Abstract
Objective
This study investigated the effects of additional balance training using three dimensional balance trainer on dynamic balance, gait symmetry and fall efficacy in subacute hemiplegic stroke patients.
Method
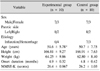
This study designed pretest-posttest control group. Twenty subacute stroke patients were randomly assigned to an experimental or a control group. All patients had conventional physical therapy. In addition, 10 patients in experimental group was trained with the three dimensional balance trainer (BalPro®) for 30 min/day, 5 day/week for 4 weeks. All participants were assessed by: Berg Balance Scale (BBS), Timed Up and Go test (TUG), gait symmetry, and Fall efficacy scale-Korea (FES-K) before and after training.
Results
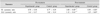
All participants of both group showed statistically significant improvements in dynamic balance, gait symmetry and fall efficacy. More improvements were shown significantly in experimental group than those in control group in BBS, TUG, step length symmetry (p<0.05) and single limb support symmetry (p<0.01).
Figures and Tables
Fig. 1
Setting for three dimentional balance trainer (TDBT). The TDBT consist of a balance board with weight bearing sensor to right or left side, conventional touch screen, tilting sensor which detects the degree of affected knee flexion and extension. A subject stands on the balance board, with performing balance training with game system. Subjects were encouraged to increase the challenge level and to try to improve their performance of each activity during the intervention duration.

Fig. 2
fomula of the gait symmetry ratio (spatial symmetry ratio, temporal symmetry ratio). SLnon paretic and paratic: Step length of non paretic side and paretic side. SLSnonparatic and paretic: Sigle limb support (% of gait cycle) of non paretic side and paretic side.

Fig. 3
Dynamic balance parameters (BBS, TUG) were assessed before intervention, after 4 weeks of intervention. During the 4 weeks, both groups showed statistically significant improvements in all parameters. BBS: Berg balance scale, TUG: timed up and go test. *p<0.05, †p<0.01.

