friedman CD, Chow LC. Facial skeletal augmentation using hydroxyapatite cement. Arch Otolaryngol Head Neck Surg. 1993. 119:185–190.

13. Matsuya Y, Antonucci JM, Matsuya S, Takagi S, Chow LC. Polymeric calcium phosphate cements derived from poly(methyl vinyl ether-maleic acid). Dent Mater. 1996. 12:2–7.

14. Sugawara A, Chow LC, Tagaki S, Chohayeb H.
In vitro evaluation of the sealing ability of a calcium phosphate cement when used as a root canal sealer-filler. J Endod. 1990. 16:162–165.

15. Sugawara A, Nishiyama M, Kusama K, Moro I, Nishimura S, Kudo I, Chow LC, Takagi S. Histopathological reactions of calcium phosphate cement. Dent Mater J. 1992. 11:11–16.

16. Chohayeb H, Chow LC, Tsaknis PJ. Evaluation of calcium phosphate as a root canal sealer-filler material. J Endod. 1987. 13:384–387.

17. Krell KF, Wefel JS. Calcium phosphate cement root canal sealer-scanning electron microscopic analysis. J Endod. 1984. 10:571–576.

18. Chau JY, Hutter JW, Mork TO, Nicoll BK. An
in vitro study of furcation perforation repair using calcium phosphate cement. J Endod. 1997. 23:588–592.

19. Kim JS, Baek SH, Bae KS.
In vivo study on the biocompatibility of newly developed calcium phosphate-based root canal sealers. J Endod. 2004. 30:708–711.

20. Beltes P, Koulaouzidou E, Kotoula V, Kortsaris AH.
In vitro evaluating of the cytotoxicity of calcium hydroxide-based root canal sealers. Endod Dent Traumatol. 1995. 11:245–249.

21. Maron DM, Ames B. Revised methods for the Salmonella mutagenicity test. Mutat Res. 1983. 113:173–215.

22. Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983. 65:55–63.

23. Matsumoto K, Inoue K, Matsumoto A. The effect of newly developed root canal sealers on rat pulp cells in primary culture. J Endod. 1989. 15:60–67.

24. Koulaouzidou EA, Papazisis KT, Beltes P, Geromichalos GD, Kortsaris AH. Cytotoxicity of three resin-based root canal sealers: an
in vitro evaluation. Endod Dent Traumatol. 1998. 14:182–185.

25. Spangberg L, Langeland K. Biologic effects of dental materials. I. Toxicity of root canal filling materials on HeLa cells in vitro. Oral Surg. 1973. 35:402–414.
26. Spangberg LS, Barosa SV, Lavigne GD. AH 26 releases formaldehyde. J Endod. 1993. 19:596–598.
27. Huang FM, Tai KW, Chou MY, Chang YC. Cytotoxicity of resin-, zinc oxide eugenol-, and calcium hydroxide-based root canal sealers on human periodontal ligament cells and permanent V79 cells. Int Endod J. 2002. 35:153–158.

28. Cohen BI, Pagnillo MK, Musikant BL, Deutsch AS. An in vitro study of the cytotoxicity of two root canal sealers. J Endod. 2000. 26:228–229.
29. Tai K, Huang F, Chang Y. Cytotoxic evaluation of root canal filling materials on primary human oral fibroblast cultures and a permanent hamster cell line. J Endod. 2001. 27:571–573.

30. Beltes P, Koulaouzidou E, Kolokuris I, Kortsaris AH.
In vitro evaluation of the cytotoxicity of two glassionomer root canal sealers. J Endod. 1997. 23:572–574.

31. Willershausen B, Briseno B, Schafer D, Schulze R. Cytotoxicity of root canal filling materials to three different human cell line. J Endod. 2000. 26:703–707.

32. Kolokuris I, Beltes P, Economides N, Vlemmas I. Experimental study of the biocompatibility of a new glass ionomer root canal sealer (Ketac Endo). J Endod. 1996. 22:395–398.

33. Briseno BM, Willershausen B. Root canal sealer cytotoxicity with human gingival fibroblast III. Calcium hydroxide-based sealers. J Endod. 1992. 18:110–111.
34. Bilginer S, Esener T, Soylemezoglu F, Tiftik AM. The investigation of biocompatibility and apical microleakage of tricalcium phosphate based root canal sealers. J Endod. 1997. 23:105–109.

35. Leyhausen G, Heil J, Reifferscheid G, Waldmann P, Gerutsen W. Genotoxicity and cytotoxicity of the epoxy resin based sealer AH Plus. J Endod. 1999. 25:109–113.
36. Segura JJ, Jmenez-Rubio A. Effect of eugenol on macropage adhesion in vivo to plastic surfaces. Endod Dent Traumatol. 1998. 14:72–74.
37. Economides N, Ioannis K. Experimental study of the biocompatibility of four root canal sealers and their influence on the zinc and calcium content of several tissues. J Endod. 1995. 21:122–127.

38. Kolokouris I, Nikolaos E.
In vivo comparison of the biocompatibility of two root canal sealers implanted into the subcutaneous connective tissue of rats. J Endod. 1998. 24:82–85.

39. Yoshikawa M, Hayami S, Tsuji I, Toda T. Histopathological study of a newly developed root canal sealer containing tetracalcium-dicalcium phosphates and 1.0% chondroitin sulfate. J Endod. 1997. 23:162–166.

40. Takechi M, Miyamoto Y, Ishikawa K, Toh T, Yuasa T, Nagayama M, Suzuki K. Initial histological evaluation of anti-washout type fast-setting calcium phosphate cement following subcutaneous implantation. Biomaterials. 1998. 19:2057–2063.

41. Wright KJ, Barbosa SV, Araki K, Spangberg LS. In vitro antimicrobial and cytotoxic effects of Kri 1 paste and zinc oxide-eugenol used in primary tooth pulpectomies. Pediatr Dent. 1994. 16:102–106.
42. Yuan H, Li Y, de Bruijn JD, de Groot K, Zhang X. Tissue responses of calcium phosphate cement: a study in dogs. Biomaterials. 2000. 21:1283–1290.

43. Miyamoto Y, Ishikawa K, Takechi M, Yuasa M, Kon M, Nagayama M, Asaoka K. Non-decay type fast-setting calcium phosphate cement: setting behaviour in calf serum and its tissue response. Biomaterials. 1996. 17:1429–1435.

44. Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR. The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J. 2005. 38:834–842.

45. Ribeiro DA, Duarte MA, Matsumoto MA, Marques ME, Salvadori DM. Biocompatibility
in vitro tests of mineral trioxide aggregate and regular and white Portland cements. J Endod. 2005. 31:605–607.

46. Saidon J, He J, Zhu Q, Safavi K, Spangberg LS. Cell and tissue reactions to mineral trioxide aggregate and Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:483–489.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download