Abstract
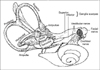
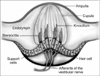
Postural balance is controlled by intricate connections between the vestibular, visual and proprioception system. Among these, the vestibular system is one of the key factors in coordinating and maintaining balance. The peripheral apparatus for the vestibular system consists of the semicircular canals, which sense head rotation; and the otoliths, which sense gravity and linear acceleration. The central vestibular pathways form a large network from the vestibular nuclei, ocular motor nuclei, integration centers in the pons and rostral midbrain, vestibulocerebellum, thalamus, to the multisensory vestibular cortex areas in the temporoparietal cortex. The most important structures for the central vestibular pathways are those mediating the vestibulo-ocular reflex (VOR), and the descending pathways into the spinal cord along the medial and lateral vestibulospinal tract which mediate postural control. The cortical structures involved in vestibular function are the parietoinsular vestibular cortex, the retroinsular cortex, the superior temporal gyrus and the inferior parietal lobule. Activation of the cortical network during vestibular stimulation is not symmetrical; dominance is stronger in the nondominant hemisphere, in the hemisphere ipsilateral to the stimulated ear and in the hemisphere ipsilateral to the slow phase of the vestibular caloric nystagmus. Disorder of the vestibular pathway, anyway along its various tracts, may result in balance and coordination impairments and lead to misperception of motion.
Figures and Tables
 | Fig. 3Diagram showing the various connections of the vestibular nuclei (modified from Lundy-Ekman 2012). |
 | Fig. 4Schematic drawing showing the neural structures involved in the vestibulo-ocular reflex (adapted from Dieterich 2007). |
 | Fig. 5Illustration showing cortical activation during vestibular stimulation. Activations in the temporo-parieto-insular areas of both sides are observed with dominance of the non-dominant right hemisphere. During vestibular stimulation, deactivations are observed in the visual cortex bilaterally (adapted from Dieterich 2010). |
References
1. Hardy M. Observations on the innervation of the macula sacculi in man. Anat Rec. 1934; 59:403–418.
2. Lim JS, Han BI. A practical approach to diagnosis and management. Dizziness. 1st ed. Korea: Purunsol;2008.
3. Schubert MC, Minor LB. Vestibulo-ocular physiology underlying vestibular hypofunction. Phys Ther. 2004; 84:373–385.
4. Dieterich M. Central vestibular disorders. J Neurol. 2007; 254:559–568.
5. Brandt T. Classification of vestibular brainstem disorders according to vestibulo-ocular reflex planes. Klin Wochenschr. 1991; 69:121–123.
6. Dieterich M, Bartenstein P, Spiegel S, Bense S, Schwaiger M, Brandt T. Thalamic infarctions cause side-specific suppression of vestibular cortex activations. Brain. 2005; 128:2052–2067.
7. Brandt T, Dieterich M. The vestibular cortex. Its locations, functions, and disorders. Ann N Y Acad Sci. 1999; 871:293–312.
8. Dieterich M, Bense S, Lutz S, Drzezga A, Stephan T, Bartenstein P, Brandt T. Dominance for vestibular cortical function in the non-dominant hemisphere. Cereb Cortex. 2003; 13:994–1007.
9. Naito Y, Tateya I, Hirano S, Inoue M, Funabiki K, Toyoda H, Ueno M, Ishizu K, Nagahama Y, Fukuyama H, Ito J. Cortical correlates of vestibulo-ocular reflex modulation: a PET study. Brain. 2003; 126:1562–1578.
10. Dieterich M, Brandt T. Imaging cortical activity after vestibular lesions. Restor Neurol Neurosci. 2010; 28:47–56.
11. Lee H. Neuro-otological aspects of cerebellar stroke syndrome. J Clin Neurol. 2009; 5:65–73.
12. Perlman HB, Kimura R, Fernandez C. Experiments on temporary obstruction of the internal auditory artery. Laryngoscope. 1959; 69:591–613.
13. Kim JS, Cho KH, Lee H. Isolated labyrinthine infarction as a harbinger of anterior inferior cerebellar artery territory infarction with normal diffusion-weighted brain MRI. J Neurol Sci. 2009; 278:82–84.
14. Kim HA, Lee H. Recent advances in central acute vestibular syndrome of a vascular cause. J Neurol Sci. 2012; 321:17–22.
15. Lee H, Kim HJ, Koo JW, Kim JS. Superior divisional vestibular paresis in anterior inferior cerebellar artery infarction. J Neurol Sci. 2009; 285:250–253.
16. Laurie Lundy-Ekman. Fundamentals for rehabilitation. Neuroscience. 4th ed. Korea: Elsevier;2012.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download