References
1. Sharp SA, Brouwer BJ. Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Arch Phys Med Rehabil. 1997; 78:1231–1236.
2. Kelley RE, Borazanci AP. Stroke rehabilitation. Neurol Res. 2009; 31:832–840.
3. Smania N, Picelli A, Gandolfi M, Fiaschi A, Tinazzi M. Rehabilitation of sensorimotor integration deficits in balance impairment of patients with stroke hemiparesis: a before/after pilot study. Neurol Sci. 2008; 29:313–319.
4. Shumway CA, Wollacott M. Motor control: translating research into clinical practice. 3rd ed. Maryland: Lippincott Williams & Wilkins;2007. p. 157–162.
5. Kim EJ, Hwang BY, Kim JH. The effect of core strength exercises on balance and walking in patients with stroke. J Korean Soc Phys Ther. 2009; 21:17–22.
6. Yavuzer G, Eser F, Karakus D, Karaoglan B, Stam HJ. The effects of balance training on gait late after stroke: a randomized controlled trial. Clin Rehabil. 2006; 20:960–969.
7. Lee HS, Kim MC. The effect of balance task-related circuit training on chronic stroke patients. J Korean Soc Phys Ther. 2009; 21:23–30.
8. de Sèze M, Wiart L, Bon-Saint-Come A, Debelleix X, de Seze M, Joseph PA, Mazaux JM, Barat M. Rehabilitation of postural disturbances of hemiplegic patients by using trunk control retraining during exploratory exercises. Arch Phys Med Rehabil. 2001; 82:793–800.
9. Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction of balance. Suggestion from the field. Phys Ther. 1986; 66:1548–1550.
10. Byun SD, Cho DH, Choi WD, Hong YH, Lee ZI, Lee YS. Effects of the balance control training in chronic hemiplegic stroke patients. Brain Neurorehabil. 2012; 5:32–38.
11. Lee SH, Byun SD, Kim CH, Go JY, Nam HU, Huh JS, Jung TD. Feasibility and effects of newly developed balance control trainer for mobility and balance in chronic stroke patients: a randomized controlled trial. Ann Rehabil Med. 2012; 36:521–529.
12. Kwolek A, Lewicka K. Analysis of reasons for falls of hemiparetic inpatient rehabilited patients. Ortop Traumatol Rehabil. 2002; 4:606–612.
13. Bohannon RW, Tinti-Wald D. Accuracy of weightbearing estimation by stroke versus healthy subjects. Percept Mot Skills. 1991; 72:935–941.
14. Hyndman D, Ashburn A, Strack E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil. 2002; 83:165–170.
15. Botner EM, Miller WC, Eng JJ. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil Rehabil. 2005; 27:156–163.
16. Ashburn A, Hyndman D, Pickering R, Yardley L, Harris S. Predicting people with stroke at risk of falls. Age Ageing. 2008; 37:270–276.
17. Brandstater ME, de Bruin H, Gowland C, Clark BM. Hemiplegic gait: analysis of temporal variables. Arch Phys Med Rehabil. 1983; 64:583–587.
18. Patterson KK, Parafianowicz I, Danells CJ, Closson V, Verrier MC, Staines WR, Black SE, Mcllroy WE. Gait asymmetry in community-ambulating stroke survivors. Arch Phys Med Rehabil. 2008; 89:304–310.
19. Yang YR, Wang RY, Chen YC, Kao MJ. Dual-task exercise improves walking ability in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007; 88:1236–1240.
20. Patterson KK, Gage WH, Brooks D, Black SE, McIlroy WE. Evaluation of gait symmetry after stroke: a comparison of current methods and recommendations for standardization. Gait Posture. 2010; 31:241–246.
21. Pang MY, Eng JJ. Fall-related self-efficacy, not balance and mobility performance, is related to accidental falls in chronic stroke survivors with low bone mineral density. Osteoporos Int. 2008; 19:919–927.
22. Cohen H, Blatchly CA, Gombash LL. A study of the clinical test of sensory interaction and balance. Phys Ther. 1993; 73:346–351.
23. Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992; 73:1073–1080.
24. Era P, Heikkinen E, Gause-Nilsson I, Schroll M. Postural balance in elderly people: changes over a five-year follow-up and its predictive value for survival. Aging Clin Exp Res. 2002; 14:37–46.
25. Nichols DS. Balance retraining after stroke using force platform biofeedback. Phys Ther. 1997; 77:553–558.
26. Liston RA, Brouwer BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil. 1996; 77:425–430.
27. Kim WG. Effectof balance training on gait and functional activity in stroke patients. Korea University;2009. Dissertation of Master's Degree.
28. Yang DJ, Park SK, Kang JI, Lee JH, Uhm YH. Effect of computerized feedback postural training on balance and muscle activity in stroke patients. J Korean Soc Phys Ther. 2012; 24:348–354.
29. Cho KH, Lee KJ, Song CH. Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. Tohoku J Exp Med. 2012; 228:69–74.
30. Wall JC, Turnbull GI. Gait asymmetries in residual hemiplegia. Arch Phys Med Rehabil. 1986; 67:550–553.
31. Lin PY, Yang YR, Cheng SJ, Wang RY. The relation between ankle impairments and gait velocity and symmetry in people with stroke. Arch Phys Med Rehabil. 2006; 87:562–568.
32. Hsu AL, Tang PF, Jan MH. Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch Phys Med Rehabil. 2003; 84:1185–1193.
33. Teasell R, McRae M, Foley N, Bhardwaj A. The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Arch Phys Med Rehabil. 2002; 83:329–333.
34. Brunt D, Vander Linden DW, Behrman AL. The relation between limb loading and control parameters of gait initiation in persons with stroke. Arch Phys Med Rehabil. 1995; 76:627–634.
35. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990; 45:P239–P243.
36. Tsai SF, Yin JH, Tung TH, Shimada T. Falls efficacy among stroke survivors living in the community. Disabil Rehabil. 2011; 33:1785–1790.
37. Tyson SF, Hanley M, Chillala J, Selley A, Tallis RC. Balance disability after stroke. Phys Ther. 2006; 86:30–38.
38. Cheng PT, Liaw MY, Wong MK, Tang FT, Lee MY, Lin PS. The sit-to-stand movement in stroke patients and its correlation with falling. Arch Phys Med Rehabil. 1998; 79:1043–1046.
39. Ross EZ, Goodall S, Stevens A, Harris I. Time course of neuromuscular changes during running in well-trained subjects. Med Sci Sports Exerc. 2010; 42:1184–1190.
40. Lee JH, Kim SB, Lee KW, Lee JY. The effect of prolonged inpatient rehabilitation therapy in subacute stroke patients. Ann Rehabil Med. 2012; 36:16–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download